Insights and Challenges of Psychological Status Investigation for Different People Age Groups After Covid - 19 Lockdown Impact
Paulius Uselis1,2, Zivile Jacike2 and Audrone Seibokaite2
1Lithuanian University of Health Sciences, Mickeviciaus 9, Kaunas 44307, Lithuania
2Public institution Kaunas City Outpatient Clinic, Pramones pr. 31, Kaunas 51270, Lithuania
Received Date: 01/07/2023; Published Date: 17/11/2023
*Corresponding author: Paulius Uselis, Lithuanian University of Health Sciences, Mickeviciaus 9, Kaunas 44307, Lithuania; Public institution Kaunas City Outpatient Clinic, Pramones pr. 31, Kaunas 51270, Lithuania
Abstract
The lack of comprehensive knowledge during the Covid - 19 due to the lack of experience in how to behave and evaluate such a situation forces to look for additional research methods, detailed analysis and knowledge in psychology. There are a number of studies in the scientific literature about the psychological effects of quarantine. Most of them showed an increased incidence of common mental disorders such as anxiety and depression compared to the general population.
Almost all infectious disease outbreaks studied were recorded before such a wide spread of news in the social space.
Emerging disease and strict public health measures naturally cause people great stress and anxiety. The COVID-19 pandemic has led to the implementation of unprecedented "social distancing" strategies, critical to limiting the spread of the virus. However, the massive effort associated with the necessary quarantine and social distancing measures for COVID-19, especially for older people who have experienced acute debilitating feelings of social isolation and loneliness, can have serious mental and physical health consequences. It is already announced that for a significant part of the population, the quarantine will have direct effects on their mental well-being, for example, they will have to fight with despair or negative emotions, anxiety about getting sick or infecting others. Emerging evidence from developmental psychology suggests that potential effects will vary greatly depending on the age of the child and the socio-demographic characteristics of the family. So, this means that the decisions taken by the government regarding the measures for COVID-19 in the society will affect different age groups of children differently.
Past epidemics have shown that individuals who recover from acute infections can experience varying degrees of psychological trauma and subsequent problems associated with it.
Epidemiological studies confirm that those who experience persistent or severe stress over a long period of time report poorer mental and physical health and increased mortality. Psychosomatic medicine integrates interdisciplinary assessment and management involving multiple specialties, including psychiatry, psychology, neurology, psychoanalysis, internal medicine, pediatrics, surgery, allergy, dermatology, and psychoneuroimmunology.
Exposure to stress can be measured using self-administered questionnaires, such as the Life Events Checklist, which is rated by an interviewer, or objectively determined based on a recent event. Some secretory biomarkers (cortisol, alpha-amylase, pro-inflammatory cytokines) have been developed as stress biomarkers reflecting both ANS (Autoimmune Nervous System) and HPA (Hypothalamo-Pituitary-Adrenocortical) activity.
The review results suggest the lack of evidence of objective diagnostics methods to investigate stress level, duration, other impact for health with perception of possibilities for complex approach of various methodologies, including laboratory stress indicators tests in combination with the PSS research method for optional stress investigation.
Introduction
Current situation, which began in the late autumn of 2019 and has continued for more than two years, marked by the threat of COVID-19 to humanity, will go down in history as one of the biggest pandemics, which claimed more than five million lives, sickened and infected hundreds of millions of people with the terrible virus. Modern man knew little about the effect of self-isolation or the need for it in an age of rapid travel, constant movement and interpersonal communication. Although previous severe acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), Spanish flu, Ebola, and plague have shocked the world with millions of victims, the dominance of technology was not so great as it is today that one would feel strong in isolation from the rest of the world [1]. Humanity always knew what to do now, what to do next, life went on in the usual direction. A sudden catastrophic turn of events forced humanity to face a painful realization - how to live with yourself. Indeed, it is a frightening realization when one or two generations of humanity know what to do in the event of a nuclear disaster, but no longer know how to spend time alone. It affected entire families. Paradoxically, the "virtual connection" provided by social media has made us forget how close relationships should feel, how we feel when we can't touch our loved ones, friends, say hello, extend a hand, hug, cuddle. Fear, submission, uncertainty, denial, aggression - a lot of emotions that fell at the same time and not a single clear, guaranteed solution for today caused a lot of psychological challenges, for which you need to seek help and prevention right now.
