The Association Between Asthma and Endometriosis in the United States: A Retrospective Cohort Study
Marisa R Imbroane1, Hanna Kim2, Tommaso Falcone2,* and Elliott G Richards2
1Case Western Reserve University, School of Medicine, USA
2Department of Obstetrics, Gynecology and Reproductive Biology, USA
Received Date: 19/07/2024; Published Date: 14/10/2024
*Corresponding author: Tommaso Falcone, M.D., FRCSC, FACOG, FRCOG (ad eundem), Professor of Obstetrics, Gynecology and Reproductive Biology, Cleveland Clinic Lerner College of Medicine, 9500 Euclid Avenue, NA4 | Cleveland, OH 44195, USA
Abstract
Background: Data regarding the association between endometriosis and asthma has been mixed in the literature. The aim of this study was to use a data set including multiple health systems to assess the risk of diagnosis of endometriosis in patients with diagnosis of asthma.
Methods: We used the US Collaborative Network on the TriNetX research network of healthcare organizations to conduct a retrospective cohort study. Asthma and control cohorts of female patients aged 12-50 were created and stratified into age groups: 12-20, 21-30, 31-40, 41-50. The primary outcome was a diagnosis of endometriosis.
Results: The asthma cohort consisted of 1,581,644 patients, and the control cohort consisted of 23,066,153 patients. Across all age-stratified cohorts, there was an over 3-fold increased likelihood of concurrent endometriosis diagnosis (all p<0.0001) in the asthma cohort compared to the control cohort.
Conclusion: There is a clear and clinically significant association between asthma and endometriosis diagnosis in 12–50-year-old patients in the United States.
Keywords: Endometriosis; Asthma; Cohort study; Database
Introduction
An association between asthma and endometriosis is a phenomenon that has been investigated previously [1-3]. The link between these two conditions remains unclear to this day but, has been hypothesized to involve an inflammatory response from Th2 cells along with the effects of increased estrogen exposure in women with endometriosis [4-6]. However, the validity of the association has remained unclear, as other studies have documented similar rates of endometriosis in women with and without asthma [7]. A study of particular interest to the authors was previously published by Peng et al. in 2017 [2]. This retrospective cohort study out of Taiwan used a nationwide database to demonstrate the association between these two conditions in women aged 12-50. The aim of our study was to establish the relationships found in the work of Peng et al. for women in the United States using a large database of multiple health systems. We hypothesized that this association between endometriosis and asthma would also be present in our large U.S. cohort.
Materials and Methods
We conducted a retrospective cohort study utilizing the TriNetX research network on February 17, 2024. We specifically used the US Collaborative Network, consisting of 64 healthcare organizations across the United States. TriNetX has an exemption from the Western institutional review board due to the data being deidentified, complying with HIPAA. We included female patients aged 12-50 in our analysis. Our asthma cohort was defined as patients with an asthma diagnosis by ICD-10 J45. The control cohort excluded patients with this diagnosis. Our primary outcome was a concurrent diagnosis of endometriosis (ICD-10 N80). We matched cohorts for current age, race, ethnicity, female infertility (ICD-10 N97), inflammatory diseases of female pelvic organs (ICD-10 N70-77), and leiomyoma of the uterus (ICD-10 D25). We also created cohorts stratified by age, as done by Peng et al.: 12-20, 21-30, 31-40, and 41-50. Statistical testing was only completed for the age-stratified cohorts, as the database could not complete matching for the large number of patients in the overall cohort. Z-tests, logistic regression, and relative risk analysis were performed, and a p-value <0.05 was considered significant.
Results
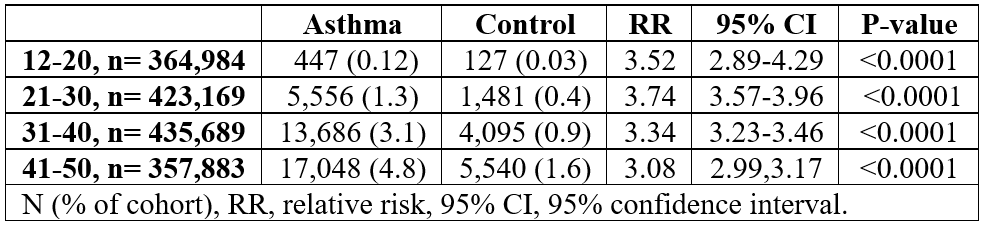
The asthma cohort consisted of 1,581,644 patients, and the control cohort consisted of 23,066,153 patients. Overall, 36,733 patients in the asthma cohort had a recorded diagnosis of endometriosis (2.3%) compared to 160,124 patients in the control cohort (0.69%). After matching, there were 364,984 patients ages 12-20; 423,169 ages 21-30; 435,689 ages 31-40; and 357,883 ages 41-50. Patients in the asthma cohort were at an increased likelihood of endometriosis compared to the control cohort across all stratifications (p all <0.0001). For 12–20 year-old, 447 in the asthma cohort had endometriosis (0.12%) compared to 127 in the control cohort (0.03%; RR 3.52, 95% CI 2.89-4.29). Similar findings were documented in the 21-30 cohort (1.3% vs 0.35%; RR 3.74, 95% CI 3.57-3.96), 31-40 cohort (3.1% vs 0.94%; RR 3.34, 95% CI 3.23,3.46) and the 41-50 cohort (4.8% vs 1.6%; RR 3.08, 95% CI 2.99,3.17) (Table 1).
