Knee Osteoarthritis Falls Injuries Interactions: Retrospective 2023 Overview and Emerging Implications
Ray Marks*
OARC Clinical Research and Education Director, Ontario L3T 5H3, Canada
Received Date: 22/12/2023; Published Date: 08/05/2024
*Corresponding author: Ray Marks, OARC Clinical Research and Education Director, Ontario L3T 5H3, Canada
Abstract
Knee osteoarthritis, a widespread arthritic disease, commonly resulting in considerable pain and functional disability among both young as well as older adults, is often accompanied by an increased tendency to fall and sustain various degrees of injury. But what does the research show specifically? This report aimed to update what is known about the risk factors for falls in the context of knee osteoarthritis. Using the PUBMED data base and others, clinical studies published between January 1, 2020 and December 31, 2023 concerning possible falls and osteoarthritis of the knee linkages were sought. The search results revealed a growing interest in this topic and that knee osteoarthritis can lead to the changes of incurring one or more falls and further health and disability challenges. Yet, even when multiple potential falls explanatory risk factors are studied, the diverse results remain less than conclusive. Thus, more resounding research is strongly indicated.
Keywords: Falls; Fall injuries; Falls risk factors; Knee osteoarthritis; Pain; Prevention
Introduction
Osteoarthritis, the most common form of arthritis is a universally disabling disease commonly affecting one or more freely moving joints such as the knee joints and others, such as the hip joint. A disease mainly impacting older adults, but not exclusively, knee osteoarthritis is frequently associated with various degrees of pain plus oftentimes a progressive loss of the ability of the affected person to function physically. Regardless of age, among the challenges noted in many diagnosed as having knee osteoarthritis are joint swelling of varying degrees, joint stiffness, gait abnormalities, and often a strong tendency for one or more affected knee joints to ‘give way’, along with possible further injury to the knee joints and others [1-4]. At the same time, even if the knee joints are stable, knee osteoarthritis symptoms plus any prevailing diseases commonly associated with both aging and osteoarthritis such as obesity, diabetes, and cardiovascular diseases can all increase the risk of injurious falls, including recurrent falls, and fractures [5, 6]. Other related disease factors including the strong presence of depression, the lack of adequate sleep, sarcopenia, plus possible medications that can heighten a risk for falls [7]. As well, neurological disease correlates, such as impaired balance capacity, impaired step kinematics, and proprioception [8] may have diverse knee osteoarthritis adverse fall-associated implications.
In the face of rising health care costs, and high numbers of aging adults worldwide, and the prevalence of knee osteoarthritis, a strong need to address remediable factors in the disability cycle has been discussed [9], but no definitive conclusion has emerged as of 2020 [6].
Key Research Questions
- Is there any agreed upon linkage between one or more than one of these aforementioned falls factors that could be harnessed towards more effective falls prevention efforts among those with knee osteoarthritis? In particular, are falls prevention programs for knee osteoarthritis cases of import? If so, what specific approaches are indicated? Finally, is the association between falls and knee osteoarthritis uni or bidirectional in selected cases?
- Will careful early evaluation of adults with knee osteoarthritis disease to examine their risk for falling, deter or improve knee osteoarthritis disability? [9].
- Since falls associated with knee osteoarthritis can thus magnify or induce a life time of suffering, plus account for significant proportion of health costs [8], should more emphasis on this possible preventable health association be forthcoming? That is, is there evidence that a strong case can be made for more public health investments towards well designed and resourced efforts to mitigate the possible cycle of excess knee osteoarthritis progression, plus persistent or recurrent fall-associated injuries?
- Moreover, if preventive strategies do exist are they grounded in a strong evidence base or are they too general, or of high merit-but not followed, contemplated or actively avoided by adults with knee osteoarthritis because they are seen as ‘stigmatizing? [10].
Rationale
Both knee osteoarthritis as well as falls injuries currently pose an enormous challenge to many aging individuals, worldwide, as well as tremendous challenges to health providers, plus immense hospital and societal costs. At the same time, the disease may impact life quality, as well as the ability to live independently in the community. But what produces falls that can impact knee osteoarthritis outcomes negatively is uncertain at best, and whether a fall can initiate a cycle of knee osteoarthritis damage is even less well understood and relatively unknown.
Since outcomes for knee osteoarthritis sufferers’ who fall are significantly worse than those who don’t, and surgery to replace a knee, does not always prevent falls post surgery, it appears a better understanding of what specific variables might be amenable to intervention in at risk individuals, and achieving evidence based guidelines in this respect would undoubtedly be highly advantageous in the context of primary, as well as secondary and tertiary preventive efforts [11]. Moreover, since falling, as well as excess pain and disability that can arise due to falls are paramount among the important causes of premature mortality and morbidity in advanced age, the assessment of risk factors for falling and effective strategies to prevent these appear of specific salience to consider in the context of primary disabling knee osteoarthritis.
Hypothesis
There is a consistent cyclical linkage between the onset and progression of disabling knee osteoarthritis in the older population that can be mediated by neuromuscular factors and others that may be remediable.