Length of quarantine, fear of infection, frustration, boredom, multiple interpretations of social phenomena, insufficient information, financial loss, and stigma [2]. These concepts have become daily companions for people living in quarantine or self-isolation. Thus, the complexity of the situation always causes psychological discomfort, and how to deal with such challenges depends not only on the individual characteristics of a person, but also on the perception and effectiveness of the comprehensive assistance provided by various public organizations and medical specialists. The lack of comprehensive knowledge due to the lack of experience in how to behave and evaluate such a situation forces us to look for additional research methods, detailed analysis and knowledge in psychology.
Collected data published by scientists about the conditions of high psychological tension that occur during any quarantine and in the absence of data about the changes taking place in the face of the current COVID-19 pandemic in personal and social life and their impact on the health of the body, formed the need to perform a complex analysis of the psychological state of people in self-isolation.
The psychological capabilities of scales and laboratory stress indicator research methodology expand the concept of detailed analysis in the presence of the impact of several different groups of stressors on the body: a person's fear of contracting a dangerous infection that is still little known or researched, and the consequences of a psychological discomfort breakthrough after being in self- isolation.
General psychological effects of quarantine
There are a number of studies in the scientific literature about the psychological effects of quarantine. Most of them showed an increased incidence of common mental disorders such as anxiety and depression compared to the general population (American Psychiatric Manual, 2020). Almost all infectious disease outbreaks studied were recorded before such a wide spread of news in the social space. For example, in the case of the Ebola virus, the use of mobile phones was still very limited in the outbreak areas. The fever outbreak itself was more localized and did not reach the level of a pandemic that the global public is now facing [2].
There is strong evidence that not being able to connect with family or friends is directly related to increased anxiety [3]. Today, most families use television, the radio is no longer surprising, the Internet or mobile phones have become mandatory attributes of well-being. However, there are still people, especially the elderly or those with special needs, who do not have access to or ability to use today's communication channels. The mentioned groups are more vulnerable and psychologically, for example, there is constant anxiety about the access to daily services, food and medicine. The support provided includes helplines currently being developed and implemented in most countries around the world [2].
It is important to mention the very risky level of psychological impact of healthcare workers. It is enough to observe how complex details of medical clothing, coveralls, masks, respirators and other equipment that are worn in a mandatory manner create an image of detachment and inaccessibility. Health care workers who have been quarantined have been found to have more severe and pronounced PTSD (posttraumatic stress disease) symptoms than health care workers who have not been quarantined [4]. In part, this may be due to the fact that their responsibilities are to perform work or carry out tasks that are exhausting, intense and in themselves cause not only physical, but also spiritual discomfort [5].
A study conducted in 2003, at a hospital in Toronto, the epicenter of the SARS outbreak, found that quarantined medical workers were concerned about their personal safety, transmission of the infection to family members, stigmatization and interpersonal isolation [6]. Employees were worried about the lack of colleagues due to the quarantine and the excessive workload. The COVID-19 quarantine is not exactly analogous to the SARS epidemic, but studies of health care workers during the SARS outbreak suggest that the need to provide additional mental health care and support to health care workers should not even be considered [7]. It is already announced that for a significant part of the population, the quarantine will have direct effects on their mental well-being, for example, they will have to fight with despair or negative emotions, anxiety about getting sick or infecting others [5].
Psychological reasons for fear of infectious diseases
Emerging disease and strict public health measures naturally cause people great stress and anxiety [8-10]. The COVID-19 pandemic has led to the implementation of unprecedented "social distancing" strategies, critical to limiting the spread of the virus. However, the massive effort associated with the necessary quarantine and social distancing measures for COVID-19, especially for older people who have experienced acute debilitating feelings of social isolation and loneliness, can have serious mental and physical health consequences. The impact may be disproportionately high among those who already have mental illness, loneliness, and isolation prior to the COVID-19 pandemic [10].
