Medicinal Cannabinoids in Controlling ADHD Symptoms Among Children and Adolescents: What is the Evidence?
Hani F Ayyash1,2,3,*, Michael Ogundele4, Maissa T Dahabra5 and Majd H Ayash6
1Essex Partnership University NHS Foundation Trust, UK
2Scientific Member, British Paediatric Surveillance Unit- Royal College of Paediatrics and Child Health, UK
3Executive Member, Child and Adolescent Psychiatric Surveillance System, Royal College of Psychiatry, UK
4Bridgewater Community Healthcare NHS Foundation Trust, Halton, UK
5Department of Pharmacy, Jordanian Royal Medical Services, Amman, Jordan
6Department of Neurosurgery, Al Bashir Hospital, Amman, Jordan
Received Date: 01/08/2024; Published Date: 18/10/2024
*Corresponding author: Hani F Ayyash PhD, MMedSci, MBBS, MRCPCH, FRCPCH. Consultant Neurodevelopmental Paediatrician, Essex Partnership University NHS Foundation Trust, Essex, United Kingdom
Abstract
The diagnosis of ADHD is based on combination of one more of three core symptoms of are impulsivity, hyperactivity and inattentiveness. It is often associated with considerable impact on a child’s social, emotional and cognitive development, resulting in significant difficulties within the home, social and educational settings. Effective management of ADHD patients including medication treatment and psychoeducation requires pro-active service development, engagement of commissioning and service managers for addressing primary care involvement.
One of the commonest co-morbidities of ADHD is substance abuse and many children and young people (CYP) are suspected to use illicit drugs as self-medication.
We carried out a literature search in health databases (Medline, EMBASE, PsycINFO, AMED) using the Health Database Advanced Search (HDAS) interface with relevant keywords including ADHD, Disruptive Behaviour Disorders, Cannabinoids and Medical Marijuana.
This paper uses a narrative review to explore the current published literature about the use of medical cannabinoids (CBD) and cannabidiol (CBO) among CYP. A total of 164 relevant articles were found. After excluding duplications and other articles not meeting the criteria for the study objective, one random controlled trial, one case-controlled, five observational / cross-sectional, and one literature review were identified. 3 case reports and one related case-control study of the brain structure.
There is lack of evidence that CBO are effective in the management of ADHD and for this reason its use should be discouraged. In view of limited evidence and anecdotal suspicion of higher risk of CBD negative outcomes on the still developing brain of adolescents, greater caution should be exercised before encouraging more liberal use of CBD among this group.
It is concluded that there are limited published studies relevant to CYP compared to adult populations and all studies had multiple outcomes.
Keywords: ADHD; Cannabinoids; Cannabidiol; Child; Young people; Pharmacotherapy
Abbreviations: CBO - Cannabinoid oil; CBD – Cannabinoids; CYP - children and young people; ADHD - Attention Deficit Hyperactivity Disorder
Key Messages:
- There is lack of consistent evidence that CBO are effective in the management of ADHD and for this reason its use should be discouraged.
- In view of limited evidence and anecdotal suspicion of higher risk of CBD negative outcomes on the still developing brain of adolescents, greater caution should be exercised before encouraging more liberal use of CBD among this group.
Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is one of the most common neurobiological disorders of childhood. The three principal features of ADHD are impulsivity, hyperactivity and inattentiveness [1]. The diagnosis of ADHD is based on combination of one more of these symptoms when in excess of what is normal for age or developmental stage. It is often associated with considerable impact on a child’s social, emotional and cognitive development, resulting in significant difficulties within the home, social and educational settings [2].
The prevalence of ADHD is estimated at approximately 5% with male predominance and gender ratios reported in the range of 3:1 to 8:1 [3]. Population based studies suggest that 15% of those with childhood ADHD still meet the full diagnostic criteria for the disorder at age 25 [4].
Diagnosis of ADHD is traditionally based on subjective assessment of behaviour by clinicians and carers in different settings, but this approach is prone to biases. Recent advances in computerised Continuous Performance Task (CPT) tests have greatly improved their clinical utility as objective diagnostic aid [5]. Evidence based research has shown that Quantified Behaviour Test (QBTest) is one of the most commonly used computer-based objective assessment for children and young people (CYP) who present with ADHD worldwide [6].
Children and young people affected by neurodevelopmental, emotional, behavioural and intellectual disorders (NDEBIDs) such as Attention Deficit Hyperactivity Disorder (ADHD) and Autism Spectrum Disorder (ASD) are at increased risk of mental health difficulties such as anxiety and depression. They therefore require comprehensive and holistic services to meet their complex needs [7]. There is increasing evidence that these additional mental health risks can extend into adulthood [8].
Effective management of ADHD patients including medication treatment and psychoeducation requires active service development, engagement of commissioning and service managers for addressing primary care involvement [9]. In the UK, the outcome of parenting educational programme (APEG) that is offered to parents of children who are diagnosed with ADHD found that the provision of a group psychosocial intervention programme proved to be effective in significantly improving the knowledge and understanding of parents regarding several aspects of ADHD [10].
One of the most common problems associated with ADHD is co-occurring substance abuse. One theory posited to explain the increased risk of substance use in ADHD is that of self-medication [11]. Different motivations behind drug use have been reported. ADHD patients were more likely to use drugs to improve their mood and sleep, suggesting that drug use in ADHD could help to improve symptoms [12]. Also, as stimulant medications are the recommended first line treatment in ADHD and alongside cannabis, stimulants are one of the most common classes of drugs of abuse in ADHD [13].