Methods
The desired data believed to address the key questions posed in this mini review were sought largely on the PUBMED electronic data base when applying the key terms: “knee osteoarthritis and falls”, “knee osteoarthritis and falls risk/injury”. As well, the PubMed Central, and Google Scholar data bases were reviewed for additional data. Articles published in the English language as full reports and pertinent to the current theme, with the exception of falls relative to older adults in general, and/or total knee joint replacement surgery prospective follow up studies were sought. Excluded were articles that did not discuss knee osteoarthritis per se, for example those that discussed falls and hip osteoarthritis, articles on the perception of possible falls, the fear of falling, or falls self-efficacy. Available data representing the post-COVID 19 onset period and extending from January 1 2020-December 15, 2023 were carefully reviewed even if their embedded data sources were not current. No ethics approval was required, as this narrative review and presents data that does not violate human rights, as documented in The Helsinki Declaration. Those articles of potential relevance deemed pertinent in the author’s view to the present topic, were downloaded and scrutinized further. The review material was then carefully examined and summarized and reported in narrative form, given the lack of any uniform focus or diagnostic descriptions in most studies. All forms of clinical study as well as review articles were deemed acceptable, and stressed the topic of falls risk factors in the context of definitive knee osteoarthritis, rather than the role of falls in causing possible knee osteoarthritis. Post-surgical knee osteoarthritis falls studies were excluded, as were treatment proposals or partially completed studies. Each review focused on what was observed and concluded. PUBMED was selected as the key electronic data source of information given its widespread data repository and effective method of accessing relevant data. Readers seeking more historic perspectives are encouraged to refer to Nyugen [13], di Fraturra et al. [14], Tasci Bosbaz et al. [15], Ng et al. [16], Mat et al. [17], Manlapaz et al. [18], and for more current information Zhang et al. [6].
Results
Even though this was a restricted review, it was clear that knee osteoarthritis remains a topic of immense interest has been studied in over 14,000 reports published since 2020 and its key risk factors that have been studied for 35 years or more. Of these, 115 related current PUBMED articles, including 40 posted between January 2023 and December 2023 and that highlighted knee osteoarthritis and falls were consistent in asserting that this association is highly important to clarify more specifically. This recommendation is indeed recounted by almost all current authors whether they studied similar or dissimilar aspects of the issue.
In this regard, one of several of these recent papers, that by Manlapaz et al. [18] who reported on an electronic data search on this topic that yielded 4382 studies related to falls and knee osteoarthritis, only found 11 were eligible for their systematic review. Although the studies met the inclusion criteria for review, they showed risk factors were not uniform in any respect, but tended to occur in association with impaired balance, muscle weakness, the presence of chronic illnesses, and increasing numbers of symptomatic joints. The presence of knee pain was also identified as a risk factor for falls; however, the strength of evidence was rated as "conflicting". No mention was made of health status or cognitive factors, environmental or neurological falls injury factors. Surprisingly, limited support for knee instability, impaired proprioception, and use of walking aids was found. However, this may be due to the widespread use of self-reports, studies that have biased attributes, and the aggregation of data from hip as well as knee osteoarthritis [6] or because the method of assessing falls risk factors separately rather than collectively in knee osteoarthritis cases may yield falls data comparable to that of control disease free elders [19].
Rosadi et al. [8] note however, that the risk of falls may be higher in those cases of knee osteoarthritis with higher degrees of dysfunctional symptoms, such as a persistent fear of falls, low back pain, diabetes mellitus, and an increased body mass index, even though Zhang et al. [6] found no lasting cumulative influence of similar factors on recurrent falls among knee osteoarthritis cases when measured with radiographs rather than clinical symptoms. Rosadi et al. [8] also felt their study showed that knee proprioception and joint range of motion are potential falls risk factors as these tentatively serve as protective factors against falls, but may increase the older adults falls risk in the face of progressive knee joint damage and increasing instability [20]. In another study, adults with knee osteoarthritis who fell more often than those without knee osteoarthritis demonstrated a relevant percentage of falls to be associated with perceptions of imbalance or knee instability that was similar to that of older knee osteoarthritis cases [21].
According to Iijima et al. [22] who examined cases with sarcopenia plus knee osteoarthritis, those with both these attributes tended to have a 4.17 times higher odds of incurring two or more falls than controls after adjustment for age, sex, and body mass index. The increased recurrent falls experience was not clearly confirmed in participants with isolated sarcopenia and knee osteoarthritis, but a loss of muscle mass is likely to have an impact on balance and timely reflex response ability. In contrast, van Schoor et al. [23] who observed Individuals with clinical knee osteoarthritis showed this group to be at an increased risk for recurrent falls. This relationship was mediated by pain medication, particularly the use of opioids. In addition, a falls risk appears to be more likely in cases showing possible challenges in carrying out dual tasks when walking or trying to balance [24-26], as well as in those with altered gait and gaze behaviors [27]. Additional findings by Aljehani et al. [4] confirm knee osteoarthritis fallers do have high levels of back pain and appear to walk shorter distances over a six-minute period than non-fallers.
