PAC Score-IT’s Need in Pediatric Units for Qulaity Nursing Care
Mary Anbarasi Johnson*
Professor, Department of in Pediatric Nursing, CMC Vellore, India
Received Date: 12/02/2023; Published Date: 03/04/2023
*Corresponding author: Mary Anbarasi Johnson, Professor, Department of in Pediatric Nursing, CMC Vellore, India
Abstract
The potential and ability of sick children to withhold the stress during the time of illness is very low and they can deteriorate very rapidly as compared to adults, if the intervention is not done at appropriate time. The sick children presenting to Emergency Services with obvious compromise of the airway, breathing and circulation is transferred to the Intensive Care Unit for further management. Clinical deterioration of children who are not very sick and are subsequently admitted to the wards might have unexpected death or unplanned admission to the intensive care unit. The challenge to prevent unexpected clinical deterioration in the hospital lies in the ability of the health care provider to identify the early warning signs of deterioration and to intervene at the appropriate time. The number of lives thus saved can be extrapolated to the national mortality and morbidity burden contributed by illness and ICU care. Hence any effort should be analysed and the results can be implemented in a resource limited country like India. This article highlights the need for usage of PAC SCORE in pediatric units to ensure quality nursing care, reduce the complications in children and minimise CART calls and PICU admissions.
Keywords: PICU; Cart; PAC Score
Introduction
The inpatient hospital cardiac arrests lack the data collection and analysis. Arrest in Pediatrics can be due to three complications through the inpatient care- respiratory arrest, severe bradycardia, and pulseless cardiac arrest [1]. These conditions are recorded with varied interchangability. In the early 1990s, international experts developed the Utstein style for data reporting of cardiac arrests and resuscitation [2]. The American Heart Association started a National Registry of Cardiopulmonary Resuscitation (NRCPR) to collect a large database of hospital cardiac arrests and13.resuscitation with Utstein style definitions. The outcome measures are all recorded to determine any intervention that could have been done for averting a death. Advances in resuscitation care-like BLS courses in the decade have resulted inincreasing rates of survival for patients with out-of-hospital cardiac arrest [3]. In the in-hospital setting, efforts to improve quality include the use of routine mock codes, post-resuscitation debriefing, and defibrillation machine brought by the specialised code personnel. Code teams respond to sudden arrests that occur in the hospital and resuscitate within the window period of 3-5 min for return of spontaneous circulation. In the hospitalized children, 0.7% to 3.5% of them have cardiopulmonary arrest during the course of stay, with only 15-36% of children surviving the arrest [1].
Despite technological and pharmaceutical advances, the survival rate of the children who have unexpected deterioration after admission has not improved.
This unexpected clinical deterioration can be prevented by the following interventions:
1. The implementation of CART (Cardiac Arrest Resuscitative Team) /an outreach of
the ICU team to resuscitate children with cardiopulmonary arrest and
2. The use of early warning scores. - developed depending on the relevant predictors of clinical deterioration. It is an objective assessment tool that incorporates the clinical manifestations that have the greatest impact on patient outcome.
Background
History of pediatric critical care
Pediatric intensive care has been established as a sub-specialty of medicine over the past two decades. It grew out of a need for increasingly complex pediatric care, long-term management of disease, and advancements in medical and surgical sub-specialties, as well as, life-sustaining therapies [1]. The development of pediatric critical care followed the establishment of pediatric intensive care units or PICUs. The first PICU was opened in Europe by Goran Haglund in 1955 at Children's Hospital of Goteburg in Sweden [2]. Advancements in Neonatology and neonatal intensive care, pediatric general surgery, pediatric cardiac surgery, pediatric anesthesiology lead to its opening because of the need to care for critically ill infants and children. Over the next forty years, hundreds of PICUs were established in academic institutions, children's hospitals, and community hospitals. In 1981, the Society of Critical Care Medicine, SCCM, which express guidelines and standards for adult critical care, recognized pediatric critical care as unique from adults and created a separate section within the SSCM for their care [2]. Other institutes followed throughout the 80's, by 1990 there were multiple training programs, certification available, and sub-board on pediatric critical care [2]. Pediatric critical care is now seen as a multidisciplinary field that includes a team of nurse specialists, respiratory therapists, nutritionists, pharmacists, social workers, physical therapists, occupational therapist, and other medical professionals.
Development of Pediatric Early Warning Score (PEWS)
To reduce the occurrence of second-rate care, improve outcomes, and enhance quality of life, systems to identify adult patients at risk for rapid clinical deterioration were established based on "early warning signs". These signs brought attention to key clinical parameters that, when affected, encouraged emergent intervention. Modified Early Warning System (MEWS) is a tool for nurses to help monitor their patients and improve how quickly a rapidly deteriorating client receives the needed care developed from early warning signs. MEWS helps increase objectivity and communication within hospitals [3].