Prior to the COVID-19 pandemic, loneliness and social isolation were already prevalent across Europe, the United States and China (10–40%) [11,12], even being labeled a “behavioral epidemic” [13]. The situation has only worsened with the introduction of restrictions to prevent the spread of viruses. In the midst of pandemic lockdowns, not only national but also global economies are suffering, health systems are under enormous critical pressure, mass public hysteria is gaining unbridled momentum, and public hopes and daily lives are mercilessly restricted and constrained (Li et al., 2020).
This COVID-19 pandemic seems to have stopped the speed of our modern society and directly crushed the possibility of unlimited social freedom. Under these social constraints, individuals are forced to accept the reality of isolation, which can provoke domestic violence or boredom. Similar trends of increased isolation and loneliness were observed among emergency workers and quarantined residents in Wuhan, China. This has increased the population's incidence of depression, anxiety, post-traumatic stress disorder and insomnia. Certainly, this promotes fatigue and reduces the quality of work of healthcare workers [14]. It is important to note that the society was not ready to accept this challenge of the pandemic, so the consequences are not predictable.
The fear of infectious diseases, together with the perception of loneliness, causes anger, confusion, disappointment with the government's decisions and can encourage many to ignore the restrictions of quarantine, to rebel, which can cause painful consequences for the entire public health. The emotional unpreparedness for such biological catastrophes has a profoundly damaging effect because the situation is unprecedented in every way. In the absence of the basic amenities of life, thinking about distance or hand disinfection according to established standards is far from acceptable or feasible for everyone.
Isolation causes stress for people of all age groups
Past epidemics have shown that individuals who recover from acute infections can experience varying degrees of psychological trauma and subsequent problems associated with it. For example, in the immediate aftermath of the SARS epidemic, there were a number of reports of increased levels of anxiety, depression, or PTSD [15]. There is also evidence that these problems can be long-term. Wu et al., 2009 reported that 30 months after the SARS outbreak, one- third of ex-infected patients had long-term psychiatric problems observed immediately after the epidemic [16]. Also, not only those infected with the virus experience negative psychosocial consequences. Canadian researchers confirmed that health care workers experienced an intense burst of negative emotional responses during SARS infection, including fear of contracting the virus, feelings of ongoing stigma, loneliness, anger, anxiety, and uncertainty [15].
However, not enough research has been done on the psychological consequences for children and adolescents who find themselves in quarantine or isolation. The collected evidence focuses primarily on children who have direct contact with sick or quarantined individuals. Children who were hospitalized due to SARS were found to experience strong feelings of sadness due to loneliness, separation from family, and peers, for the same reasons adult family members are also worried [17]. Parents have also noticed what children experience, even if they are not infected or quarantined. For example, a study of family mental health during the H1N1 (commonly known as swine flu) epidemic showed that 30 percent of children experienced post- traumatic stress simply by being in an epidemic environment, feeling constant concern and fear from other family members [18]. Another study conducted during the SARS epidemic showed that children's concern and sense of loss of self-protection, when at least one parent becomes ill, causes significant psychological instabilities [16]. However, none of the previous epidemic episodes has had such a wide global pandemic scale as COVID-19, causing massive changes in society, affecting people of all ages, regardless of whether they were directly affected by the disease or not.
The United Nations (UN) Educational, Scientific and Cultural Organization stated that school closures affected 862 million children and youth—about half of the world's students [19]. This has led many physicians and scientists to express concern about the potential psychological impact of the COVID-19 pandemic, particularly on children and adolescents [9,20]. People aged 18-35 and 35-59 experience a similar number of concerns, however people aged 60 ≥ have significantly less concerns than younger participants [21].
Moreover, emerging evidence from developmental psychology suggests that potential effects will vary greatly depending on the age of the child and the socio-demographic characteristics of the family. So, this means that the decisions taken by the government regarding the measures for COVID-19 in the society will affect different age groups of children differently. School closures have a major impact on children aged five and under 18, while other measures affect younger, pre- school age groups. Consequently, infants and young children may be more affected indirectly by the stress that COVID-19 places on their parents, and there is evidence that, over time, parental stress may generally be associated with behavioral problems in the developing child [22] and children with developmental disabilities [23].
