The Relationship Between Food Pattern and Medical Problems and Gestational Weight Growth in the Third Trimester
Remya Paul Mukkathu*, Alona Claris Joseph, Athira Mol P R, Padmasree P S
Department of Dietician, Caritas Hospital, India
Received Date: 13/05/2023; Published Date: 04/09/2023
*Corresponding author: Remya Paul Mukkathu, Department of Dietician, Caritas Hospital, Kerala, India
Abstract
It is crucial for women to consume a balanced diet during the gestation period for both her own health and the best possible development of the foetus. A child’s good growth and development, which in turn leads to a productive and healthy life in later years, depend largely on adequate nutrition during the “critical window of opportunity” in the first 1000 days. Total weight gain during pregnancy, which is obviously determined and impacted by maternal nutritional intake during pregnancy, is one of many elements that determine foetal growth as a result of overall pregnancy status. One of the best indicators of a successful pregnancy is observing a mother’s adequate weight growth. Predicting new born and mother morbidity and death using weight gain during pregnancy is crucial. Other factors like PCOD, hypothyroidism, GDM can also play a role in excessive weight gain. The present research focuses to study more about factors that causes excessive weight gain during pregnancy.
Introduction
The condition of carrying a growing foetus inside a woman's body is called pregnancy. It is also known as the gestational period. From the moment of conception until birth, it begins. The typical gestation period for humans is 40 weeks. According to Rolfes et al. (2009) [1], pregnancy is frequently broken up into three trimesters, each lasting three months. Pregnancy is a special time in life that has a lot of potential to affect both the health of the mother and the unborn child. Significant physiological changes occur during pregnancy, and these changes necessitate a healthy and ideal diet. The placenta secretes several hormones that cause these modifications to take place. During pregnancy, food must be nutrient-dense and abundant in all the necessary macro- and micronutrients. (2007) Insel et al [2].
Maternal and child health are extremely important factors influenced by nutrition. From the moment of conception until the time of birth, a baby's growth and development are totally dependent on the mother's nutrition. The complex time of rapid fetal growth requires a rise in nutrients from the mother's diet, including macronutrients and micronutrients. The cornerstone of long-term health is optimal nutrition during the early stages of life. The risk of maternal, fetal, and long-term consequences for the growing baby is decreased by a healthy maternal nutrition intake and dietary pattern that includes nutrient-dense meals, proper maternal body composition, and the provision of nutrients through the placenta.
The nutritional health of the mother, as assessed by her pre-pregnancy weight and Body Mass Index (BMI), has an impact on both the mother and her fetus at every stage of the reproductive cycle, from conception on through the whole gestation period and nursing. Gestational weight gain, one of many factors that affect fetal growth and pregnancy outcomes, is an indicator of overall fetal growth and pregnancy status and is obviously influenced by maternal dietary and nutrient intake throughout the entire course of gestation (Paturi et al., 2008) [3].
One of the greatest indicators of a successful pregnancy, particularly in terms of the newborn's birth weight, is enough weight growth during the course of the three trimesters for a nine-month period (ADA Report, 2002) [4]. Throughout the first trimester, her diet should permit a weight increase of 0.9 to 1.8 kg, followed by weekly weight gains of 0.3 to 0.5 kg throughout the second and third trimesters (Wardlaw et al., 2004) [5]. The typical total weight increase objective for women of normal weight is 11.5 to 16 kg. The target weight for underweight women rises to 12.5 to 18 kg, whereas it drops to 7 to 11.5 kg and 5 to 9 kg for overweight and obese women, respectively. (IOM, 2009) [6].
Objectives
- To assess the dietary pattern of the expectant mothers.
- To assess the correlation between unhealthy weight gain and food pattern.
- To assess the correlation between unhealthy weight gain and other factors like GDM and PCOD.
Review of Literature
Weight gain during pregnancy:
An important factor in determining the size of the fetus is the weight gain over the course of pregnancy. Low birth weight (LBW), defined as a birth weight of less than 2.5 kg, and intrauterine growth retardation (IUGR) are both significantly increased by inadequate prenatal weight gain. Preterm birth risk is enhanced when the third trimester of pregnancy sees inadequate maternal weight growth.
Neonatal birth weight is significantly influenced by the mother's pre-pregnancy weight, the pattern of weight growth throughout gestation, and the overall weight gain associated with pregnancy. According to Mamun et al. (2009) [7], birth weight appears to have an influence on early adult weight as well as long-term health and neonatal morbidity and mortality.