Discussion
Patients with progressing critical illness can be predicted and prevented, but failure to identify the signs and lack of prompt intervention for patients developing acute and critical illness remain a problem. Care for them is challenging because children may be asymptomatic until critically ill. Pediatric patients have unique characteristics and different clinical parameters for each age group; adult parameters and concepts cannot be applied to the pediatric patient. Children have greater compensatory mechanisms than adults and can maintain a normal blood pressure despite considerable loss of fluid. For example, a child with sepsis or severe dehydration may seem unaffected and the acute condition is often identified only by the affected vital parameters [4]. However, their condition deteriorates quickly once compensation mechanisms are overwhelmed. In one review, sixty-one percent of pediatric cardiac arrests were caused by respiratory failure and twenty-nine percent by shock, which are both preventable and potentially reversible causes [5]. Thus, to ensure timely care for pediatric patients and improve outcomes, systemic assessment of key symptoms and their severity is essential.
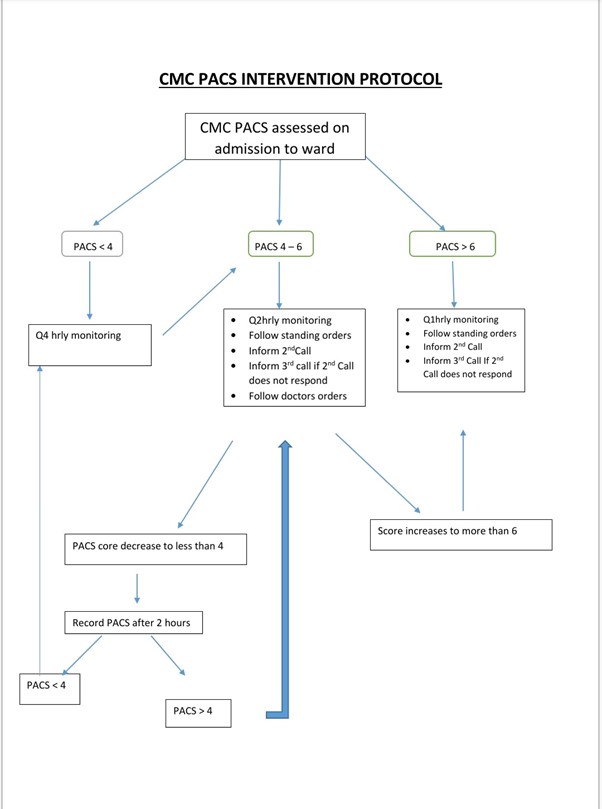
Goals:
- To alert the staff about deterioration in pediatric patients at the earliest.
- To quickly intervene and reduce the mortality rate.
Domains:
The domains in PACS represents major body systems that are sensory to changes in the body and thus create the criteria to be evaluated in a patient to help identify if they are at risk for further deterioration.
The 3 domains are cardiovascular, respiratory and neurological.
Cardiovascular
Heart rate is commonly used in PEWS, as well as, capillary refill. However, only few uses blood pressure because it is not considered as reliable of a measure as the other two. As stated previously, children can maintain a stable blood pressure for much longer than adults. Anatomy and physiology are different in infants and children than adults and vary with age, which produces normal ranges for electrocardiograms. Capillary refill is used across the lifespan as a cardiovascular assessment parameter because it is a non-invasive, quick test to help determine blood flow to the tissues. Heart rate is a crucial piece of assessment in acutely ill pediatric patients because bradycardia may be a sign of conductive tissue dysfunction and lead to sudden death.

Respiratory
Respiratory can be measured by rate, rhythm, characteristics of breathing, and supplemental oxygen use. Different characteristics of breathing are lung sounds, retractions, accessory muscle use, tracheal tug, etc. PEWS uses highly visible and easily monitored characteristics are used, such as retractions, that way there is little variation based on in interpretation. Retractions are a sucking in of the skin around the bones of the chest and illustrate the additional use of muscle to breath, indicated the increased work needed to breath. Similarly, the more supplemental oxygen needed, the less the lungs are providing adequate oxygenation.
