Technical and Ergonomic Considerations: Two Surgeon’s Techniques for Lap Cholecystectomy in Situs-Inversus For a Right-Handed Surgeon
Venu bhargav Malpuri1,*, Krishna Ramavath2, Pranay Palle3 and Kishore Abuji4
1Surgical Gastroenterology, ESI medical college and hospital, Hyderabad, India
2Department of General Surgery, AIIMS, bibinagar, Hyderabad, India
3Department of General Surgery, Gandhi medical college, Hyderabad, India
4Department of General Surgery, Post graduate institute of medical education and research, Chandigarh
Received Date: 04/07/2022; Published Date: 15/07/2022
*Corresponding author: Venu bhargav Malpuri, M. Ch, Assistant Professor, Surgical Gastroenterology, ESI medical college and hospital, Hyderabad, India
Abstract
Laparoscopic cholecystectomy can be technically challenging in patients with situs inversus totalis (SIT). A 39-year male presented with left hypochondriac pain. His cardiac workup showed dextrocardia, and ultrasonography showed a gall bladder on the left side. We used the four-port technique where anterior dissection was carried out by the dominant right hand of the primary surgeon, and the infundibulum was retracted by the first assistant from the mid-clavicular port. The first assistant carries out the posterior dissection through a midclavicular port, whereas the primary surgeon does retraction. To conclude, this two-surgeon technique decreases the ergonomic difficulty faced by right-handed surgeons while performing laparoscopic cholecystectomy.
Keywords: Situs inversus totalis; Dextro-cardia; Laparoscopy; Cholecystectomy
Introduction
Situs inversus totalis is a rare congenital anomaly with an estimated incidence of 1 per 5000-20,000 live births [1-3]. Anatomically, gall bladder is located in the left hypochondrium, posing a diagnostic challenge to clinically suspect symptomatic gall stone disease. Laparoscopic surgery in these patients poses technical challenges, especially for right-handed surgeons, like dissecting calot’s triangle with the non-dominated hand and chances of crossing the arms [1,2]. Another concerning issue in these patients is associated with vascular anomalies, which are common in patients with situs-inversus [4-7]. Despite these concerns, laparoscopic cholecystectomy is the treatment of choice and can be performed safely even in acute cholecystitis patients with situs-inversus [8-11]. In this review, we discussed the technical and ergonomic considerations for safe cholecystectomy in patients with situs-inversus.
Case Report
A 39-year gentleman complained of pain in the left hypochondrium for one month. Ultrasonography revealed a spleen in the right hypochondriac region and gallbladder in the left hypochondriac region, and stones were identified in the gall bladder. Based on ultrasonography findings, diagnosis of symptomatic gall stones was made. His laboratory parameters, ECG, and echocardiography were normal, and he was planned for laparoscopic cholecystectomy. We started the procedure by adjusting the theatre equipment on the left side, mirroring the right side. The primary surgeon and first assistant stood on the patient's right side and the second assistant on the left side. Four ports were used-the; two 10 mm ports were placed in the subxiphoid towards the left and other supra umbilically, respectively. Two 5mm ports were placed in the left hypochondriac region in the left midclavicular line and left anterior axillary line at the level of the umbilicus. An open technique created Pneumoperitoneum by the surgeon standing on the patient's left side. The abdomen was inspected, and a gall bladder was found on the left side.
Technical Aspects
The second assistant standing on the left retracted the fundus of the gall bladder to prevent a crossover of the arms of the operating surgeon fundus of the gall bladder was retracted by the first assistant. By using the Maryland dissecting forceps calot’s triangle was dissected, the anterior fibrofatty layer was dissected by the primary surgeon [Figure-1(G)], and posterior dissection was carried out by the first assistant to prevent cross over of the arms [Figure-1 (H)]. Once calot’s triangle was dissected, and a critical view of safety was achieved, the cystic artery and the cystic duct were clipped and divided. The gall bladder was dissected from the liver surface using hook diathermy by the first assistant, and traction was given by the primary surgeon [Figure-2]. The gall bladder was delivered from the epigastric port, closed ports using non-absorbable sutures.
The total operating time was 60 minutes, and the postoperatively patient was discharged the next day following surgery. Postoperatively no complications were noted to date.
