Psychological Stress and Type 2 Diabetes: A Review of the Bidirectional Link in the Onset and Progression of the Disease
Rojina Rashidi Ahmadi, Zahra Majdi, Mahdokht Yazdani Shokouh, Niloufar Masihipour and Seyed Ali Hosseini Zavareh*
Young Researchers and Elite Club, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
Medical Student, Department of Medicine, Islamic Azad University Tehran Medical Sciences, Iran
Medical doctor, Department of medicine, Lorestan University of medical science, Iran
Received Date: 14/05/2022; Published Date: 26/05/2022
*Corresponding author: Seyed Ali Hosseini Zavareh, Medical Student, Department of Medicine, Islamic Azad University Tehran Medical Sciences, Iran. Email: a.hosseini@student.iautmu.ac.ir
Abstract
In this article, the relationship between stress and type 2 diabetes has been carefully studied by considering various parameters such as individual-social factors, status of side diseases, diet and sleep status, cortisol changes, etc. Stress affects T2DM both directly and indirectly. Diabetics experience more stress and depression than healthy people, and ultimately stress and related processes contribute to the development of T2DM. Meanwhile, people who are more likely to be diagnosed with diabetes are more likely to be depressed. People with a family history of chronic illness are also more likely to have anxiety and stress.
Items such as inability to handle tasks and discomfort are associated with depression, and stress symptoms such as headache, shoulder stiffness, diarrhea, and constipation are significantly associated with diabetes. Many studies show that the level of stress and depression is directly related to diabetic distress and its most important factor is fear of the future and complications of the disease.
In the study of SES (socioeconemic status) factors, an inverse relationship with the risk of diabetes was assessed so that the lower the income level of people or the less educated, the poorer performance in coping with stress (emotional dealing with problems) and poor control over they will have blood sugar.
Since type 2 diabetes is the second most common physical disability after hypertension (8% of chronic patients) and also has a 3-fold mortality rate compared to other chronic patients; It is important to pay attention to common complications such as hypertension and heart disease. Stress can be involved in the development and spread of disease complications by affecting BP and MBF (myocardial blood flow).
PTSD causes hormonal and metabolic abnormalities that also lead to insulin resistance, and may also lead to sleep disturbances with increased levels of insulin resistance and blood C-protein concentrations, which is an important risk factor for T2DM. T2DM patients have higher stress, lower sleep quality and poorer mental health than healthy individuals. Sleep disorders are also associated with gender as a risk factor and are more common in women than men. People taking diabetes medications are more likely to have sleep disorders. In the field of nutrition, perceived stress and diabetes-related distress also have a significant effect on eating behavior (emotional and extreme coping). Family support and self-efficacy also have a positive and effective relationship in nutritional behaviors.
Regarding coping with stress and its consequences, several programs and solutions such as mindfulness-based stress reduction (MBSR) method have been proposed. The results obtained from the effectiveness of this method indicate that HbA1c level, blood sugar, depression level and stress they are significantly reduced.
Cortisol (a factor in raising blood sugar) is a glucocorticoid hormone that is released under stress and has been the focus of much study. In most studies, people with diabetes had higher cortisol levels than those in the control group, which was more strongly associated with depression with diabetes. Also, in diabetics, the activity level of the cortisone-to-cortisol-converting enzyme called 11BHSD1 is higher, and metformin has an intensifying effect on this enzyme.
Keywords: Psychological stress; Diabetes type 2; Socio-individual factors; Heart disease; Diet and sleep; Stress control methods; Cortisol
Introduction
Diabetes is a chronic metabolic disease characterized by elevated blood glucose levels and over time can lead to damage to the heart, blood vessels, eyes, kidneys and nerves. Managing diabetes is a lifelong process that can put a lot of stress on your daily life. Stress can be one of the main obstacles to effective glucose control. Stress affects T2DM both directly and indirectly by affecting other risk factors for diabetes [1,2].