In terms of falls alone, Devassy et al. [28] found older women who have cognitive symptoms of anxiety and stress may have a higher than anticipated chance of falling, as may those with muscle weakness and early pathological changes in the neuromuscular system [13].
Harris et al. [29] noted older adults with radiographic evidence of knee osteoarthritis tended to have an increased likelihood of experiencing recurrent falls that may be partially explained by the use of opioids to control pain [23, 30-33] and/or by an associated abnormality in gait cycle mechanics and joint protection [13, 15, 34]. Indirectly, those who are depressed or exhibit a fear falling or both may also tend to fall more readily [35, 36] with dire consequences [31, 33], although the combined role of physical as well as psychological correlates cannot be ruled out [7, 19].
Manlapaz et al. [18] did show that impaired balance, muscle weakness, the presence of comorbidities, and increasing number of symptomatic joints are falls risk factors. However, as in other realms of osteoarthritis research, the strength of the evidence was rated as "conflicting" because of the inconsistency of the findings. Surprisingly, even though the authors found limited evidence for knee instability, impaired proprioception, and use of walking aids as falls determinants, no updated study has examined and published data on these possible valuable explanatory and mediating correlates as of 2023. The role of disease severity or grade of disease another possibly highly salient falls predictor has also not been well studied, and remains controversial. In addition, stability and balance functions are also greatly influenced by the patient's falling experience and the level of pain that may be of high relevance [38] along with compromised balance that could provoke a fall when walking [39].
It is also apparent that personal factors are more likely to predict falls and fractures than osteoarthritis impairments, and include environmental factors, activity limitations and participation restrictions in people with definitive osteoarthritis or at high risk for developing osteoarthritis [39]. In another report,
Ren et al. [40] found selected muscle responses needed to protect against sudden perturbations were suboptimal in those with knee osteoarthritis disability that could provoke falls. Other examples of current reports and their insights are listed below.
Table 1: Selected features of representative studies examining falls risk factors among cases with knee osteoarthritis as published between January 1 2020 and December 15, 2023 and showing diversity of enterprise and conclusions.
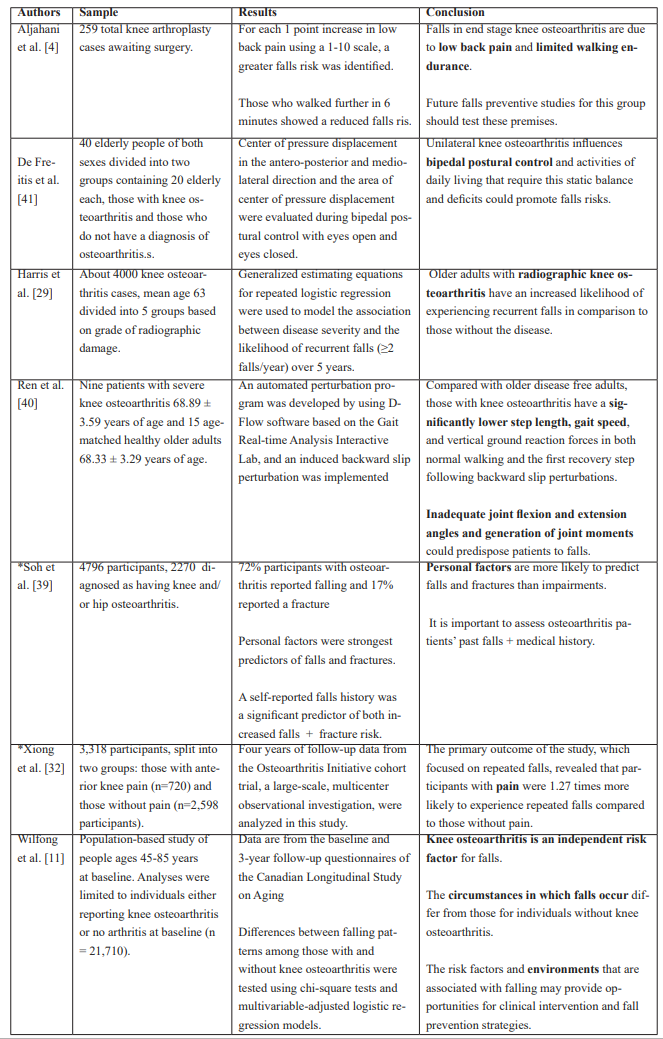
*Data source=Osteoarthritis Initiative (https://nda.nih.gov/oai/)
In short, as per Table 1 and other data cited above, the relative impact of those variables studied to date to explain ors predict the nature of the knee osteoarthritis-falls linkage are highly complex to unravel. In addition, in the absence of careful sub studies, whether numbers of affected joints, osteoarthritis severity, muscle force capacity, and timing, balance, walking ability, pain, and medication intake are of key import and if so, in what respect, is hard to discern at best.