Most women gain weight when they are pregnant. There are, however, rare instances in which some women either do not gain any weight at all or even lose weight; in these cases, the fetal growth is thought to be occurring at the expense of the mother. Weight gain has both fetal and maternal components; the fetal component (related to growth of the fetus, placenta, and amniotic fluid) occurs in the third trimester, while the maternal component (due to expansion of blood volume, growth of the uterus, growth of the breast, and fat storage) occurs in the second trimester. (2000) Robinson et al [8].
Regular monitoring of weight growth throughout pregnancy is necessary from the outset until delivery. If the mother's weight growth falls within the IOM-recommended parameters, the infant's birth weight improves. A pregnant woman can determine how much to modify her food and nutritional consumption during the gestational period by keeping weekly records of her weight gain.
Obesity-related weight gain increases the risk of gestational hypertension, diabetes mellitus, toxaemia, and eclampsia. Additionally, the need for surgery and other difficulties after childbirth increase. These pregnancies need close observation during the whole gestation period and are associated with a higher risk of birth abnormalities in the offspring, partly because the fetus can develop into a very large size. Low birth weight is frequently caused by inadequate weight growth, especially in underweight mothers (BMI 18.5 kg/m2). Women who are malnourished frequently consume too little iron and calcium and need to increase their body reserves. By the conclusion of the first trimester of pregnancy, they should attempt to reach a healthy weight (BMI 18.5-22.9 kg/m2) (Gordon and Wardlaw, 1999) [9].
Obesity in mothers increases the chance of developing a number of cardiovascular illnesses in the future. A 2013 study from India looked into the relationship between certain pregnancy problems and the risk of cardiovascular disease during the following ten years. After 3–8 years postpartum, the associations between obesity markers, including BMI, WC, and W/H ratio, and pregnancy problems were investigated. It was shown that women who had diabetes, hypertension, or any other pregnancy issue had an elevated risk of cardiovascular illnesses at age 10 years.
Therefore, pregnancy is the perfect time to spot women who may be at risk for cardiovascular disease at a young age. Since being overweight or obese causes a woman's metabolism to change, this might have a negative impact on the outcome of the pregnancy (Meenakshi et al., 2012). However, issues, including intrauterine development retardation, might arise from acquiring less weight during pregnancy (Alwani et al., 2015). In light of this, enough GWG is a crucial factor in determining pregnancy outcomes. The goal of prenatal treatment should be to help women acquire a healthy weight before getting pregnant and maintain that weight during pregnancy.
Pregnancy and Physical Activity
Pregnant women typically engage in less physical activity (Amezcua Prieto et al., 2013; Hegaard et al., 2011). They are recommended to reduce their exercise levels during pregnancy since it is considered a vulnerable time (Hammer et al., 2000).
Pregnancy and Diet
For pregnant and nursing women, the national health site of India has provided specific dietary recommendations. As the pregnancy advances, so does the nutritional need; therefore, food should be sufficient and attention should be paid to ensuring its nutritional sufficiency (Greenberg et.al., 2011, Chitayat et.al., 2016).
Obstacles to dietary choice during pregnancy and nursing were highlighted in a 2018 analysis by Kavle and Landry in low- and middle-income nations. Most of the research considered obstacles including cultural views about pregnancy (knowledge about food intake, weight gain, and "eating down" to avoid giving birth to a huge baby). Foods deemed improper for ingestion were linked to dietary restrictions. The choice of food was influenced by the emergence of an aversion to it, budgetary limitations, and the ease with which food was accessible. Rarely was there any diet or weight gain during pregnancy guidance provided. They concluded that there aren't many initiatives encouraging a healthy diet for pregnant women and GWG. This necessitates the creation of well-thought-out and socially acceptable nutrition recommendations for expectant mothers and lactating women.
Pregnancy Weight Gain Recommendations
General Weight Gain Recommendations
Less than half of a normal-weight pregnant woman's entire weight increase throughout a singleton gestation is stored in the fetus, placenta, and amniotic fluid. The remaining portion is found in the uterine and breast tissues of the mother, as well as in interstitial fluid, blood volume, and adipose tissue. Increased subcutaneous fat in the back, upper thighs, and belly acts as a reservoir of energy during pregnancy and nursing. By pre-pregnancy BMI, different weight increases are advised to ensure a healthy pregnancy.