Neurological
Behavior is typically measured by playing, sleeping, irritable, and confused or reduced response to pain. This is due to the fact it is an age-based assessment and pediatric patients have some form of "playing" as their age-appropriate norm. Whether it be gurgling and cooing, coloring, or video games, it is age-specific behavior to a younger population. Irritability in children is often a cue that something is wrong, especially in those unable to communicate verbally due to age or disorder. Other scales simply use level of consciousness as they're neurological assessment, instead of behavior
Comorbid factors:
- Oncological conditions
- Immunodeficiency
- Cardiac diseases
- Chronic Lung disease
- Chronic renal disease
- Malnutrition
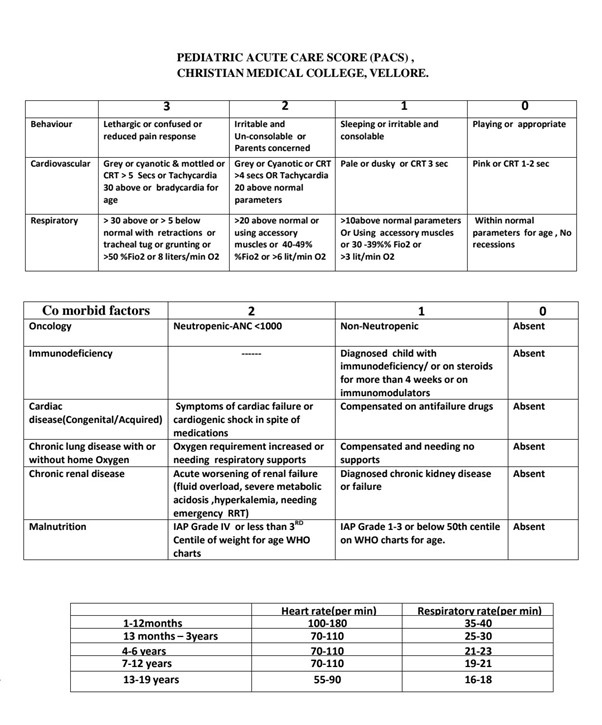
Paediatric Early Warning Score Paediatric Early Warning Score (PEWS) is a tool in which the vital signs or the condition of the patient is given a numerical value which is graded according to the intensity of variation from the normal. It helps in the recoding of the variation of each patient from normal in a short span of assessment, in a single sheet of paper. It can be graded and communicated to other health care professional easily. There are no contraindications and it can be modified based on the local conditions. Other parameters like surgery, cardiac parameters etc can be added.
The concept of PEWS PEWS is a score which increases as the patient variables differ more than the normal values and is high when the child is critical. The scores can depict the severity of illness.
Pediatric Early Warning Signs (PEWS)
PEWS are clinical manifestations that indicate rapid deterioration in pediatric patients, infancy to adolescence. PEWS Score or PEWS System are objective assessment tools that incorporate the clinical manifestations that have the greatest impact on patient outcome. Pediatric intensive care is a subspecialty designed for the unique parameters of pediatric patients that need critical care. The first PICU was opened in Europe by Goran Haglund. Over the past few decades, research has proven that adult care and pediatric care vary in parameters, approach, technique, etc. PEWS is used to help determine if a child that is in the Emergency Department should be admitted to the PICU or if a child admitted to the floor should be transferred to the PICU.
It was developed based on the success of MEWS in adult patients to fit the vital parameters and manifestations seen in children. The goal of PEWS is to provide an assessment tool that can be used by multiple specialties and units to objectively determine the overall status of the patient. The purpose of this is to improve communication within teams and across fields, recognition time and patient care, and morbidity and mortality rates. Monaghan created the first PEWS based on MEWS, interviews with pediatric nurses, and observation of pediatric patients.
Conclusion
Currently, multiple PEWS systems are in circulation. They are similar in nature, measuring the same domains, but vary in the parameters used to measure the domains. Therefore, some have been proven more effective than others, however, all of them have been statistically significant in improving patient care times and outcomes. In CMC Vellore in the Pediatric units we follow the above mentions pediatric acute score which is found to be very beneficial in identifying impending complications in children, so that preventive measures are taken at the earliest and the PICU admissions and CART calls are prevented or minimized.
References
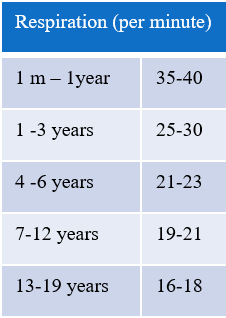
- Agrawal S. Normal vital signs in children: heart rate, respirations, temperature, and blood pressure. Complex Child E-Magazine, 2009; 1-4.
- Akre M, Frinkelstein M, Erickson M, Liu M, Vanderbilt L, Billman G. Sensitivity of the pediatric early warning score to identify patient deterioration. Pediatrics, 2010; 125(4): e763-e769. doi: 10.1542/peds.2009-0338
- Baruteau A, Perry JC, Sanatani S, Horie M, Dubin AM. Evaluation and management of bradycardia in neonates and children. European Journal of Pediatrics, 2016; 175: 151-161. doi: 10.1007/s00431-015-2689-z
- Epstein D, Brill JE. A history of pediatric critical care of medicine. Pediatric Research, 2005; 58(5): 987-996. doi: 0031-3998/05/5805-0987
- Hockenberry M, Wilson D. Wong’s nursing care of infants and children (10th ed.). St. Louis, MO: Elsevier, Mosby, 2015.
- Jensen CS, Aagaard H, Olesen HV, Kirkegaard H. A multicenter, randomized intervention study of the paediatric early warning score: study protocol for a randomized controlled trial. Trials, 2017; 18(267): 1-9. doi: 10.1186/s13063-017-2011-7