The research of CBD in treatment of children with ADHD is undoubtedly controversial, but of considerable interest to clinicians working with adults with ADHD [12]. Many clinicians are aware that ADHD patients tend to report potential benefits of cannabis, and a small number of clinicians in the US have gone as far as prescribing or recommending cannabis for ADHD [14]. Furthermore, the medicinal use of cannabinoids is gaining increasing attention and currently being investigated as a treatment for schizophrenia, anxiety, epilepsy and autism [15,16].
Published evidence for the use of cannabinoid products in children and adolescents with ADHD is limited. On the other hand, many clinicians are now increasingly being asked for advice and requests for recommending CBD products for CYP with ADHD.
Methods
Literature Search
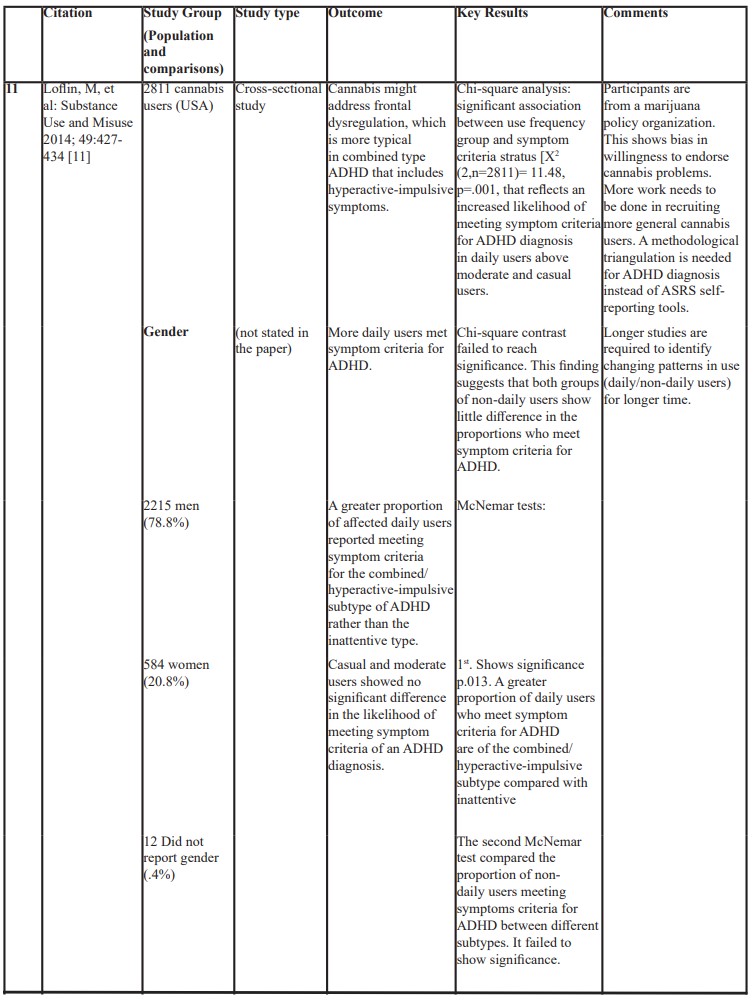
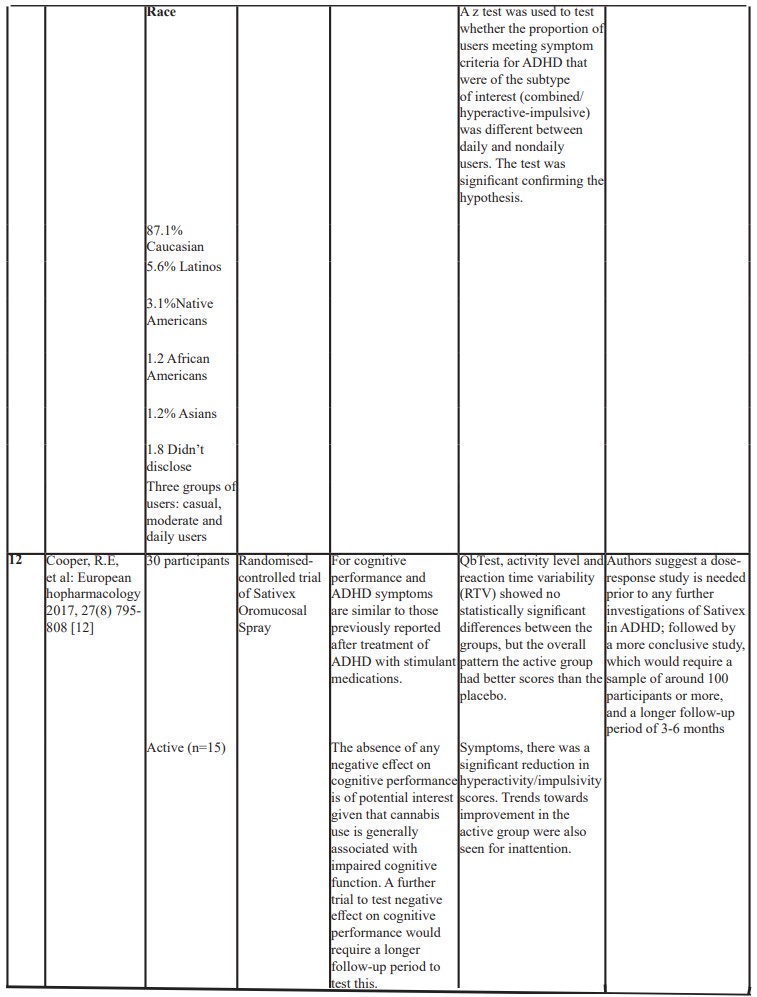
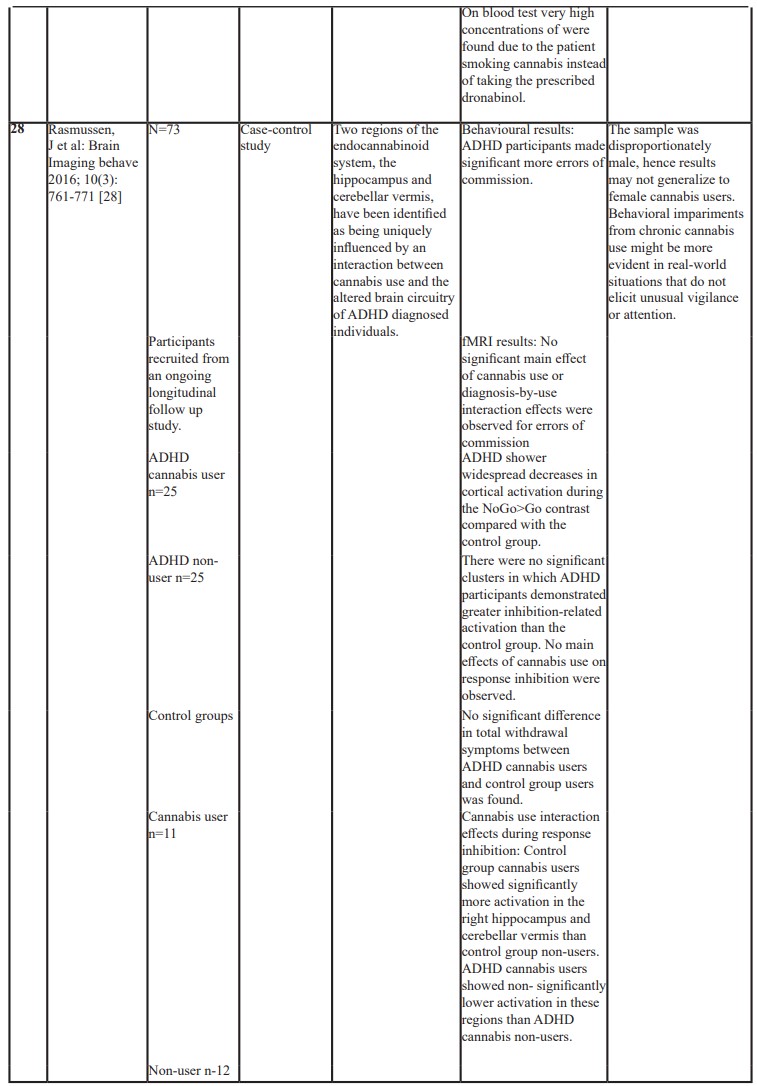
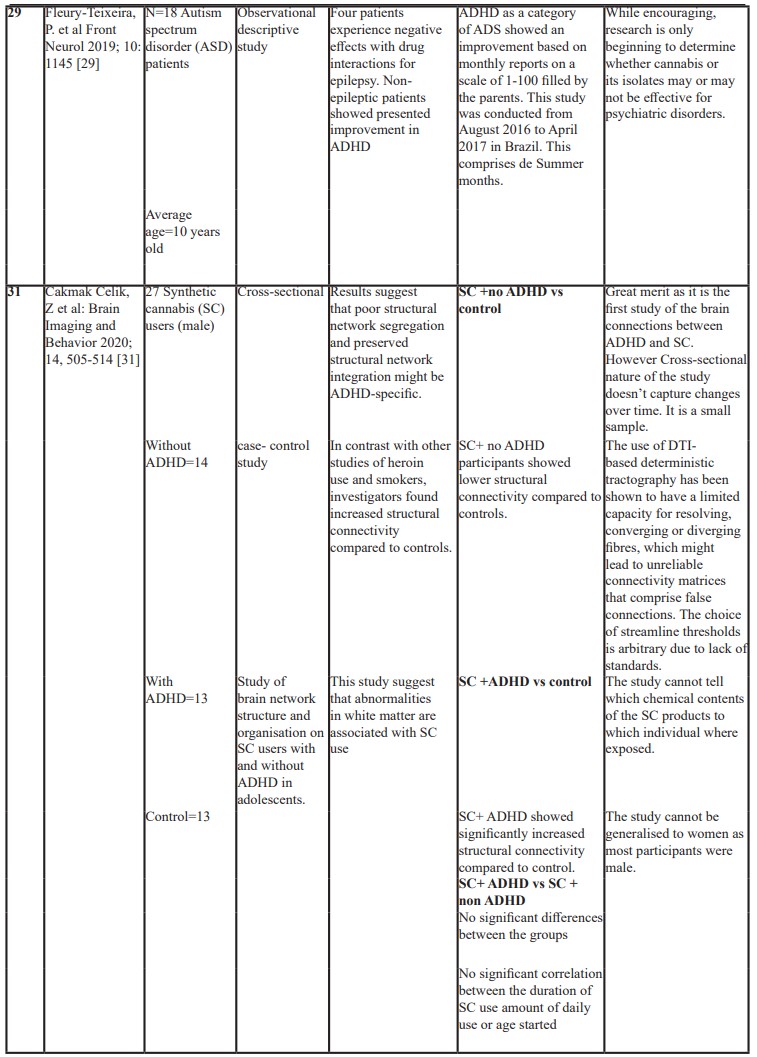
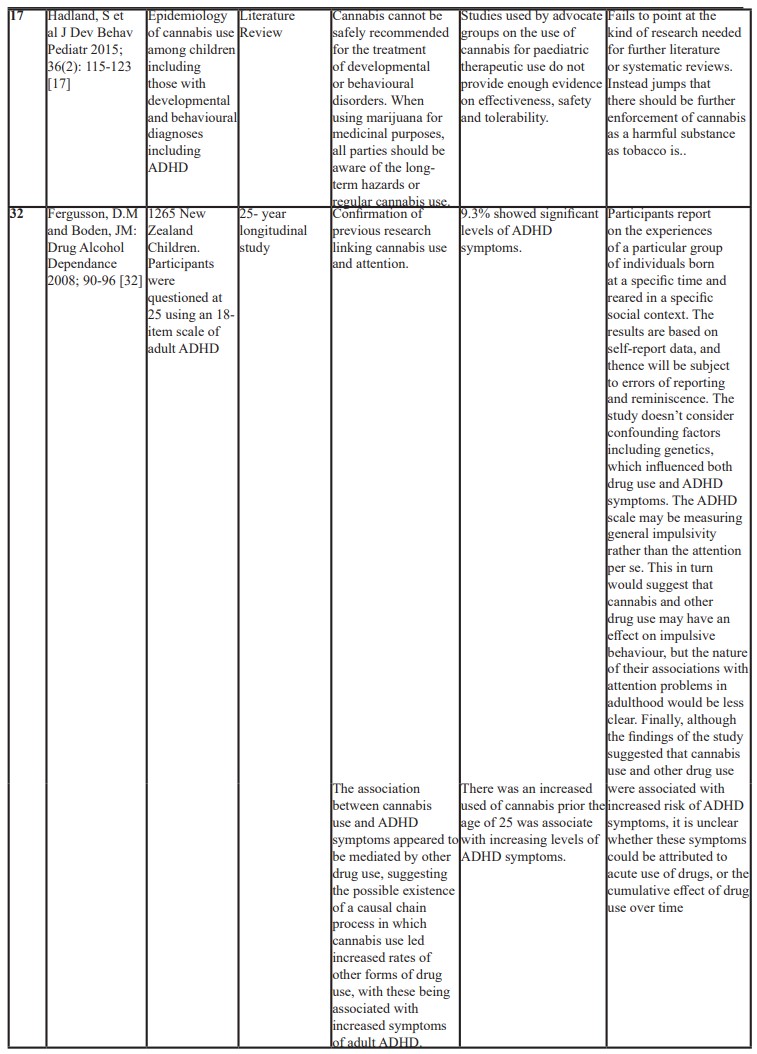
Major health databases were searched (Medline, EMBASE, PsycINFO, AMED) from inception to 2024, using the Health Database Advanced Search (HDAS) interface. Relevant keywords used included "Attention Deficit Disorder With Hyperactivity"/ OR ADHD OR "attention deficit disorder" exp "ATTENTION DEFICIT AND Disruptive Behaviour Disorders"/ exp Cannabinoids/ OR exp Cannabis/ (cannabidiol OR cannabinoid* OR CBD OR exp "Medical Marijuana"/).ti,ab "Complementary Therapies"/. "Alternative Medicine"/. No additional relevant papers were found on Cochrane database. A total of 180 relevant articles were found. After excluding duplications and other articles not meeting the criteria for the study objective, one random controlled trial, one case-controlled, five observational / cross-sectional, and one literature review were identified (Table 1). 3 case reports and one related case-control study of the brain structure are listed in the supplementary table.
Table 1: Showing a list of published studies and outcomes.


Results
Cannabis is traditionally derived from the plant Cannabis Sativa. The dried buds and accompanying leaves of cannabis are most commonly smoked, ingested and or vaped [17]. Onset of physiologic and psychologic effects vary based on route of administration, with peak effects occurring 30 minutes after inhalation and 2 to 4 hours after ingestion. Physiologic effects include tachycardia, hypertension, dry mouth and conjunctival injection. Acute effects include on the one hand relaxation, euphoria, heightened perception, sociability, sensation of time slowing, increased appetite and decreased pain, and on the other hand paranoia, anxiety, irritability, impaired short term memory, poor attention and judgement, and poor coordination and balance [18,19].
The mechanism for any potential therapeutic effects of cannabinoids (CBD) in ADHD is unknown. One possibility is that cannabinoids enhance dopaminergic transmission which is thought to be the main mechanism by which stimulants decrease ADHD symptoms and improve cognitive performance [20,21]. In addition to dopamine, the role of glutamate, GABA, and other transmitter systems need consideration, as well as N-methyl-D-aspartate and cannabinoid 2 (CB2) receptors, which has been suggested to modulate impulsivity in interaction with endocannabinoids [22-24].
Thirty eight percent (38%) of participants in a large multisite study of adolescent cannabis users met diagnostic criteria for ADHD [25]. A recent systematically review the scientific literature to characterize the effects of cannabis use on brain structure, function, and neurodevelopmental outcomes in adolescents and young adults with ADHD identified 11 studies. The limited, potentially underpowered evidence does not support the hypothesis that cannabis use has a deleterious impact on neuropsychological tasks in transitional age youth with ADHD [26].