Obesity Weight Gain Recommendations
There are three categories of prenatal obesity: class I (BMI 30 to 34.9), class II (BMI 35 to 39.9), and class III (BMI greater than 40). These groups are not distinguished by the IOM's recommended weight increase range of 11 to 20 pounds. Research is ongoing, but there is some indication that lesser growth, or even loss, can be effectively managed since people may balance their diets well enough to prevent ketonemia. Optimal gestational weight gains for these populations are yet unknown. Obesity is linked to reduced blood levels of carotenoids, vitamins C, D, B6, K, folate, iron, and selenium, proving that being overweight and then overeating are not the same thing.
Fetal growth must be monitored, and individual counseling and clinical judgment are required, including optimizing food intake and promoting activity (ACOG, 2013a) [10,11]. Certain research indicates that if weight growth is excessively restricted, the risk of preterm birth, IUGR, and neonatal mortality all rise; long-term implications must also be considered. Weight gain objectives may be too high for certain women.
Methodology
This chapter covers the specifics of the sample and sampling techniques, the study's conceptual framework, and the statistical techniques applied to the data analysis.
Study design:
The present study is survey research. One to one interview method of survey research was used in this study. According to Frances et.al.,2009, one to one interview is valuable method of collecting rich in-depth data about participants experiences and perspectives.
Selection of sample:
Simple random sampling method is used for the selection of samples. 299 antenatal women at third trimester attending hospital and who were willing to participate were randomly selected for the study.
Data collection:
One to one interview method was used to collect data. During planning the interview schedule, the study's goals and conceptual framework were taken into consideration.
Anthropometric measurements including height, pre-pregnancy, and present weight, from these data BMI has been calculated. Dietary assessment is done based on food frequency method.
Statistical analysis:
The recorded data were statistically analysed. Categorical and quantitative variables were expressed as frequency (percentage) and mean ± SD respectively. Chi square test is used to determine the correlation of weight gaining with other variables like PCOD, GDM, physical activity and dietary pattern.
Result
Descriptive statistics
Table 1: Background characteristics.
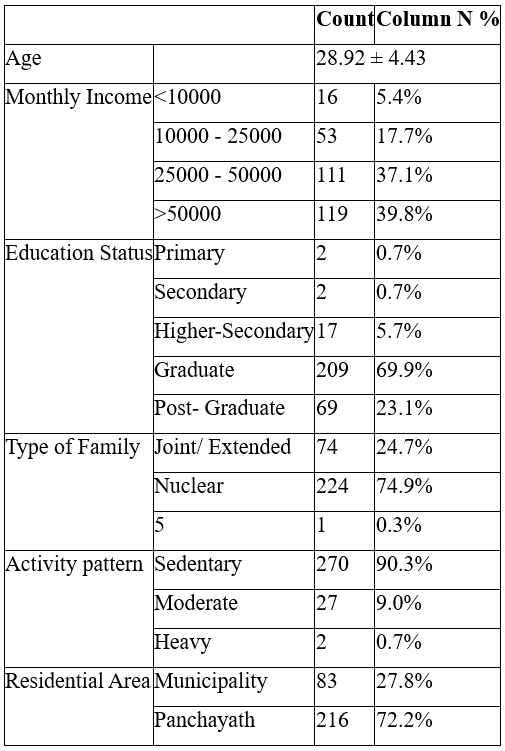
The above table shows the mean age of selected antenatal mothers were 28.92±4.43. The monthly income of majority of selected expectant mothers were above 25,000. About 93% of them were either graduated or post graduated. Three-fourth of them were from nuclear family. Ninety percent of them were leading a sedentary life style. More than 70% of them were from panchayath area.
Table 2: Co-morbidities and family history of selected antenatal mothers.
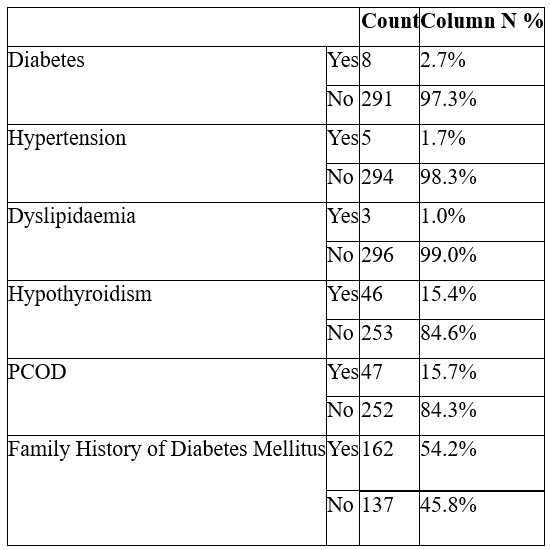
Among the selected 299 expectant mothers 8 were diabetic, 5 were hypertensive, 3 were dyslipidemia, 46 were having hypothyroidism and 47 were having PCOD. More than half of them were having a family history of diabetes.