Loneliness is increasingly recognized as a major public health problem, particularly damaging to the young, and can also lead to premature deaths in old age [24,25]. Loneliness is associated with feelings of emptiness, sadness and shame, alongside the subjective perception that a person is disconnected, isolated from others. Like social isolation, loneliness is also associated with depression [26], increased cortisol levels in the body [27,28], decreased immunity, and the resulting increase in the duration and frequency of hospitalization. Social isolation and loneliness may be significantly stronger risk factors for suicide than other well-known risk factors such as anxiety and hopelessness [29]. Despite the clear risks of loneliness, psychological support based on cognitive- behavioral principles to date has shown poor results [30]. With the onset of COVID-19, enforced social isolation is likely to exacerbate and exacerbate what is already known to be a significant problem in our society. Added to this is the devastating and understandable anxiety about economic problems and the loss of a loved one in the context of a pandemic. During the coronavirus epidemic, we are forced to deal with death in ways unrelated to human civilization: from the thought of not being able to be with the deceased in the last moments of life, to the guilt of having someone accidentally infected, the torment of not being able to properly honor them with a funeral ceremony, which is the essence of mourning to the process, these are all factors that intensify the pain of death, increase the incidence of depression, alcohol, drugs, and risky behavior, and in extreme cases, suicide [25].
Unexpressed long-lasting stress, anger and increased irritability, nervousness return with additional psychological problems after getting rid of the oppressive situation. Similarly, spending unusual amounts of time together in enclosed spaces, often unsuitable for such purposes, increases the risk of conflict and domestic violence. Those who come out of isolation are also at risk of being stigmatized: they are viewed as potential "plague spreaders" with fear and suspicion.
The concept of psychosomatics and objective methods of studying the effects of stress
Epidemiological studies confirm that those who experience persistent or severe stress over a long period of time report poorer mental and physical health and increased mortality [31]. The association between greater stressor exposure and increased risk of disease has been demonstrated for a wide variety of stressors (eg, discrimination on any basis, mobbing, stress at work) and a number of aging-related factors affecting physical health (eg, cardiovascular disease, metabolic disorders, etc.). The mechanisms underlying these associations have also been detailed [32,33], (Figure 1). The figure shows that stressors are experienced in the various situations within the context of a person's life and overall situation around, which could have an impact for the health outcomes. All pathophysiological mechanisms stand in between initial and all subsequent steps moderating the individual’s response with triggering effect to moderate the outcomes [31].
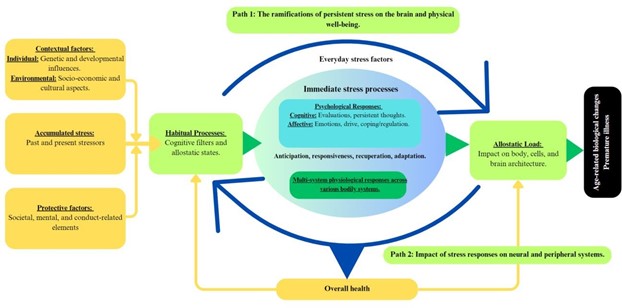
Figure 1: Impact of stress within pathophysiology mechanisms (Adapted from Epel et al., 2018 [31]).
Despite compelling evidence, health researchers often measure stress using unvalidated measures or choose inappropriate methods, without considering the objective circumstances or factors involved in the onset, progression, and appropriate assessment of stress itself and its links to physiological conditions [34].
Psychosomatic medicine is an interdisciplinary field of medicine that studies the relationship of social, psychological, and behavioral factors with bodily processes and the quality of life of humans and animals. Psychosomatic medicine integrates interdisciplinary assessment and management involving multiple specialties, including psychiatry, psychology, neurology, psychoanalysis, internal medicine, pediatrics, surgery, allergy, dermatology, and psychoneuroimmunology. Clinical situations where mental processes act as a major factor influencing medical outcomes are areas where psychosomatic medicine plays a leading role (Cambler et al., 2022).
Exposure to stress can be measured using self-administered questionnaires, such as the Life Events Checklist, which is rated by an interviewer, or objectively determined based on a recent event (eg, living in New York City during the 9/11 terrorist attacks). An individual's response to a stressor is sometimes multifaceted, especially when it comes to the impact of the stressor on physical health, such as caring for a sick family member, illness is often considered a chronic stressor because it requires constant physical and emotional strain [34].