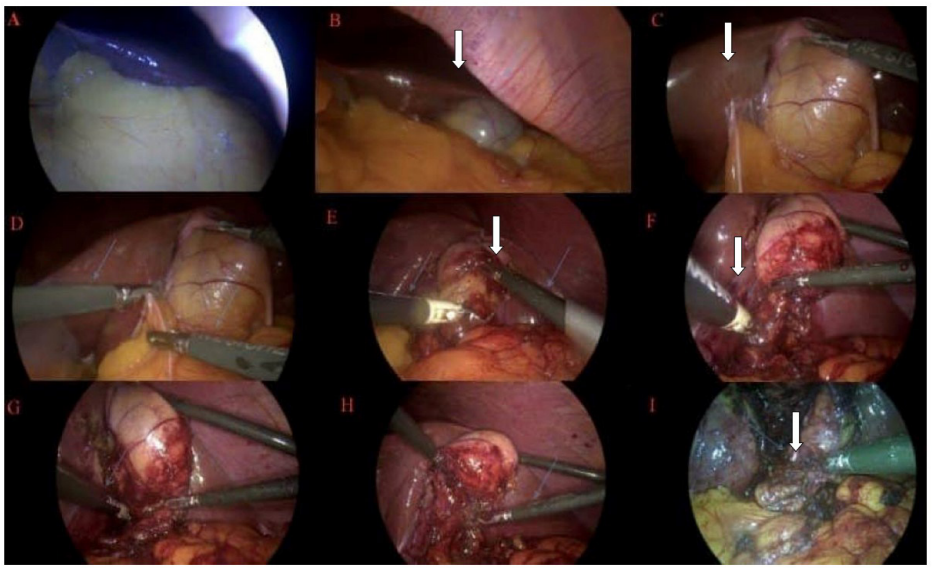
Figure 1: A, B, and C: Left-sided location of the liver and gall bladder, D, E, F, G: Right hand of the primary surgeon using Maryland for separating adhesions while retraction by the assistant, H: posterior dissection is being done by the right hand of the assistant surgeon using Maryland dissecting forceps, I: arrow showing cystic duct

Figure 2:
A and B: Image show the acritical view of safety
C: Clipping of the cystic duct and cystic artery
D: Separating gall bladder from the liver bed by the first assistant using hook diathermy
Discussion
The right-handed surgeon might experience technical difficulties while performing the laparoscopic cholecystectomy in situs inversus totalis patients. The difficulty might be due to a) difficult adhesiolysis with the non-dominant hand, b) constant mental orientation of the anatomy c) crossover of the hands while dissecting the calot’s triangle [12-16]. Dissection of the calot’s triangle would be easier for a left-handed surgeon than a right-handed surgeon [17-20].
Many techniques are described to decrease the difficulty, like the four-port technique, the French position of the operating surgeon, frequent changes in instruments between two arms, retracting infundibulum through the sub-xiphoid port, and port relocation [21-26]. These techniques, even though useful, could not prevent crossover of the arms leading to an abnormal posture for the surgeon.
To avoid difficult dissection, two surgeon’s techniques can be followed, where the primary and the first assistant use the dominant right hand [6,25,27,28]. However, the problem with this technique is it requires good coordination among the operating surgeons, preventing abnormal posture for the operating surgeon [29]. In this technique, the primary surgeon dissects the calot’s triangle with his dominant hand while the infundibulum is retracted by the first assistant and the fundus by the third assistant [30-32]. The first assistant carries out posterior dissection while the operating surgeon retracts the infundibulum. Dissection by the left hand from the sub-xiphoid port makes the instrument lose its perpendicular and narrow angles, making dissection difficult [32]. However, this problem can be overcome by doing anterior dissection alone from the dominant right hand of the right-handed surgeon and posterior dissection by the first assistant through the mid-clavicular port [33]. Advantages of this technique include using the dominant hand by the surgeons, preventing abnormal postures when the surgeon is standing to the patient's left, and simplifying the procedure ergonomically. Bile duct injuries following laparoscopic cholecystectomy have been rarely reported and can be prevented using similar techniques described when the gall bladder is on the right side [34,35].
Conclusion
To conclude, laparoscopic cholecystectomy is the gold standard even when situs inversus is present. Two surgeon techniques can decrease the ergonomic difficulties faced by the right-handed surgeon. However, to standardize these techniques prospective study might be required, because of the rarity of situs inversus this might not be possible.
Authorship Criteria:
Venu bhargav Malpuri – Concept and design, drafting, critical review, guarantor
Krishna Ramavath - Concept and design, drafting, critical review
Pranay singh Palle - Concept and design, drafting, critical review
Kishore Abuji - Concept and design, drafting, critical review
Conflicts of Interest: No conflict of interest among the authors
Grant Information: No funding provided
Acknowledgements: no acknowledgement
References
- Alam A, Santra A. Laparoscopic cholecystectomy in a case of situs inversus totalis: a review of technical challenges and adaptations. Ann Hepatobiliary Pancreat Surg, 2017; 21(2): 84-87. doi:10.14701/ahbps.2017.21.2.84.