There is only one controlled study on cannabis-based medication in ADHD. This was a formal clinical trial in the UK treating a small number of adult ADHD patients with the Satinex Oromucosal SprayR, containing a 1:1 ratio of Delta-THC to cannabidiol. The study found that despite there being no statistically significant difference in the primary outcome of cognitive performance and activity level measured by QbTest, the overall trend was that the active group (n=15) achieved better results than the placebo group (n= 15) and reported reduced hyperactivity/impulsivity symptoms as well as improved emotional lability [12]. The absence of any negative effect on cognitive performance is of potential interest given that cannabis use is generally associated with impaired cognitive function. A further trial to test negative effect on cognitive performance would require a longer follow-up period to test this. The researchers reported one serious (muscular seizures/spasms) and three mild adverse events occurred in the active group and one serious (cardiovascular problem) adverse event in the placebo group [12].
A large cross-sectional study involving 2811 adults, aged between 18- 74, all of them were cannabis users but with different regimes, showed an association between the frequent use of cannabis and the subtype of ADHD. A greater proportion of affected daily users reported meeting symptom criteria for the combined/hyperactive-impulsive subtype of ADHD rather than the inattentive type. Casual or moderate users showed no significant difference in meeting symptom criteria of an ADHD diagnosis. The authors speculated that cannabis might cause frontal dysregulation, which is more typical in combined type ADHD that includes hyperactive-impulsive symptoms [11].
In a cross-sectional questionnaire-based study on adult patients who were licensed for medical cannabis use and also were diagnosed with ADHD, it was revealed that the high dose consumption of medicinal cannabis components (phytocannabinoids and terpenes) was associated with ADHD medication reduction. In addition, the higher dosage of CBD was associated with a lower Adult ADHD Self Report Scale-ASRS)- Rating Score. No significant differences in Mental illnesses, co-morbidities were found between the low and high medicinal cannabis. It was speculated that some constitutes of the cannabis plant contribute more than others to its neurobiological effect and for this reason, ADHD patients consume MC as a substitute treatment for their conventional ADHD treatment [27].
In a longitudinal study inviting 73 participants, Functional Magnetic Resonance Imaging (fMRI) from young adults with childhood ADHD (no= 25) and without (no= 25) cannabis use was compared with a control normative comparison group (n= 11 cannabis users) and without (n=12) cannabis use was completed. ADHD participants made significantly more commission errors on NOGO trials than controls. ADHD participants also had less fronto-parietal and fronto-striatal activity, independent of cannabis use. An interaction of ADHD diagnosis and cannabis use was found in the right hippocampus and40 cerebellar vermis, with increased recruitment of these regions in cannabis-using controls during correct response inhibition. The cannabis use was associated with hippocampal and cerebral activation, areas rich in cannabinoid receptors, in local normative comparison group but not with the ADHD participants. However, the sample was disproportionately male, hence results may not generalise to female cannabis users. Hence behavioural impairments from chronic cannabis use might be more evident in real-world situations that do not elicit unusual vigilance or attention [28].
An observational descriptive study, including 18 patients with an average age 10 years old concluded that there was improvement in the symptoms of social communication and many co-morbid mental disorders in patients [; with ASD including symptoms of ADHD. Behaviour disorders, motor deficits, autonomy deficits, communication and social interaction, cognitive deficits, sleep disorders and seizures, with very infrequent and mild adverse effects such as sleepiness, irritability, diarrhoea, conjunctival hyperaemia and increased body temperature [29]. Another single case study of 6 years old boy with autism and ADHD type symptoms, was treated with daily dronabinol for six months and was noted to have improvement in hyperactivity, irritability, lethargy, stereotyped behaviours and speech , as measured by Aberrant Behavior Checklist (ABC) [30].
A cross sectional case control study of brain Network structure and organization on synthetic cannabis users with and without ADHD in adolescents. Twenty-seven cannabis users (14 without ADHD and 13 with ADHD combined type) with a history of using synthetic cannabis more than three times a week for at least 6 months prior to study enrolment were included in the study along with 13 controls. Patients were abstinent for at least 2 days before having diffusion- weighted Magnetic Resonance Imaging Scanning. The authors found that Synthetic cannabis users without ADHD had significantly weaker connectivity compared to controls in bilateral hemispheres. In contrast, synthetic cannabis users with ADHD showed stronger structural connectivity compared to controls. In addition, adolescent cannabis users with ADHD displayed reduced network organisation, suggesting that poor structural network segregation and preserved structural network integration. These results suggest that comorbidity of ADHD and substance dependence may show different structural connectivity alterations than substance use alone [31].
Literature review on the cannabis use among children including those with developmental and behaviour problems such as ADHD and ASD concluded that cannabis can’t be safely recommended for the treatment of developmental or behaviour disorders. The authors addressed those studies conducted by the advocate groups on the use of cannabis for paediatric therapeutic use do not provide enough evidence on effectiveness, safety and tolerability. It is therefore important for all parties to be aware of the long-term hazards or regular cannabis use when using marijuana for medicinal purposes [17].
A longitudinal study in New Zealand children showed a clear dose-dependent association between ADHD symptoms at age of 25 years and cannabinoid abuse. This association was found to be mediated through abuse of other substances, including Ectasy (MDMA) and methamphetamines, suggesting the possible existence of a causal chain process in which cannabis use led to increased rates of other forms of drug use, with these being associated with increased symptoms of adult ADHD [32].