In addition, study inclusion criteri that omt cases with mental health issues, render it unclear as to whether possible cognitive factors deemed to underpin falls risk in older adults, also impact those with knee osteoarthritis and should be closely examined in the future in this regard. The role of poor coordination, balance, and deficits in gait control that appear to underlie falls risk in older weakened adults with painful knee osteoarthritis [13, 24, 37] also warrants further study.
In the interim, although not well recognized, it appears safe to say knee osteoarthritis, which is clearly an important contributor to falling among older adults is its own right, is an especially noteworthy and clinically relevant falls determinant warranting urgent attention in the realm of falls mitigation as well as knee osteoarthritis disability.
Discussion
Knee osteoarthritis, a progressively disabling joint disease that is increasing in prevalence despite years of study is a costly disease among older adults in all parts of the world. At the same time, the prevalence of falls among older populations and that can be attributed in part to knee osteoarthritis disease features is an unsolvable problem in its own right. In this regard, many have turned their attention towards teasing out the underpinnings of observed knee joint disease determinants as well as those that hasten its progression or drawing attention to the need for a more focused research and clinical approach [42]. Others have sought to reveal the key importance of identifying remediable disease outcomes and pathogenic factors in general, and those related to falls risk. In this regard, a sizeable number of investigators tend to agree regarding the key factors that may predispose older knee osteoarthritis and raise the risk for falling and sustaining one or more additional injuries [2], as well as possible joint damage or worse knee osteoarthritis outcomes than anticipated [11] even if no conclusive results prevail [43]. Yet it is concluded by most authors that evidence supports the view that falls are inextricably linked to knee osteoarthritis among other determinants. But fewer groups have sought to examine if falls, a major health issue in its own right, can lead to the onset of knee osteoarthritis, an hypothesis that cannot be ruled out. However, many papers currently imply some degree of relevance must be attributed to muscle as well as nerve associated pathways that affect gait. In addition, most concur that knee osteoarthritis and falls are potentially associated even if their underpinnings are not singular or well codified [42, 44]. Moreover, even if it appears those with more severe disease may fall to the same degree as those with less joint damage, this is mostly true for radiological not the clinical disease features of knee osteoarthritis [43]. However, even when the data sources examined are known to be reputable, and give the impression that they house a reasonable number of relevant papers on the present topic of interest, most do not appear to be based on any sound theoretical framework and thus a high number either examine many possible falls knee osteoarthritis correlates simultaneously, while others only examine a small number. Some data drawn from specific data repositories and not others, and analyses that employ secondary data sets captured in the previous decade using surveys and medical charts, may not represent the entirety of the situation as this occurs globally in 2023 and following the fallout of the COVID pandemic.
How the issues of knee osteoarthritis and falls proceed is however rarely studied prospectively in non surgical contexts as opposed to those detailing post surgical knee osteoarthritis follow up studies and falls occurrences. At the same time, what is being measured specifically is unclear as the terms applied for both knee osteoarthritis as well as falls, falling, and recurrent falls are not uniformly defined or employed across available studies. As well, a high number of studies continue to rely on subjective reports and measures that could be flawed, for example the frequency of falls incidents as recounted by patients who must rely on memory.
The possible confounding factors of differing osteoarthritis phenotypes, types of falls, falls location, disease duration, and extent, plus the role of prior surgery, overall health status, corticosteroid injections and others, and a trend to include a wide age range of study subjects versus stratification of key determinants also continues to truly preclude any meaningful summative analysis of prevailing data from what has been collected or aggregated to date as argued by Li et al. [45].
According to some of this data however, one can predict with reasonable certainty that older adults with knee osteoarthritis may be more prone to falling or falls than healthy age-matched adults, even if this is not universally supported. On the contrary, it has been possible to argue that that osteoarthritis may actually be protective against falls and related fractures, especially if it is severe and induces less rather than more weight bearing activities. However, if this is so, it is unclear how poor toe grip strength on the affected side appears to raise the risk for falling in knee osteoarthritis cases [46], or why joint replacement surgery does not obviate falls risk entirely [14]. There is also evidence that a persistent preoccupation related to an incident fall, term also called fear of falling by some authors, is of interest in the fields of geriatrics and gerontology because it is related to the risk of falling and subsequent morbidity of falling [36].
It is accepted that this report is a limited one and articles for inclusion missed. The quality of the reported assessments too cannot be readily discerned. But even so, what the weightings of the possible role of balance, muscle strength and proprioception problems and others in explaining the prevailing falls rate among osteoarthritis knee cases are remains challenging to unravel Moreover, the role of comorbid health conditions, gender, and age, plus obesity is clearly relevant but the magnitude of these factors is hard to discern [9].
It is also apparent that some of the data may be erroneous or underreported or exaggerated by the immense reliance in this data base on self-reports to assess falls history, along with the frequent exclusion of osteoarthritis cases who might be cognitively challenged as well as at high risk for falls. Additionally, efforts to examine the precise role of other potentially modifiable risk factors not highlighted in the literature, such as diabetic neuropathy, joint inflammation, assistive device use, footwear, sedatives, sleep issues, frailty, fatigue, social factors, and health beliefs about falling may prove insightful. At the same time, efforts to differentiate static from dynamic balance, which has not been studied to any degree in the knee osteoarthritis population, and its possible falls linkage warrant study among samples of cases with well-defined and clearly established clinical and radiological knee osteoarthritis, and disease sub groups.