Table 3: Food frequency of antenatal mothers.
Table 3.1: Food frequency of CHO rich foods.

About 88% of the selected expectant mothers were taking whole grains at least thrice a week. Less than one-fourth of the selected expectant mothers were not taking refined cereals or taking it only rarely. Around 19% of the selected expectant were taking sugar items at least once in a week. About one-fourth of the expectant mothers were taking roots and tubers at least thrice a week.
Table 3.2: Food frequency of protein rich foods.
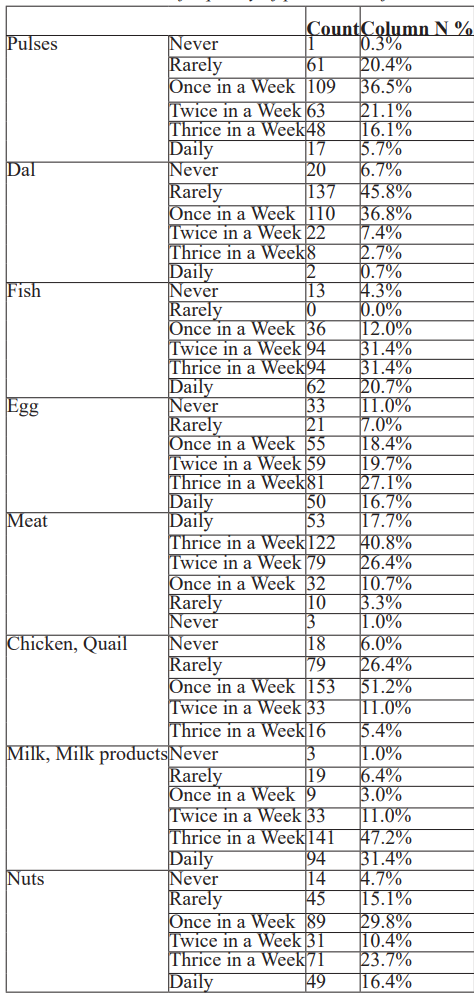
When looking into protein rich foods, about 80% among the selected expectant mothers were taking pulses at least once a week. About half of them were not taking dhal or taking it rarely. Half of them were consuming fish at least thrice in a week. More than 80% of the selected antenatal women were taking egg at least once in a week. Only around 4% of them were avoiding or rarely taking red meats. Around 67% of the antenatal women were consuming chicken/quail at least once in a week. Milk and milk products were consumed by more than 90 percent of the antenatal women at least once in a week. About 80% of the antenatal women were taking nuts at least once in a week.
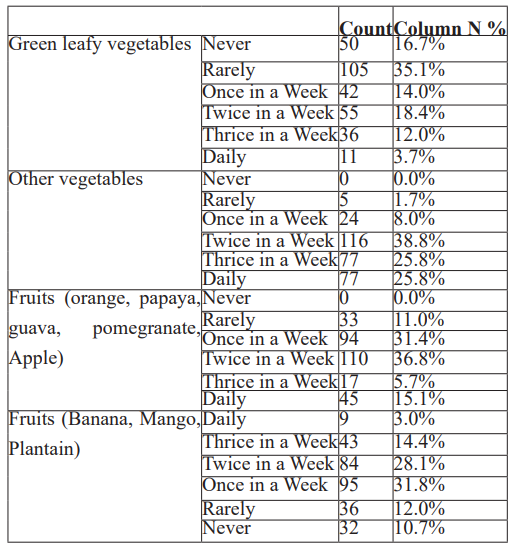
About half of the antenatal women were avoiding or rarely taking green leafy vegetables. About half of them were taking other vegetables at least thrice in a day. Ninety percent of them were taking fruits (like orange, papaya, guava, pomegranate, apple) at least once in a week. More than 20% of them were avoiding or rarely taking fruits like banana, mango, plantain.