In a recent observational cohort survey in the UK, it was identified that families of children with ADHD are using a wide variety of main and nonmain treatments, which are both publicly and privately funded to help with ADHD management. Nearly 70% of those surveyed reported using pharmaceutical medications, 74% had participated in a parenting class and 45% reported use of non-mainstream treatment. The most popular non-mainstream treatments used were nutrition, homoeopathy, massage and cranial osteopathy. Out of 175 families surveyed there was only one child who m ADHD symptoms were managed by cannabidiol [33].
The therapeutic use of cannabinoids for a 33 years old male with combined- type adult ADHD patient who accessed BedrocanR and BediolR for more than 5 years was described in detail. The patient reported relief for his ADHD symptoms, with reduced hyperactivity as well as improved focus, impulse control and better frustration control. Before using cannabinoids, the patient was tried for several years on several medications to Ritalin, Temazepam, Bupropion and Alprazolam but with poor results and hence he was tried on Cannabinoids [34].
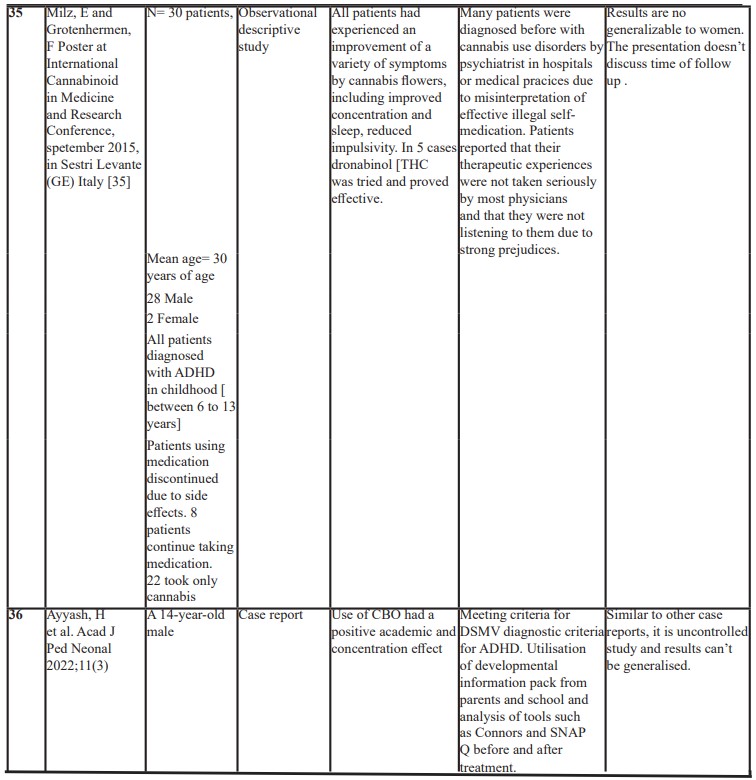
In a series of clinical cases with 30 treatment- resistant adults with ADHD, it was found that medical cannabis was helpful for a variety of symptoms, including improved concentration and sleep as well reduced impulsivity. Seventy three percent preferred to use only cannabinoids after the study, while 27% (No: 8) continued to combine CBD with other stimulant medications [35].
In a single case study of a cannabis using, 28 adult males with ADHD off stimulants, the subject’s driving skills in a simulated test during a time of abstinence improved after smoking marijuana. It was also reported that the consumption of cannabis had a positive impact on performance, behaviour and mental state of the subject. However, on blood testing, very high concentrations of cannabinoids were found in view of the patient smoking cannabis instead of taking the prescribed dronabinol [36].
On the other hand, the research on cannabinoid oil and other cannabis products as a possible intervention for ADHD does not show effectiveness for managing symptoms, but actually shows increased mental and physical health risks. There haven’t been studies on long term effects. While some people are using it and have shared their results publicly, researchers and medical professionals have not found evidence that it is an effective treatment for ADHD. The research does not show that CBO oil works for ADHD management [37].
Given the increasing prevalence of adolescent cannabis misuse and dependence as well as the growing body of literature linking cannabis use to long term and potentially irreversible adverse physical, neurocognitive, psychiatric and psychosocial outcomes, it is now more important than ever for the developmental-behaviour paediatrician to understand the available evidence on cannabis. Large professional organisations , including the American Academy of Paediatrics, The American Medical Association, the American Society of Addiction Medicine, and the American Academy of Child and Adolescent Psychiatry all have policy statements identifying marijuana use as a public health concern and currently oppose further steps toward legalisation [17].
Conclusion
There is increasing attention focused on the use of medicinal CBD in the control of ADHD symptoms and its comorbidities. Analysis of online forums where ADHD and Cannabis use was discussed found three – times as many comments advocating for the therapeutic (as opposed to harmful) effects of cannabis on ADHD. Researching medicinal cannabis and or cannabinoid oil in neurodevelopmental disorders specifically ADHD is new. There have been some case reports and few qualitative and quantitative studies but the findings in general do not see a benefit or have been inconclusive [38].
The growing interest in CBO is apparently based on the perception of its lack of harmfulness and the changing perceptions towards use of marijuana use in genera as a recreational agent. However, there have been only limited studies showing effectiveness or safety of the CBO oil or cannabis products when it comes to ADHD management, mainly in adult or young people. Furthermore, the literature shows there are harmful effects with impacts on cognitive ability, motivation, with increased mental and physical health risks. There haven’t been any studies on the use of cannabinoid oil in children; neither have there been studies on long term effects [39].