Table 1: Risk of endometriosis diagnosis in asthma cohort versus control cohort.
Discussion
Using a large research database with a sample size of over 20 million female patients aged 12-50, we were able to document an association between endometriosis and asthma in the United States patient cohort. For all of our age-stratified cohorts, there was a significant increase in the likelihood for endometriosis in patients with an asthma diagnosis after matching for age, race, ethnicity, female infertility, inflammatory diseases of the female pelvis, and leiomyoma of the uterus.
Our findings support the association documented by Peng et al. in Taiwan as similar findings were seen for women in the United States [2]. Peng et al. reported a 1.5-fold increase in endometriosis for patients with asthma, whereas we found an over3-fold increase in risk across all cohorts. Possible explanations for this difference are differing environmental factors in the United States compared to Taiwan or a difference in the genetics of the population that places American women at an increased risk for both conditions. Nevertheless, a 3-fold increase in the risk of endometriosis in 12–50-year-old women with asthma is a considerable finding, much larger than this observation arising by chance alone.
A study of the CDC National Health and Nutrition Examination Survey (NHANES) database was recently conducted by Pan et al [1]. This study also documented the association of endometriosis and asthma in the United States. However, the sample size of the NHANES study was only 5,556 and only included data from 1996-2006. Our study corroborates these findings on a much larger scale and also contains patient data as recent as the day of analysis. The implications for these findings in American women can be directed to the burden the combination of these two conditions can have on quality of life. On its own, asthma, especially when uncontrolled, takes a toll on patients’ lives with the need for numerous pharmacologic interventions and even hospitalizations to control the condition, while always having an existing risk of life-threatening asthma attacks [8]. The anxiety arising from this chronic state of disease uncertainty has been linked with even worse ratings of quality of life by patients [9]. Endometriosis is also not without its own burden on quality of life. Patients with endometriosis have been found to have 0.809 quality-adjusted life years per women due to the toll of endometriosis symptoms with the decrease in quality of life being a predictor of the healthcare costs associated with the condition.10 Therefore, the association between asthma and endometriosis may indicate a common factor in the pathophysiology of these disorders, warranting further research into what this commonality could be and even into the quality of life for patients faced with the burden of both of these diagnoses.
The large sample size of our cohort is the main strength of our study, yielding large statistical power. However, it is not without its limitations. One limitation of the study is the fact the database is based on ICD-10 coding, thus relying on provider coding practices to reflect the actual diagnoses of these conditions. Another potential limitation of the study is that patients with asthma may have increased interaction with the healthcare system, increasing their likelihood of seeking out care for endometriosis-related symptoms.
Conclusion
Using a large research database of female patients aged 12-50 in the United States, we were able to document an increased risk for endometriosis in patients with an asthma diagnosis, signifying a large group of American women with a compounded burden of disease.
Declarations of interest: None
References
- Pan G, Zhang P, Li S, Cao L, Yang C. Association of endometriosis with asthma: a study of the NHANES database in 1999–2006. J Health Popul Nutr, 2024; 43: 50. doi: 10.1186/s41043-024-00541-3.
- Peng YH, Su SY, Liao WC, et al. Asthma is associated with endometriosis: A retrospective population-based cohort study. Respiratory Medicine, 2017; 132: 112-116. doi: 10.1016/j.rmed.2017.10.004.
- Sinaii N, Cleary SD, Ballweg ML, Nieman LK, Stratton P. High rates of autoimmune and endocrine disorders, fibromyalgia, chronic fatigue syndrome and atopic diseases among women with endometriosis: a survey analysis. Hum Reprod, 2002; 17(10): 2715-2724. doi: 10.1093/humrep/17.10.2715.
- Podgaec S, Abrao MS, Dias JA Jr, Rizzo LV, de Oliveira RM, Baracat EC. Endometriosis: an inflammatory disease with a Th2 immune response component. Human Reproduction, 2007; 22(5): 1373-1379. doi: 10.1093/humrep/del516.
- Truyen E, Coteur L, Dilissen E, et al. Evaluation of airway inflammation by quantitative Th1/Th2 cytokine mRNA measurement in sputum of asthma patients. Thorax, 2006; 61(3): 202-208. doi: 10.1136/thx.2005.052399.
- Keselman A, Heller N. Estrogen Signaling Modulates Allergic Inflammation and Contributes to Sex Differences in Asthma. Front Immunol, 2015; 6. doi: 10.3389/fimmu.2015.00568.
- Ferrero S, Petrera P, Colombo BM, et al. Asthma in women with endometriosis. Hum Reprod, 2005; 20(12): 3514-3517. doi: 10.1093/humrep/dei263.
- McDonald VM, Hiles SA, Jones KA, Clark VL, Yorke J. Health-related quality of life burden in severe asthma. Med J Aust, 2018; 209(2).
- Kharaba Z, Feghali E, El Husseini F, et al. An Assessment of Quality of Life in Patients with Asthma Through Physical, Emotional, Social, and Occupational Aspects. A Cross-Sectional Study. Front Public Health, 2022; 10: 883784. doi: 10.3389/fpubh.2022.883784.
- Simoens S, Dunselman G, Dirksen C, et al. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres. Hum Reprod, 2012; 27(5): 1292-1299. doi: 10.1093/humrep/des073.