Research Implications
Further research that may well offer more conclusive applied directions and insights include: examining the role of
- Nutritional [eg magnesium intake], cognitive, and health status factors [44, 47].
- Medication intake, environmental, and sleep factors [11].
- Specific knee osteoarthritis correlates, such as pain, postural sway, joint stability, dynamic balance during gait, muscle fatigue, contracture, muscle modulation capacity [48] and atrophy, plus falls fears and falls self-efficacy [38, 41, 46-50] and obesity [9].
To advance this line of inquiry, efforts to more clearly differentiate high from low falls risk individuals using samples that match the median age of most knee osteoarthritis cases and who have either distinctive unilateral versus bilateral knee joint disease, that is not compounded by hip joint osteoarthritis will be helpful. Additional efforts to differentiate the relative impact of falls risk in early versus late stages of knee osteoarthritis, and in medial versus lateral compartment knee osteoarthritis, are similarly highly indicated. The development and validation of practical cost-effective reliable personalized screening tools, including that can capture falls history, age, sex, fear of falling trends, medication usage, knee osteoarthritis severity, lower limb pain, gait speed, and proprioception are paramount as well [51].
Until then, despite a laudable number of published falls prevention approaches and even in the event relevant articles do prevail, a definitive evidence base for employing one or more of these remains elusive. As well, even if deemed effective when studied in controlled conditions, some, falls preventive programs may not be sufficiently personalized or accessible to all who need these, thus accounting for the high [40%] percentage of those with a falls history undergoing surgery [56]. At the same time, not all home based exercises or treatment plans are likely to prove helpful if not individualized and closely monitored, especially among those with one or more balance problems, cardiovascular conditions and others, such as intractable pain, depression and, and neuromuscular deficits.
Clinical Implications
Notwithstanding the limitations discussed above and others, until more compelling data are forthcoming, applying what we do know carefully for purposes of decreasing falls risk among vulnerable in knee osteoarthritis cases may have profound health savings and favorable longevity implications. Insightful efforts that do not rely solely on public health strategies, but on careful evaluation of the vulnerable subject’s perceptions and beliefs, their overall fall history, fears regarding falling [immense fear or no fear-that could both be problematic], type and usage of prescribed medications, knee osteoarthritis severity, pain extent, walking and balance facility and and environmental safety issues. Moreover, efforts that may be indicated based on the current research, but not enacted to date, for example, treating low back pain to avert its effect on falls risk along with little attention to the individual’s personal beliefs, plus their cognitive, physical, and medical profile should be reviewed accordingly.
Finally, to improve the chances of mitigating falls and their possible harm in older adults with knee osteoarthritis, interventions to maximize muscle strength at the knee, training to foster better postural control and desirable reflex responses, as well as efforts to allay pain, depression and falls fears may prove noteworthy [55, 56-58].
Concluding Thoughts
Despite the immense clinical relevance of falls and their mitigation in the older adult population in general, as in the knee osteoarthritis population, in particular, there remain numerous challenges. Nonetheless, in recognizing the present narrative overview is not a systematic analysis or an expansive one, it is believed the review highlights several important issues for the researcher, as well as the practitioner as follows:
- Falls are serious injuries that may prevail in sizeable numbers of knee osteoarthritis cases, and can heighten knee osteoarthritis disability considerably in multiple ways.
- Posture and balance as well as muscle modulation factors appear of high import among the key risk factors explaining falling in knee osteoarthritis even after knee joint replacement surgery.
- The entire neurological system, not only the skeletal system may have an incremental and collective impact on joint stability unless identified and attenuated.
- To advance this line of inquiry-the clinical prediction rule developed by Amano et al. [52], along with the Comprehensive Geriatric Assessment tool [53] and objective neuromuscular analogues of balance [55] should be carefully examined in those at risk for falling as these appear to hold great promise.
- It is also concluded that knee osteoarthritis cases should be screened for their falls risk periodically including pre surgery and made aware of their falls risk and their help should be sought in averting falls in the future rather than ignored even after surgery.
- In planning to avert excess falls associated knee osteoarthritis disability, efforts to address knee extensor muscle weakness, muscle wasting, and deficient reflex responsiveness, and pain should be forthcoming at all disease stages.
Funding: None.
Acknowledgments: None.
Conflicts of Interest: “The author declares no conflict of interest.”
References
- Karimi MT, Sharifmoradi K. Static and local dynamic stability of subjects with knee joint osteoarthritis. Proc Inst Mech Eng H, 2022; 236(8): 1100-1105.
- Ataullah AHM, De Jesus O. Gait Disturbances, In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
- Deng ZH, Xu J, Long LJ, et al. Association between hip and knee osteoarthritis with falls: A systematic review and meta-analysis. Int J Clin Pract, 2021; 75(10): e14537.