It is concluded that there are limited published studies relevant to CYP compared to adult populations and all studies had multiple outcomes. While some trials and case reports have shown some potential benefits [40], the results are not consistently confirmed in randomised controlled trials [41].
There have been single-case reports in adults with ADHD and evidence of self-medication reporting variable extent of symptom control. Cooper et al study was the only double blind randomised controlled study which was conducted in adults with small number of participants and the results can’t be generalised to children and adolescents [12]. One longitudinal cohort study from birth to age 25 showed dose-response relationship with extent of ADHD symptoms and self- medication with CBO. One study in adolescent with and without ADHD in terms of brain network Structural connectivity showed no significant effect by 6 months use of synthetic CBD. The effects on symptoms control were not examined. One narrative systematic literature review confirmed our conclusion that there is currently not enough evidence for the therapeutic use of cannabis in children and adolescents with ADHD in terms of effectiveness, safety and tolerability and for this reason it should not be recommended for treatment of ADHD.
In summary, there is lack of evidence that CBO are effective in the management of ADHD and for this reason its use should be discouraged. In view of limited evidence and anecdotal suspicion of higher risk of CBD negative outcomes on the still developing brain of adolescents, greater caution should be exercised before encouraging more liberal use of CBD among this group.
Larger and longer-term studies are needed, however, to better inform clinicians and patients as to the benefits, safety and negative impacts of cannabis use in CYP with ADHD.
Acknowledgement: We acknowledge the work of Mrs Bertha Calles Cartas (Library Research Officer) for the literature search and contribution on our first CBO published article.
References
- National Institute for Health and Care Excellence. Attention Deficit Hyperactivity Disorder: Diagnosis and management, 2018.
- Dalrymple RA, Maxwell LM, Russel S, et al. Nice guideline review: Attention deficit hyperactivity disorder: diagnosis and management (NG87). Arch Dis Child Educ Pract Ed, 2020: 105: 289-293. doi: 10.1136/archdischild-2019-316928.
- American Academy of Pediatrics (AAP). (2011). ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics, 2011; 128(5): 1007- 1022.
- Faraone S, Biederman J, Mick E. The age dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow up studies. Psychol Med, 2006; 36(2): 159-165.
- Ogundele MO, Ayyash HF, Banerjee S. Role of computerised continuous performance task tests in ADHD. Progress in Neurology and Psychiatry, 2011; 15: pp. 8-13.
- Bellato A, Hall CL, Groom MJ, Simonoff E, Thaper A, Hollis C, et al. Practitioner Review: Clinical utility of the Qb testing for the assessment and diagnosis of ADHD. A systematic review and meta-analysis. J Child Psychol Psychiatry, 2024; 65(6): 845-861. DOI:10.1111/JCPP.1390.
- Ayyash H, Ani C, Ogundele M. The role of integrated services in the care of children and young people with neurodevelopmental disorders and co-morbid mental health difficulties: An international perspective. In Book: Common Pediatric Diseases: Current Challenges, 2023. DOI:10.2174/97898815124187123020007.
- Agnew-Blais JC, et al. ‘Young adult mental health and functional outcomes among individuals with remitted, persistent and late onset ADHD’, The British Journal of Psychiatry: The Journal of Mental Sciences, 2018; 213(3): pp.526-534. doi: 10.1192/bjp.2018.97.
- Ayyash H, Sankar S, Merriman H, Vogt C, Earl T, Shah K, et al. Multidisciplinary consensus for the development of ADHD services: the way forward. Clinical Governance: An International Journal, 2013; 18(1): pp.30-38.
- Ayyash H, Ogundele M, Wisbey R, et al. The outcome of anADHD parenting grouptrainingprogramme (APEG) in the Peterborough Neurodevelopmental Services (NDS). Clin J of Nurs care Pract, 2017; 1: 013—019. DOI: 10.29328/journal.cjncp.1001002.
- Loflin M, Earleywine M, De Leo J, et al. Subtypes of attention deficit-hyperactivity disorder (ADHD) and cannabis use. Subst Use Misuse, 2014; 49: 427-434.
- Cooper RE, Williams E, Seegobin S, Tye C, Kuntsi J, Asherson P. Cannabinoids in attention-deficit/hyperactivity disorder: A randomised-controlled trial. Eur Neuropsychopharmacol, 2017; 27(8): 795-808. doi: 10.1016/j.euroneuro.2017.05.005.
- Gudjonsson Gh, Sigurdsson JF, Sigfusdottir ID, et al. An epidemiological study of ADHD symptoms among young persons and the relationship with cigarette smoking, alcohol consumption and illicit drug use. J. Child Psychol.Psychiatry Allied Discip, 2012; 53: pp 304-312. http://dx.doi.org/10.1111/j.1469-7610.2011.02489.X.
- S House of Representatives, Marijuana and Medicine, 2004. The need for a science-based approach hearing before the subcommittee on Criminal Justice, Drug Policy and Human Resources, Second Session Sess.
- Devinsky O, Cilio MR, Cross H. et al. Canabidiol: pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders. Epilepsia, 2014; 55: 791-802. http://dx.doi.org/10.1111/epi.12631.24.
- Fusar- Poli L, Cavone V, Tinacci S, et al. Cannabinoids for people with ASD: A Systematic review of published and ongoing studies. Preprints (preprints.org), 2020. http://doi: 10.20944/preprints202007.0373.v1.
- Hadland SE, Knight JR, Harris SK. Medical marijuana: review of the science and implications for developmental behavioral pediatric practice. J Dev Behav Pediatr, 2015; 36(2): 115-123.