Laboratory indicators of stress
Classical biomarkers of stress include endocrine changes, particularly the cycling of hormones such as cortisol and epinephrine [35,36]. It is the hypothalamic-pituitary-adrenal system, together with the autonomic nervous and immune systems, that becomes sensitive and immediately responds to changes in peripheral stress by measuring such well-known biomarkers of stress as cortisol, alpha amylase, pro-inflammatory cytokines [35,36]. According to the application, stress markers can be classified into diagnostic, prognostic and therapeutic. Diagnostics are those that help diagnose or identify a disease. Prognostic markers help predict the course of the disease. Therapeutic - to monitor treatment and apply to prevent disease progression [37]. In a general sense, tests of secretory cortisol, alpha amylase and immunoglobulin are considered primary in clinical practice to assess whether the body shows a non-specific response to the stressor. The obtained results are always interpreted by the doctor, providing conclusions or references specific to the obtained laboratory data [37].
By studying all three stress indicators simultaneously and evaluating their changes, we can answer questions related to the nature of stress: acute or chronic; adaptation to the experienced impact: adaptation or exhaustion period; the strength of the stress experienced or the response to it; detect symptoms characteristic of endocrine (hypo-reduced adrenal function, hyper-increased function) or neurological (impaired functions of the vegetative system) pathology, etc. [38].
Some secretory biomarkers (cortisol, alpha-amylase, pro-inflammatory cytokines) have been developed as stress biomarkers reflecting both ANS and HPA activity. Among the various factors belonging to the neuroendocrine axis, cortisol plays a crucial role in the stress response. There are many works justifying the role of secretory cortisol in the diagnosis of diseases [39], i.e. in assessing somatic conditions or distinguishing purely psychological causes.
Because chronic stress can also weaken the immune response, as evidenced by the study of antibody responses to vaccines, it can cause or contribute to various diseases such as cardiovascular, endocrine, gastrointestinal diseases, and more. The scientific literature indicates that severe stress can also alter the levels of different immune factors by increasing them [8], increased cortisol levels lead to HPA hyperactivity, and the latter disorders increase the risk of various diseases [39]. Meanwhile, alpha-amylase, which reflects the state of the autonomic nervous system and, depending on the context of the study, i.e., whether there was only acute stress due to somatic illness or whether pharmacological agents were used, can be applied in principle to study ANS activity, may therefore be a suitable biomarker for the assessment of ANS in the context of behavioral medicine.
Conclusion
Various age groups perceive stress very differently [40-43]. An isolation for up to 10 days can cause long-term psychiatric symptoms, with potential residual post-traumatic stress disorder even three years or more after the stress has passed [2]. Because of the impact of long-lasting PTSD (Post Traumatic Stress Disease) outcomes after Covid 19 outbreak the investigation of psychological status is still on time. The review results suggest the lack of evidence of objective diagnostics methods to investigate stress level, duration, other impact for health with perception of possibilities for complex approach of various methodologies, including laboratory stress indicators tests in combination with the PSS research method for optional stress investigation.
References
- Bosqui T, Marshoud B. Mechanisms of change for interventions aimed at improving the wellbeing, mental health and resilience of children and adolescents affected by war and armed conflict: A systematic review of reviews. Conflict and Health, 2018; 12: 15. doi: https://10.1186/s13031-018-0153-1
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the Lancet, 2020; 395(10227) MEDLINE®/PubMed®, a database of the U.S. National Library of Medicine.
- Jeong H, Yim HW, Song Y-J. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health, 2016; 38: e2016048.
- Jin Y, Sun T, Zheng P, An J. Mass quarantine and mental health during COVID-19: A meta-analysis. J Affect Disord, 2021; 295: 1335-1346. doi: 1016/j.jad.2021.08.067.