- Aljehani MS, Crenshaw JR, Rubano JJ, et al. Falling risk in patients with end-stage knee osteoarthritis. Clin Rheumatol, 2021; 40(1): 3-9.
- Cai G, Li X, Zhang Y, et al. Knee symptom but not radiographic knee osteoarthritis increases the risk of falls and fractures: results from the Osteoarthritis Initiative. Osteoarthritis Cartilage, 2022; 30(3): 436-442.
- Zhang Y, Li X, Wang Y, et al. Association of knee and hip osteoarthritis with the risk of falls and fractures: a systematic review and meta-analysis. Arthritis Res Ther, 2023; 25(1): 184.
- Iijima H, Shimoura K, Aoyama T, et al. Low back pain as a risk factor for recurrent falls in people with knee osteoarthritis. Arthritis Care Res, 2020.
- Rosadi R, Jankaew A, Wu PT, et al. Factors associated with falls in patients with knee osteoarthritis: A cross-sectional study. Medicine (Baltimore), 2022; 101(48): e32146.
- Veronese N, Koyanagi A, Soysal P, et al. Dynapenic abdominal obesity and susceptibility to fall: a prospective analysis of the Osteoarthritis Initiative. Front Nutr, 2023; 10: 1153399.
- Tsindos T, Ayton D, Soh SE, et al. Perceptions of falls risk and falls prevention among people with osteoarthritis. Disabil Rehabil, 2020; 1-8.
- Wilfong JM, Perruccio AV, Badley EM. Examination of the Increased risk for falls among individuals with knee osteoarthritis: a Canadian longitudinal study on aging population-based study. Arthritis Care Res (Hoboken), 2023; 75(11): 2336-2344.
- Veronese N, Honvo G, Bruyère O, Rizzoli R, Barbagallo M, Maggi S, et al. Knee osteoarthritis and adverse health outcomes: an umbrella review of meta-analyses of observational studies. Aging Clin Exp Res, 2023; 35(2): 245-252.
- Nguyen BM. Myofascial trigger point, falls in the elderly, idiopathic knee pain and osteoarthritis: an alternative concept. Med Hypotheses, 2019; 80(6): 806-809.
- di Laura Frattura G, Filardo G, Giunchi D, et al. Risk of falls in patients with knee osteoarthritis undergoing total knee arthroplasty: a systematic review and best evidence synthesis. J Orthop, 2018; 15(3): 903-908. doi: 10.1016/j.jor.2018.08.026.
- Tasci Bozbas G, Sendur OF, Aydemir, AH. Primary knee osteoarthritis increases the risk of falling. J Back Musculoskelet Rehabil, 2017; 30(4): 785-789. doi: 10.3233/BMR-150413.
- Ng CT, Tan MP. Osteoarthritis and falls in the older person. Age Ageing, 2013; 42(5): 56156-56156.
- Mat S, Tan PJ, Ng CT, et al. Mild joint symptoms are associated with lower risk of falls than asymptomatic individuals with radiological evidence of osteoarthritis. PLoS One, 2015; 22: 10(10). e0141368.
- Manlapaz DG, Sole G, Jayakaran P, et al. Risk factors for falls in adults with knee osteoarthritis: a systematic review. PM R, 2019; 11(7): 745-757.
- Norouzi P, Javadian Y, Hosseini SR, Mousavi Khatir SR, Bijani A. Comparison of falls and its determinants in the elderly with and without knee osteoarthritis. J Babol University of Med Sci, 2023; 25(1): 46-57.
- Raizah A, Reddy RS, Alshahrani MS, Tedla JS, Dixit S, Gular K, et al. Investigating knee joint proprioception and its impact on limits of stability using dynamic posturography in individuals with bilateral knee osteoarthritis-a cross-sectional study of comparisons and correlations. J Clin Med, 2023; 12(8): 2764.
- Iosimuta N, Santos WN, Sousa T, Jardim R, Matos A. Number of falls in elderlies and adults with knee osteoarthritis (KOA). Arch Phys Med Rehabil, 2022; 103(3): e36.
- Iijima H, Aoyama T. Increased recurrent falls experience in older adults with coexisting of sarcopenia and knee osteoarthritis: a cross-sectional study. BMC Geriatr, 2021; 21(1): 698. doi: 10.1186/s12877-021-02654-4.
- van Schoor NM, Dennison E,Castell, MV, Cooper C, Edwards MH, Maggi S, et al. EPOSA research group. Clinical osteoarthritis of the hip and knee and fall risk: the role of low physical functioning and pain medication. Semin Arthritis Rheum, 2020; 50(3): 380-386. doi: 10.1016/j.semarthrit.2020.02.006.
- Bezalel G, Nachoum Arad G, Plotnik M, Friedman J. Voluntary step execution in patients with knee osteoarthritis: Symptomatic vs. non-symptomatic legs. Gait Posture, 2021; 83: 60-66. doi: 10.1016/j.gaitpost.2020.10.006.