Perceived stress is higher in diabetic people than in non-diabetics, and handgrip strength is higher in diabetic men than in diabetic women. This high stress in diabetics is related to low physical activity. Diabetics experience more stress, hostile symptoms, and depression than healthy people, and as a result, process disturbances may be related to biological stress. Stress and related processes contribute to the development of T2DM, and long-term diabetes can cause cognitive impairment, which occurs faster in men than in women due to structural differences in the brain and its function and differences between the sexes [3].
In an observational cohort study in men without a history of diabetes, a 2% incidence of diabetes was observed during 1.9 years of stress severity. Inability to handle work and discomfort were associated with depression and stress symptoms such as headache, shoulder stiffness, diarrhea and constipation were significantly associated with diabetes [4].
By examining the relationship between psychological stress and T2DM, it was found that the relationship between stress and diabetes can be directly related to the neuroendocrine system and cortisol and indirectly due to decreased exercise mood, diet modification and healthy lifestyle [6]. Exposure to higher psychological stress is associated with higher BMI and the person with more psychological stress is less active [7]. Also, people who are more likely to be diagnosed with diabetes are more likely to be depressed. People with a family history of chronic illness are also more likely to have anxiety and stress [8]. Another study aimed at examining the association between carboxylated osteocalcin (cOCN) and decarboxylated osteocalcin (dcOCN) levels with perceived chronic stress found a link between serum osteocalcin levels and stress in T2DM patients and depression. T2DM is more important and stronger than non-depressed individuals, but because no significant difference between Cocn and dcOCN was observed in depressed and non-depressed individuals, it was found that osteocalcin was not a good marker for determining depression in T2DM individuals [9]. Covid-19 patients with T1DM and T2DM reported increased stress, which was associated with HbA1C, and those with more severe glycemic control had more stress and more insulin quarantine than before [10]. Oral insulin and oral antihyperglycemic agents had higher mean depression and anxiety than those taking only one of the two drugs. HbA1C was significantly more directly related to anxiety, depression, and stress.
There was no link between self-management and depression, stress and anxiety, it may be concluded that the relationship between stress and diabetes is beyond behavioral impact [11].
Based on the above explanations, general cases regarding the relationship between stress and type 2 diabetes were stated, and in the following, we will examine the more detailed and accurate factors of this relationship and related factors.
Effect and relationship between individual and social factors
Psychological stress is one of the main factors that increase the risk of developing type 2 diabetes and the continuation of poor blood sugar control. In this study, an attempt was made to examine the effect of stress and its relationship with individual characteristics such as gender and age and social characteristics such as working conditions and family relationships. The relationship between the variables and the results should be examined more carefully.
Many studies show that the level of stress and depression is directly related to diabetic distress and its most important factor is fear of the future and complications of the disease. By gaining knowledge and learning disease management methods, stress can be overcome, so that in this study, only 2 people believed that their stress is due to type 2 diabetes. It is noteworthy that there is no relationship between stress and health-seeking behaviors in diabetic patients. What influences these behaviors are social demographic factors such as age, marital status, occupation and education, which we will examine in the following [12,13].
In the study of gender, it has been mentioned in articles that this factor is ineffective in effective parameters in diabetes such as HbA1c, BMI and physical activity as well as the accumulation of stressful events [14,15]. However, other studies in this field show that women experience higher diabetic distress and stress and act more emotionally and have lower self-esteem when dealing with more problems, but men have more depression and anxiety than women. Are tolerated [16-18]. The association between high blood pressure and type 2 diabetes is also associated with a relatively low increased risk of bisexuality in women compared to men [19,20].
Age is another interventional factor and is inversely related to the percentage of stress and depression; There is no risk of developing type 2 diabetes after the age of 65 [19,18].
Another influential factor is SES (socioeconemic status), which is inversely related to the risk of diabetes [20]; So that the lower the income level of people or the less unemployed and educated people are, the poorer their performance in dealing with stress (emotional dealing with problems), the higher the percentage of stress and depression and the more unfavorable control over blood sugar [17,18,21].
There was also a slight disagreement about the issue of work stress, with the study [19] that high work pressure before the age of 40 increased the risk, but according to the study [22], high work pressure and working hours only for low socio-economic groups. Raises the risk of infection.