- Kumar, Satendra & Roy, Arindam & Khanna, et al. Three port laparoscopic cholecystectomy in situs inversus totalis A case report. International Archives of Integrated Medicine, 2: 193-196.
- Alsabek MB, Arafat S, Aldirani A. A case report of laparoscopic cholecystectomy in situs inversus totalis: Technique and anatomical variation. Int J Surg Case Rep, 2016; 28: 124-126. doi: 10.1016/j.ijscr.2016.09.004. Epub 2016 Sep 22. PMID: 27701001; PMCID: PMC5048624.
- Fanshawe AEE, Qurashi K. Laparoscopic cholecystectomy for gallstone pancreatitis in a patient with situs inversus totalis. J Surg Case Rep, 2017; 2017(2): rjx003. Published 2017 Feb 8. doi:10.1093/jscr/rjx003
- Pavlidis TE, Psarras K, Triantafyllou A, Marakis GN, Sakantamis AK. Laparoscopic cholecystectomy for severe acute cholecystitis in a patient with situs inversus totalis and posterior cystic artery. Diagn Ther Endosc, 2008; 2008: 465272. doi: 10.1155/2008/465272. PMID: 18493329; PMCID: PMC2375966.
- Hu L, Chai Y, Yang X, et al. Duodenoscope combined with laparoscopy in treatment of biliary stones for a patient with situs inversus totalis: A case report. Medicine, 2019; 98(7): e14272. DOI: 10.1097/md.0000000000014272. PMID: 30762727; PMCID: PMC640807
- Aydin U, Unalp O, Yazici P, Gurcu B, Sozbilen M, Coker A. Laparoscopic cholecystectomy in a patient with situs inversus totalis. World J Gastroenterol. 2006; 12(47): 7717-7719. doi: 10.3748/ wjg.v12.i47.7717. PMID: 17171807; PMCID: PMC4088060.
- Rafie BA, Abuhamdan OJ. Laparoscopic Cholecystectomy in Patients with Situs Inversus Totalis. CRSLS MIS Case Reports e2014.00018: 1–4.
- Borgaonkar VD, Deshpande SS, Kulkarni VV, Laparoscopic cholecystectomyand appendicectomy in situs inversus totalis: a case report and review ofliterature, J. Minim. Access Surg, 2011; 7(4): 242–245.
- Dahuja G, Chandra S, Mahajan A, Kaur R. Laparoscopic Cholecystectomy in Situs Inversus Totalis patient – A rare case report. SAS J. Surg., 2015; 1(3): 66-68.
- Kafadar MT, Yalcin M, Daduk Y, Soyalp M, Gok MA. Laparoscopic Cholecystectomy for Acute Cholecystitis in Situs Inversus Totalis : An Extraordinary Approach. Eurasian J Emerg Med, 2018; 17: 82-84.
- Das ES, K.Bhattacharjee,S.Bandopadhyay et al Laparoscopic cholecystectomy in patients with situs inversus Editor D. Indian J Surg, 2005; 67(4): 4–5.
- Demetriades H, Botsios D, Dervenis C, Evagelou J, Agelopoulos S, Dadoukis J. Laparoscopic cholecystectomy in two patients with symptomatic cholelithiasis and situs inversus totalis. Dig Surg, 1999; 16(6): 519-521. doi: 10.1159/000018780. PMID: 10805554.
- Malik FS, Butt UI, Khan WH, Bilal SM, Umar M, Umer S. Laparoscopic Cholecystectomy in Situs Inversus Totalis. J Coll Physicians Surg Pak, 2019; 29(10): 1000-1002. doi: 10.29271/ jcpsp.2019.10.1000. PMID: 31564278
- Gulzar AB, Deepak G. Laparoscopic Cholecystectomy in Situs Inversus Totalis Patient: Our Experience. Adv Case Stud. 1(2). AICS.000506. 2018. DOI: 10.31031/AICS.2018.01.000506
- Jhobta RS, Gupta A, Negi B, Negi K. Single-incision laparoscopic cholecystectomy using conventional instruments in situs inversus totalis. BMJ Case Rep, 2018; 11(1): e226404. Published 2018 Nov 28. doi:10.1136/bcr-2018-226404.
- Egemen Çiçek, Fatih Sümer, Kutay Sağlam, Cüneyt Kayaalp. Secure laparoscopic cholecystectomy with surgical technique modification in abdominal situs inversus.Laparosc Endosc Surg Sci, 2018; 25(2): 81–82.