- Webster R, Brooks S, Smith How to improve adherence with quarantine: Rapid review of the evidence. medRxiv, 2020. https:// DOI: 10.1101/2020.03.17.20037408
- Bhatnagar S, Kumar S, Rathore P, Sarma R, Malhotra RK, Choudhary N, et al. Surviving COVID-19 is Half the Battle; Living Life with Perceived Stigma is Other Half: A Cross- Sectional Study. Indian J Psychol Med, 2021; 43(5): 428-435. doi: 1177/02537176211029331.
- Prem K, Liu Y, Russell TW, Kucharski AJ, Eggo RM, Davies N, et al. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling The Lancet Public Health. Lancet, 2020; 14; 395(10227): 912-920.
- Liu X, Luo WT, Li Y, Li CN, Hong ZS, Chen HL, et al. Psychological status and behavior changes of the public during the COVID-19 epidemic in Int. J. Environ. Res. Public Health, 20209; 17(8479): 18-19.
- Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in Int. J. Environ. Res. Public Health, 2020; 17: 1729.
- Zheng L, Miao M, Gan Perceived control buffers the effects of the covid-19 pandemic on general health and life satisfaction: the mediating role of psychological distance. Appl Psychol, 2020. https://doi.org/10.1111/aphw.12232
- Leigh-Hunt N, Perry A. A Systematic Review of Interventions for Anxiety, Depression, and PTSD in Adult Offenders. International Journal of Offender Therapy and Comparative Criminology, 2015; 59(7): 701-725. https://doi:10.1177/0306624X13519241
- Xia CH, Ma Z, Ciric Linked dimensions of psychopathology and connectivity in functional brain networks. Nat Commun, 2018; 9: 3003. https://doi.org/10.1038/s41467-018-05317-y
- Palgi Y, Shrira A, Ring L. The loneliness pandemic: Loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 J Affect Disord, 2020; 275: 109-111. https://doi: 10.1016/j.jad.2020.06.036
- Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental International Journal of Social Psychiatry, 2020; 66(4): 317-320. https://doi:10.1177/0020764020915212
- Smith M, Steinman L, Casey Combatting social isolation among older adults in the time of physical distancing: the COVID-19 social connectivity paradox. Front Public Health, 2020. https://doi.org/10.3389/fpubh.2020.00403
- Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of Can. J. Psychiatry, 2009; 54: 302–311.
- Petrosillo N, Viceconte G, Ergonul O, Ippolito G, Petersen E. COVID-19, SARS and MERS: Are they closely related? Microbiol. Infect, 2020; 26: 729–734.
- Sprang G, Silman Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Med Public Health Prep, 2013; 7(1): 105-110. https://doi: 10.1017/dmp.2013.22. PMID: 24618142.
- Viner RM, Russell SJ, Croker H, Packer J, Ward J, Stansfield C, et al. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child. Adolesc. Health, 2020; 4: 397–404.
- Ghosh R, Dubey MJ, Chatterjee S, Dubey S. Impact of COVID-19 on children: Special focus on the psychosocial aspect. Minerva Pediatr, 2020; 72: 226–235.
- Castellano-Tejedor C, Torres-Serrano M, Cencerrado A. Psychological impact in the time of COVID-19: A cross-sectional population survey study during confinement. J Health Psychol, 2022; 27(4): 974-989. doi: 10.1177/1359105320985580.
- Mackler JS, Kelleher RT, Shanahan L, Calkins SD, Keane SP, O'Brien M. Parenting Stress, Parental Reactions, and Externalizing Behavior from Ages 4 to 10. J Marriage Fam, 2015; 77(2): 388-406. https://doi: 10.1111/jomf.12163.
- Sanner CM, Neece Parental Distress and Child Behavior Problems: Parenting Behaviors as Mediators. J. Child. Fam. Stud, 2018; 27: 591–601. Int. J. Environ. Res. Public Health 2020; 17(8479): 17-19.
- Yang H, Bin P, He AJ. Opinions from the epicenter: An online survey of university students in Wuhan amidst the COVID-19 J. Chin. Gov, 2020; 5: 234–248.
- Dunbar M, Mineyko A, Hill M, Hodge J, Floer A, Kirton Population Based Birth Prevalence of Disease-Specific Perinatal Stroke. Pediatrics, 2020; 146(5). https://doi: 10.1542/peds. PMID: 33115795.