Patients' family functioning and their social and emotional support can play a special role in the management and control of the disease [7 m]. But there are differences of opinion. Studies show that these factors are directly related to reducing stress and psychological satisfaction and thus better blood sugar control and risk reduction [25,24,21]. Family support is also significantly associated with medication in the elderly and their diet and can reduce patient stress [26]. However, other articles did not find a relationship between marital status and stress and the level of diabetic factors such as HbA1c and BMI [14,27].
It should also be noted that the duration of diabetes can affect more patients' stress, and the longer the illness lasts, the more likely people are to react emotionally to stressors [17].
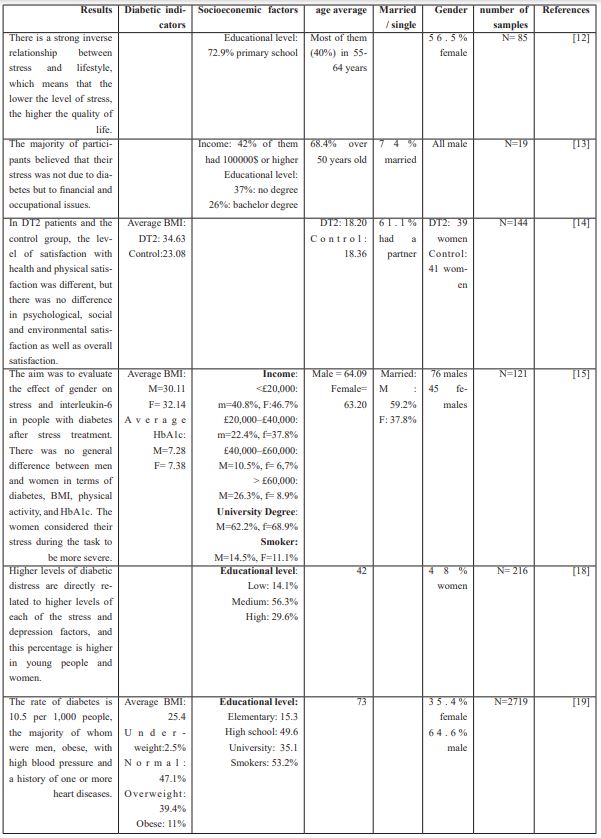
Table 1: Investigation of individual-social factors in studies.
Evaluation of heart diseases and other dangerous factors
Type 2 diabetes is the second most common physical disability after hypertension (8% of chronic patients) and also has a 3-fold mortality rate compared to other chronic patients [30]. Regarding the relationship between these two chronic diseases (type 2 diabetes and heart disease), the role of lifestyle of each person has a two-way relationship, and in between, the importance of diet has been much discussed, which we will examine in more detail, but as a mention. The key point is that the consumption of saturated fatty acids has a negative effect in both cases [31,32].
The disease may be associated with other complications and comorbidities such as hypertension, CVD, nephropathy, retinopathy, albuminuria, and even lesions such as diabetic foot thickness (affecting quality of life) [33]. One of the most common complications associated with type 2 diabetes is hypertension and ischemic heart disease. In a study [34] of 629 diabetics, 62 had a history of cardiovascular disease and insulin resistance had significantly improved [35]; So that many patients take antihypertensive drugs and ACE & ARB [29,30].
Studies show that high blood pressure alone increases the risk of type 2 diabetes [36] and the level SBP (Systolic Blood Pressure) and DBP (diastolic blood pressure) are higher in people who have recently had diabetes (NDDM) [37].
Stress can be involved in the development and spread of disease complications by affecting BP and MBF (myocardial blood flow); For example, MBF during stress in people with type 2 diabetes who had microalbuminuria or macroalbuminuria was significantly lower than in people with normoalbuminuria (P <0.01), which was significantly lower in those in macroalbuminuria than in those with microalbuminuria. (P = 0.04) In addition, the presence of autonomic neuropathy was associated with lower MBF during stress (P <0.01) and patients with severe retinopathy were significantly more MBF than patients with simple retinopathy or patients with no symptoms of retinopathy. They had lower stress times [38,39].