- Abdallat R, Sharouf F, Button K, Al-Amri M. Dual-Task Effects on Performance of Gait and Balance in People with Knee Pain: A Systematic Scoping Review. J Clin Med, 2020; 9(5): 1554. doi: 10.3390/jcm9051554.
- Amano T, Tamari K, Suzuki N. Cross-Validation of a Screening Tool to Distinguish Between Fallers and Nonfallers in Community-Dwelling Older Adults with Knee Osteoarthritis. Arch Phys Med Rehabil, 2021; 102(4): 598-603. doi: 10.1016/j.apmr.2020.12.001.
- Le Rossignol S, Fraser E, Grant A, Doma K, Wilkinson M, Morse L, et al. Patients with knee osteoarthritis have altered gait and gaze patterns compared to age-matched controls: a pilot study. PLoS One, 2023; 18(11): e0283451.
- Devassy SM, Scaria L. Prevalence and risk factors for falls in community-dwelling older population in Kerala; results from a cross sectional survey. Heliyon, 2023; 9(8): e18737.
- Harris R, Strotmeyer ES, Sharma L, Kwoh CK, Brach JS, Boudreau R, et al. The Association Between Severity of Radiographic Knee OA and Recurrent Falls in Middle and Older Aged Adults: The Osteoarthritis Initiative. J Gerontol A Biol Sci Med Sci, 2023; 78(1): 97-103. doi: 10.1093/gerona/glac050.
- Taqi A, Gran S, Knaggs RD. Current use of analgesics and the risk of falls in people with knee osteoarthritis: A population-based cohort study using primary care and hospital records. Osteoarthr Cartil Open, 2021; 3(2): 100165. doi: 10.1016/j.ocarto.2021.100165.
- Silverman S, Schepman P, Rice JB, Beck CG, Pajerowski W, White AG, et al. Risk Factors Associated with Falls and Fractures Following Prescription of Opioids Among Privately Insured Patients with Osteoarthritis. J Health Econ Outcomes Res, 2022; 9(2): 47-56. doi: 10.36469/001c.32584.
- Xiong T, Ou Y, Chen S, Liu S, Yi X, Deng X, et al. Anterior knee pain as a potential risk factor for falls in older adults: insights from the osteoarthritis initiative data. BMC Public Health, 2023; 23(1): 2288. doi: 10.1186/s1288
- Capiau A, Huys L, van Poelgeest E, van der Velde N, Petrovic M, Somers A. EuGMS Task, Finish Group on FRIDs. Therapeutic dilemmas with benzodiazepines and Z-drugs: insomnia and anxiety disorders versus increased fall risk: a clinical review. Eur Geriatr Med, 2023; 14(4): 697-708. doi: 10.1007/s41999-022-00731-4.
- Ebihara B, Fukaya T, Mutsuzaki H. Relationship between Quadriceps Tendon Young's Modulus and Maximum Knee Flexion Angle in the Swing Phase of Gait in Patients with Severe Knee Osteoarthritis. Medicina (Kaunas), 2020; 56(9): 437. doi: 10.3390/medicina56090437.
- Ofori-Asenso R, Ackerman IN, Soh SE. Prevalence and correlates of falls in a middle-aged population with osteoarthritis: data from the Osteoarthritis Initiative. Health Soc Care Community, 2020. doi: 10.1111/hsc.13103.
- González-Olguín A, Ramos Rodríguez D, Higueras Córdoba F, Martínez Rebolledo L, Taramasco C, Robles Cruz D. Classification of Center of Mass Acceleration Patterns in Older People with Knee Osteoarthritis and Fear of Falling. Int J Environ Res Public Health, 2022; 19(19): 12890. doi: 10.3390/ijerph191912890.
- Konarzewski P, Konarzewska U, Kuryliszyn-Moskal A, et al. What influences proprioceptive impairments in patients with rheumatic diseases? Analysis of different factors. Int J Environ Res Public Health, 2023; 20(4): 3698.
- Lee PA, Wu KH, Lu HY, Su KW, Wang TM, Liu HC, et al. Compromised balance control in older people with bilateral medial knee osteoarthritis during level walking. Sci Rep, 2021; 11(1): 3742. doi: 10.1038/s41598-021-83233-w.
- Soh SE, Barker AL, Morello RT, Ackerman IN. Applying the International Classification of Functioning, Disability and Health framework to determine the predictors of falls and fractures in people with osteoarthritis or at high risk of developing osteoarthritis: data from the Osteoarthritis Initiative. BMC Musculoskelet Disord, 2020; 21(1): 138. doi: 10.1186/s12891-020-3160-5.
- Ren X, Lutter C, Kebbach M, Bruhn S, Yang Q, Bader R, et al. Compensatory Responses During Slip-Induced Perturbation in Patients with Knee Osteoarthritis Compared with Healthy Older Adults: An Increased Risk of Falls? Front Bioeng Biotechnol, 2022; 10: 893840. doi: 10.3389/fbioe.2022.893840.
- de Freitas REJ, de Freitas JGA, Vieira CP, Endres DC, Inacio FM, da Silva Azevedo Nora FG. Analysis of Postural Control in Patients Diagnosed with Unilateral Knee Osteoarthrosis and Its Relationship with the Risk of Falls. Adv Orthop, 2023; 2023: 5536304. doi: 10.1155/2023/5536304.