Table 4: To analyze the correlation between the PCOD and weight gain.
Independent Samples Test
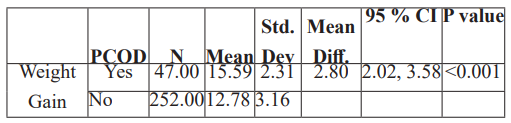
Statistical analysis shows that the correlation between weight gain and PCOD is highly significant.
Table 5: To analyze the correlation between food frequency table and weight gain.
Table 5.1: Correlation between CHO rich foods and weight gain.
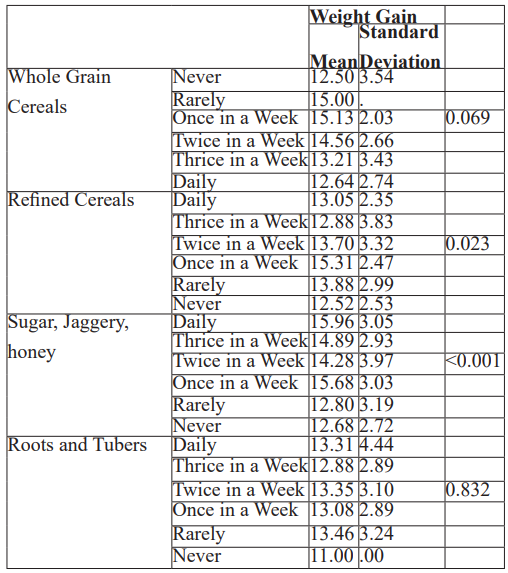
The correlation between the unhealthy gestational weight gain and the consumption of refined cereals and sugar, jaggery, honey is statistically significant.
Table 5.2: Correlation between protein rich foods and weight gain.
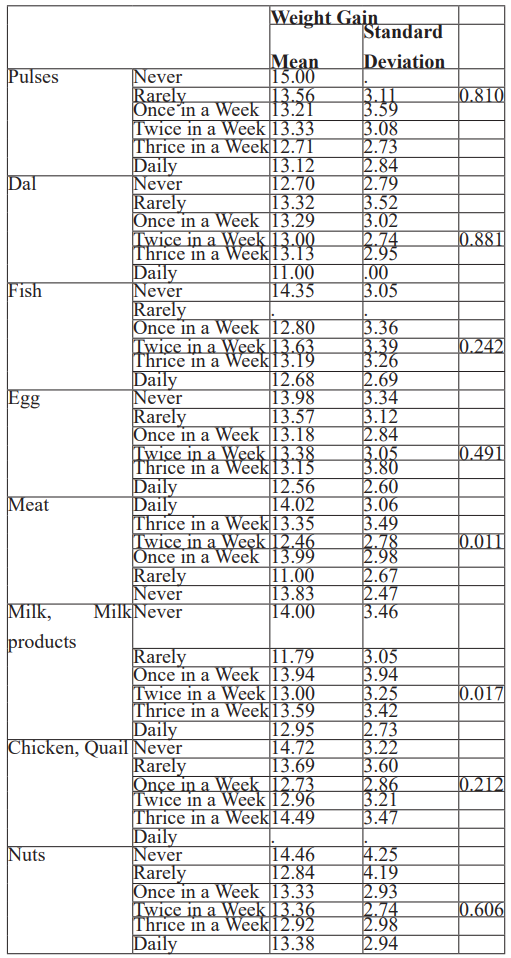
Statistical analysis shows correlation between unhealthy gestational weight gain and consumption of meat and over consumption full fat milk and milk products.
Table 5.3: Correlation between protective foods and weight gain.
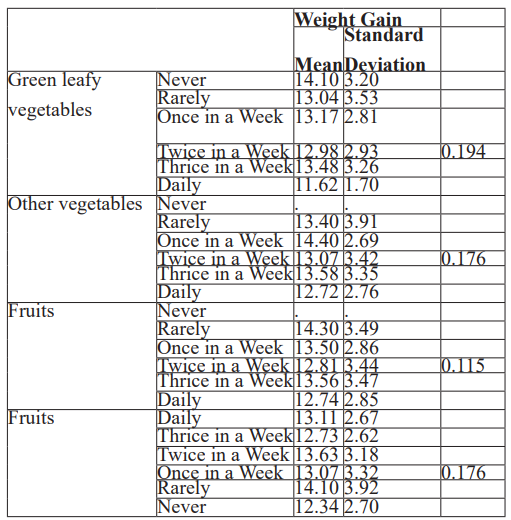
There is negative correlation between protective foods like fruits and vegetables and unhealthy weight gain during pregnancy.