- Nursal TZ, Baykal A, Iret D, Aran O. Laparoscopic cholecystectomy in a patient with situs inversus totalis. J Laparoendosc Adv Surg Tech A, 2001; 11(4): 239-241. doi: 10.1089/109264201750539772. PMID: 11569515.
- Shirin L, Yasmin R. Experience of Surgery In Situs Inversus Totalis Patient - 3 Case Report. Gastroenterol Hepatol Open Access, 2016; 5(1): 00125. DOI: 10.15406/ghoa.2016.05.00125.
- Abdelkader I, Hussein M, Houseni M. Laparoscopic cholecystectomy in situs inversus totalis : Feasibility and review of literature. Int J Surg Case Rep [Internet], 2013; 4(8): 711–715.
- Jang JY, Lee W, Cho J, Jeong C, Hong S, et al. Laparoscopic Cholecystectomy in Two Patients with Situs Inversus Totalis : A Case Report. Journal of Minimally Invasive Surgery 2018; 21(2): 82-85.
- Bogarapu CB, Kishore R, Savalam B, Chinthagada J, Kattupalli SC. Laparoscopic cholecystectomy in a patient with situs inversus totalis : a case report. Int J Res Med Sci, 2015; 3(3): 805-807.
- Kim WY, Lee YN. Laparoscopic cholecystectomy in a situs inversus totalis patient with acute calculous cholecystitis : a case report. Int Hepato-Pancreato-Biliary Assoc [Internet], 2018; 20: S758.
- Ghosh N, Roy A, Bhattacharya S, Mukherjee S, Saha M. Laparoscopic Cholecystectomy in Situs Inversus , a Modified Approach. Indian J surg, 2008; 19(2): 2–4.
- Alkhlaiwy O, Almuhsin AM, Zakarneh E. International Journal of Surgery Case Reports Laparoscopic cholecystectomy in situs inversus totalis : Case report with review of techniques. Int J Surg Case Rep [Internet], 2019; 59: 208–212.
- Ren JJ, Li SD, Geng YJ, Xiao R. Modified laparoscopic cholecystectomy technique for treatment of situs inversus totalis: A case report. J Int Med Res, 2017; 45(3): 1261-1267. doi: 10.1177/0300060517703258. Epub 2017 Apr 18. PMID: 28417652; PMCID: PMC5536415
- Phothong N, Akaraviputh T, Chinswangwatanakul V, et al. Simplified technique of laparoscopic cholecystectomy in a patient with situs inversus: a case report and review of techniques. BMC Surg, 2015; 15: 23.
- Gelevski R, Jota G, Todorović L, Trajkovski G, Joksimović V, Trenčić B. Laparoscopic cholecystectomy in situs inversus totalis: Acta facultatis medicae Naissensis, 2021; 38(2): 183-188.
- Patle NM, Tantia O, Sasmal PK, Khanna S, Sen B. Laparoscopic cholecystectomy in situs inversus-our experience of 6 cases. Indian J Surg, 2010; 72(5): 391-394. doi: 10.1007/s12262- 010-0159-4. Epub 2010 Nov 18. PMID: 21966139; PMCID: PMC3077135.
- Gupta R, Singh H, Verma GR. Laparoscopic Cholecystectomy in Kartagener Syndrome. J Postgrad Med Edu Res, 2017; 51(4): 192-194.
- Hall TC, Barandiaran J, Perry EP. Laparoscopic cholecystectomy in situs inversus totalis: is it safe? Ann R Coll Surg Engl, 2010; 92(5): W30-W32. doi:10.1308/147870810X12699662980277.
- Roy A, Mukhopadhyay M. Situs Inversus Totalis: Operating on the Mirror Image. Hellenic J Surg, 2020; 92: 150–152.
- Kumar S, Fusai G. Laparoscopic cholecystectomy in situs inversus totalis with left-sided gall bladder. Ann R Coll Surg Engl, 2007; 89(2): W16-W18. doi:10.1308/147870807X160461.
- Tirelli F, Grieco M, Biondi A, Belia F, Persiani R. Laparoscopic cholecystectomy with indocyanine green fluorescence in a patient with situs inversus totalis. Mini-invasive Surg, 2021; 5: 15.
- Chaouch MA, Jerraya H, Dougaz MW, Dziri C. A Systematic Review of Laparoscopic Cholecystectomy in Situs Inversus. J Investig Surg [Internet], 2019; 0(0): 1–10.