- Ackerman IN, Barker A, Soh SE. Falls prevention and osteoarthritis: time for awareness and action. Disability and rehabilitation, 2023; 45(4): 733-738.
- Ribeiro IC, Coimbra AMV, Costallat BL, Coimbra IB. Relationship between radiological severity and physical and mental health in elderly individuals with knee osteoarthritis. Arthritis Res Ther, 2020; 22(1): 187. doi: 10.1186/s13075-020-02280-2.
- Zheng Z, Luo H, Xu W, Shi L, Wang F, Qiu Y, et al. Association between Elevated Magnesium Intake and Reduced Risk of Recurrent Falls and Frailty in Osteoarthritis: Data from the Osteoarthritis Initiative. J Nutr Health Aging, 2023; 27(9): 775-784.
- Li Y, Hou L, Zhao H, Xie R, Yi Y, Ding X. Risk factors for falls among community-dwelling older adults: A systematic review and meta-analysis. Front Med (Lausanne), 2023; 9: 1019094. doi: 10.3389/fmed.2022.1019094.
- Mawarikado Y, Inagaki Y, Fujii T, Kubo T, Kido A, Tanaka Y. Relationship between fall history and toe grip strength in older adults with knee osteoarthritis in Japan: A cross-sectional study. PLoS One, 2023; 18(3): e0282944. doi: 10.1371/journal.pone.0282944.
- Taniguchi M, Sawano S, Maegawa S, Ikezoe T, Ichihashi N. Physical Activity Mediates the Relationship between Gait Function and Fall Incidence after Total Knee Arthroplasty. J Knee Surg, 2021; 34(11): 1205-1211. doi: 10.1055/s-0040-1702165.
- Temporiti F, De Leo D, Adamo P, Papa G, Traverso F, Maffiuletti N, et al. Impaired Modulation of Motor and Functional Performance in Patients after Total Knee Arthroplasty: A Prospective Observational Study. Biomed Res Int, 2022; 2022: 4546836. doi: 10.1155/2022/4546836.
- Fukaya T, Mutsuzaki H, Mori K. Sway and Acceleration Changes of the Center of Mass during Walking Stance Phase before and after Total Knee Arthroplasty. Geriatrics (Basel), 2022; 8(1): 2. doi: 10.3390/geriatrics8010002.
- Kiyohara M, Hamai S, Okazaki K, Fujiyoshi D, Mizu-Uchi H, Nakashima Y. Evaluation of the balance function before and after total knee arthroplasty using Berg balance scale. Arch Orthop Trauma Surg, 2022; 142(11): 3461-3467. doi: 10.1007/s00402-021-04233-z.
- Makino K, Lee S, Bae S, Chiba I, Harada K, Katayama O, et al. Simplified Decision-Tree Algorithm to Predict Falls for Community-Dwelling Older Adults. J Clin Med, 2021; 10(21): 5184. doi: 10.3390/jcm10215184.
- Long S, Hu L, Luo Y, Li Y, Ding F. Incidence and risk factors of falls in older adults after discharge: a prospective study. Int J Nurs Sci, 2022; 10(1): 23-29. doi: 10.1016/j.ijnss.2022.12.010.
- Veronese N, Siri G, Cella A, Maggi S, Maggi S, Zigoura E, et al. The Multidimensional Prognostic Index predicts falls in older people: an 8-year longitudinal cohort study of the Osteoarthritis Initiative. J Am Med Dir Assoc, 2020; 2(5): 669-674.
- Blasco JM, Pérez-Maletzki J, Díaz-Díaz B, Silvestre-Muñoz A, Martínez-Garrido I, Roig-Casasús S. Fall classification, incidence and circumstances in patients undergoing total knee replacement. Sci Rep, 2022; 12(1): 19839. doi: 10.1038/s41598-022-23258-x.
- Tütüncüler E, Ök N, Güngör HR, Bayrak G, Şavkın R, Büker N. A comparison of balance and fall risk in patients with unilateral and bilateral total knee arthroplasty. J Back Musculoskelet Rehabil, 2022; 35(5): 1043-1051. doi: 10.3233/BMR-210127. PM 35001874.
- Zapparoli L, Sacheli LM, Seghezzi S, et al. Motor imagery training speeds up gait recovery and decreases the risk of falls in patients submitted to total knee arthroplasty. Sci Rep, 2020; 10(1): 8917.
- Barbour KE, Sagawa N, Boudreau RM, et al. Knee osteoarthritis and the risk of medically treated injurious falls among older adults: a community-based US Cohort Study. Arthritis Care Res (Hoboken), 2019; 71(7): 865-874.
- Hislop A, Collins NJ, Tucker K, et al. Hip strength, quadriceps strength and dynamic balance are lower in people with unilateral knee osteoarthritis compared to their non-affected limb and asymptomatic controls. Braz J Phys Ther, 2022; 26(6): 100467.