BMI based on pre pregnancy
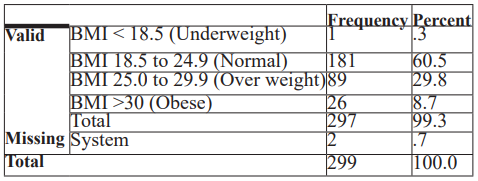
Among the selected 299 antenatal women, according to BMI based on pre pregnancy weight 1 was underweighted, 181 were under normal weight, 89 were overweighted and 26 were obese.
Table 6: To evaluate the weight gain in pregnant women's according to the pregnancy weight gain chart.

When evaluating the weight gain according to pregnancy weight gain chart 36.4% of the expectant mothers were overweighted or obese.
Table 7: To analyse the correlation between the age and weight gain.


According to the statistical analysis it shows that there is negligible correlation with age and pregnancy weight gain.
Table 8: To analyse the weight gain based on the type of activity Report.

The correlation between activity pattern and weight gain is statistically insignificant.
Table 9: To analyse the weight gain of the GDM patients.

Statistical analysis shows that the correlation between weight gain and GDM is highly significant.
Discussion
In the present study the mean age of the antenatal women was 28.92. The study shows correlation between unhealthy foods like refined cereals, meat, sugar items and full fat diary products with unhealthy weight gain during pregnancy. But when looking into fibre rich foods the correlation is negative with excessive weight gaining. So, the consumption of fibre rich foods should be encouraged during pregnancy. The study reveals there is relation between excessive weight gain and PCOD. Same as that, GDM also plays an important role in gaining unhealthy weight during pregnancy.
Conclusion
It is important to regulate gestational weight gain and inform expectant mothers about it since most of the women had excessively high or low total pregnancy weights and mid-pregnancy weights. Both the mother's and the baby's health are impacted by pregnancy and delivery. To assist women in achieving healthy weight gain during pregnancy and healthy weight afterwards, tailored care and education are required before a planned pregnancy, during pregnancy, and after delivery. Women should be encouraged and given help to accomplish these objectives.
References
- Rolfes, S. R., Pinna, K., & Whitney, E. (2009). Understanding Normal and Clinical Nutrition (8th ed.). Lachina publishing house.
- Insel, P., Turner, R.E., & Ross, D. (2007). Nutrition. 3rd edition. Jones and Bartlett Publishers. Pp. 652-659.
- Paturi, P. M., Tapanainen, H., Reinivuo, H., & Pietinen, P. (2008). The National FINDIET 2007 Survey. Publications of the National Public Health Institute.
- American Dietitic Association (ADA) Reports (2002). Nutrition & lifestyle for A Healthy pregnancy outcome. Journal of the American Dietetic Association, 102, 1479.
- Wardlaw, G. M., Hampl, J. S. & Disilverstro, R. A. (2004). Perspectives in Nutrition (6th ed.). Library of Congress Cataloguing in publishing data, 272-83.
- Institute of Medicine (2009). Weight Gain during Pregnancy: Re-examining the Guidelines. Institute of Medicine (US) and National Research Council (US) and Committee to Re-examine. IOM Pregnancy Weight Guidelines, Washington, D. C.
- Mamun, A. A., O’Callaghan, M., Callaway, L., Williams, G., Najman, J., & Lawlor, D. A. (2009). Association of gestational weight gain with Offspring body mass index and blood pressure at 21 years of age: Evidence from a birth cohort study. Circulation, 119, 1720-1727.
- Robinson, C. H., Lawer, M. R., Chenoweth, W. L. & Garwich, A. L. (2000). Normal and Therapeutic Nutrition. New York: Macmillan publishing Company.
- Gordon, M., & Wardlaw. (1999). Perspectives in nutrition (4th ed.). New York: Mc Graw Hill publishers.
- American College of Obstetricians and Gynecologists: ACOG committee opinion No. 549: Obesity in pregnancy, Obstet Gynecol 121:213, 2013a.
- Williams, (2017). William`s Basic Nutrition and Diet Therapy (15th ed.). Library of Congress Cataloging-in-Publication. 447-478.