- Winstock AR, Ford C, Witton J. Assessment and management of cannabis use disorders in primary care. BMJ, 2010; 340: c1571.
- Bramness JG, Khiabani H Z, Morland J, et al. Impairment due to cannabis and ethanol: clinical signs and addictive effects. Addiction, 2010; 105(6): 1080-1087.
- Bossong MG, Mehta MA, Van Berckel BNM, et al. Further human evidence for striatal dopamine release induced by administration of Delta 9-tetrahydrocannabinol (THC): selectivity to limbic striatum. Psychopharmacology, 2015; 232: 2723-2729. http://dx.doi.org/10.1007/s00213-015-3915-0.
- Leonard BE, McCartan D, White J, et al. Methylphenidate: a review of its neuropharmacological, neuropsychological, and adverse clinical effects. Hum. Psychopharmacol, 2004; 19: 151-180. http//:dx.doi.org/10.1002/hup.579.
- Wiskerke J, Pattij T. The cannabinoid system and impulsive behaviour. In: Fattore L, editor. Cannabinoids in neurologic and mental disease. London: Academic Press, 2015.
- Tzavara ET, Li DL, Moutsimilli L, Bisongo T, et al. Endocannabinoids activate transient receptor potential vanilloid 1 receptor to reduce hyperdopaminergia-related hyperactivity: therapeutic implications. Biol Psychiatry, 2006; 59(6): 508-515.
- Lofenetre P, Chaouloff F, Marsicano G. Bidirectional regulation of novelty- induced behavioural inhibition by the endocannabinoid system. Neuropharmacology, 2009: 57(7- 8): 715- 721.
- Dennis M, Godley SH, Diamond G, et al. The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat, 2004; 27: 197–213.
- Cawkwell PB, Hong DS, Leikauf JE. Neurodevelopmental Effects of Cannabis Use in Adolescents and Emerging Adults with ADHD: A Systematic Review. Harvard Review of Psychiatry, 2021. DOI: 10.1097/HRP.0000000000000303
- Hergenrather JY, Aviram J, Vysotski Y, et al. Cannabinoid and Terpenoid Doses are Associated with Adult ADHD Status of Medical Cannabis Patients. Rambam Maimonides Med. J,2020; 11: 1–14.13.
- Rasmussen J, Casey BJ, van Erp, TGM, et al. ADHD and cannabis use in young adults examined Using fMRI of a Go/NoGo Task. Brain Imaging Behav, 2016; 10(3): 761–771.
- Fleury-Teixeira P, Viegas Caixeta F, Cruz Ramires da Silva L, et al. Effects of CBD-enriched cannabis sativa extract on autism spectrum disorder symptoms: an observational study of 18 participants undergoing compassionate use. Neurol, 2019; 10: 1145.41.4
- Kurz R, Blaas K. Use of dronabinol (delta-9-THC) in autism. A prospective single- case-study with an early infantile autistic child. Cannabinoids, 2010; 5(4): 4-6.
- Çakmak Çelik Z, Çolak C, Di Biase MA, et al. Structural connectivity in adolescent synthetic cannabinoid users with and without ADHD. Brain Imaging and Behavior, 2019: doi:10.1007/s11682-018-0023-x.
- Fergusson DM, Boden JM. Cannabis use and adult ADHD symptoms. Drug and Alcohol Dependence, 2008; 95; 90–96.
- Fibert Ph, Relton C. What families in the UK use to manage attention deficit hyperactivity disorder (ADHD): a survey of resourse use? BMJ Paediatrics Open, 2020; 4: e000771. doi:10.1136/bmjpo-2020-000771.
- Hupli A. Medical cannabis for adult attention deficit hyperactivity disorder: sociological patient case report of cannabinoid therapeutics. Med Cannabis Cannabinoids, 2018; 1: 112–118.
- Milz E, Grotenhermen F. Successful authorised therapy of treatment resistant adult ADHD with Cannabis: experience from a medical practice with 30 patients. Poster at International Cannabinoid in Medicine and Research Conference, in Sestri Levante (GE) Italy, 2015.
- Strohbeck-Kuehner P, Skoop G, Mattern R, Cannabis improves symptoms of ADHD. Cannabinoids, 2008; 3: 1–3
- Hoffman KS. CBO oil for ADHD? What the research says, 2018.
- Mitchell Jt, Sweitzer MM, Tunno AM, et al. “I Use Weed for My ADHD”. A Qualitative Analysis of On-Line Forum Discussions on Cannabis Use and ADHD. PloSOne, 2016; 1195: e0156614.
- CHADD (John Mitchel). Children and Adults with Attention-Deficit/Hyperactivity Disorder (CHADD). CBD Oil and ADHD Management: Too Big a Leap, 2018. https://chadd.org/adhd-weekly/cbd-oil-and-adhd-management-too-big-a-leap/
- Ayyash HF, Ogundele M, Dahabra MT, Dobreva H, Cartas BC, Ayyash FF. Use of Cannabinoid Oil in a Patient with ADHD. Acad J Ped Neonatol, 2022; 11(3): 555868. DOI: 19080/AJPN.2022.11.555868.003
- Parrella NF, Hill AT, Enticott PG, Barhoun P, Bower IS, Ford TC. A systematic review of cannabidiol trials in neurodevelopmental disorders. Pharmacology Biochemistry and Behavior, 2023; 230: 173607. https://doi.org/10.1016/j.pbb.2023.173607.