- Cacioppo JT, Cacioppo Social relationships and health: the toxic effects of perceived social isolation. Soc Personal Psychol Compass, 2014; 8(2): 58–72. https://doi.org/10.1111/spc3.12087
- Hawton A, Green C, Dickens AP, Richards SH, Taylor RS, Edwards R, et al. The impact of social isolation on the health status and health-related quality of life of older people. Qual Life Res, 2011; 20(1): 57-67. https://doi: 10.1007/s11136- 010-9717-2.
- Matthews T, Danese A, Wertz J, Odgers CL, Ambler A, Moffitt TE, et al. Social isolation, loneliness and depression in young adulthood: A behavioural genetic Soc. Psychiatry Psychiatr. Epidemiol, 2016; 51: 339–348.
- Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci, 2015; 10(2): 227-237.
- Almayahi ZK, Al Lamki N. Psychological effects of, and compliance with, self-isolation among COVID-19 patients in South Batinah Governorate, Oman: a cross-sectional study. Egypt J Neurol Psychiatr Neurosurg, 2022; 58(1): 45. doi: 10.1186/s41983-022-00481-x.
- Epel E, Crosswell A, Mayer S, et More than a feeling: A unified view of stress measurement for population science. Frontiers in Neuroendocrinology, 2018; 49: 146–169.
- Boyce WT. Epigenomics and the unheralded convergence of the biological and social sciences. In: Kaplan R, Spittel M, David DH (eds) Population Health: Behavioral and Social Science Insights. Rockville, MD: Agency for Healthcare Research and Quality and Office of Behavioral and Social Sciences Research, National Institutes of Health, 2015; pp219-232.
- McEwen BS. The brain on stress: How behavior and the social environment “get under the skin.” In: Kaplan R, Spittel M, David DH (eds) Population Health: Behavioral and Social Science Insights. Rockville, MD: Agency for Healthcare Research and Quality and Office of Behavioral and Social Sciences Research, National Institutes of Health, 2015; pp. 233–250.
- Crosswell A, Lockwood K, Best practices for stress measurement: How to measure psychological stress in health research. Health Psychol Open, 2020; 7(2): https://doi:org/ 10.1177/2055102920933072.
- Ewert A, Chang Levels of nature and stress response. Behav. Sci, 2018; 8: 49. https://doi: 10.3390/bs8050049
- Takahashi S, Nakasatomi M, Takei Y, Ikeuchi H, Sakairi T, Kaneko Y. Identification of urinary activin A as a novel biomarker reflecting the severity of acute kidney Sci. Rep, 2018; 8: 5176. https://doi: 10.1038/s41598-018-23564-3
- Dhama K, Latheef SK, Dadar M, Samad HA, Munjal A, Khandia R, et al. Biomarkers in Stress Related Diseases/Disorders: Diagnostic, Prognostic, and Therapeutic Values. Front Mol Biosci, 2019; 18(6): 91. https://doi.org/10.3389/fmolb.2019.00091.
- Valantukevičius B, Seibokaite A, Sepetiene Streso indikatoriai, jų reikšmė ir pritaikymas šiuolaikinėjė ligų diagnostikoje. Lietuvos bendrosios praktikos gydytojas, 2020; T.24; Nr 3.
- Spiljak B, Vilibić M, Glavina A, Crnković M, Šešerko A, Lugović-Mihić L. A Review of Psychological Stress among Students and Its Assessment Using Salivary Biomarkers. Behav Sci (Basel), 2022; 12(10): 400. doi: 3390/bs12100400.
- Zhu X, Upenieks L. Age Differences in Mental Health During the COVID-19 Pandemic: Assessing the Moderating Role of Attachment to God. J Aging Health, 2022; 8982643221112141. doi: 10.1177/08982643221112141.
- Jeong H, Yim HW, Song Y-J. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health, 2016; 38: e2016048.
- American Psychiatric Anxiety disorders. In Diagnostic and statistical manual of mental disorders (5th ed.), 2013. https://doi.org/10.1176/appi.books.9780890425596.dsm05
- Rubin GJ, Wessely S. The psychological effects of quarantining a city. BMJ, 2020; 368: m313.