Therefore, it can be acknowledged that decreasing MBF during stress can be due to coronary artery disease such as diabetes mellitus, - in general, people with less optimism, due to increased daily cortisol concentration and also BP respond to stress, are more likely to develop CVD and CVD. In optimistic diabetics, DBP and SBP levels are higher, which is seen in healthy individuals [40]. There is also a negative association between HRV and negative emotions [41]. In a more comprehensive study, we can consider the role of race in the relationship between the above; According to the study [42], whites and African-Americans had different experiences of stressful events such as racial discrimination and its consequences, and statistics related to quality of life also show a better situation for whites.
The relationship between PTSD and diabetes and its control
PTSD causes hormonal and metabolic abnormalities that also lead to insulin resistance and increase the risk of diabetes [43].
In a study aimed at investigating the relationship between depression and stress after a natural disaster (such as a tsunami or earthquake) with blood sugar levels, it was found that there is a significant relationship between blood sugar and depression as well as blood sugar and stress [44].
PTSD alone is a risk factor for diabetes. One study found that obesity promoted the onset of PTSD symptoms. In fact, if obesity is caused by PTSD, following the treatment of symptoms, the process of weight gain slows down and even leads to weight loss, which in turn reduces the risk of metabolic and heart diseases. Antipsychotic and antidepressant drugs cause weight gain and impaired blood glucose regulation, which increases the risk of developing diabetes [45].
PTSD is associated with an increase in inflammatory markers and molecules involved in the inflammatory process. It may also increase insulin resistance and blood C-protein concentrations and cause sleep disturbances, which is associated with a higher risk of T2D. PTSD is also associated with HPA axis rotation, which impairs visceral obesity, insulin resistance, and T2D. In a 22-year longitudinal study of women, women with the most symptoms of PTSD were slightly more likely to have a larger somatotype at age 5, white, and a mother with T2D. Women with PTSD symptoms had a higher incidence of T2D than women without exposure to traumatic events. The use of antidepressants and BMI increases are also known to be the main possible mechanisms for increasing the risk of T2D in women with PTSD symptoms [46].
In another study of 184 people with T2D, by filling out questionnaires about depressive symptoms, PTSD symptoms, Diabetes distress, and self-care behaviors, the results showed that more severe depressive symptoms were directly related to higher HbA1C and higher diabetes distress, less physical activity, and inclination. Less to follow the recommended diet. On the other hand, PTSD score was significantly associated with diabetes distress and people with higher PTSD score were physically more physically active and checked their blood sugar status better and more than others [47].
Another study of 1,598 soldiers with PTSD who underwent treatment found that the incidence of T2D was higher in older people, blacks, people with lower primary care utilization, and shorter PTSD psychotherapy, hyperlipidemia, and hypertension. Obesity was significantly higher and the incidence of diabetes was significantly lower in soldiers who had more progress during treatment and whose TSPTSD was further reduced than in those who did not. [48]
Finally, a study of the symptoms of PTSD in a statistical population of 184 people with T2D who did not have good control over their disease, found that the weaker the control of the disease, the more severe the people experience the symptoms. These symptoms include arousal, withdrawal from society, and aggressive behaviors. On the other hand, these people are more inclined to exercise and pay attention to their intermittent blood sugar control. PTSD is associated with diabetic stress and has little to do with diet and HbA1C (unlike depression, which is associated) [49].
Stress control methods:
A deeper understanding of the relationship between stress and type 2 diabetes helps to apply these findings to improve diabetes and better understanding the disease. Many studies have been done to find out the nature of this relationship. Studies on the relationship between self-care behaviors of diabetics and stress showed that these self-care behaviors such as diet control, timely use of medications, and exercise were not related to stress. This may indicate that the relationship between stress and diabetes goes beyond the effect of stress on self-care behaviors and has a more direct effect on diabetes [50,51].
In another study focusing more on the direct effects of stress and diabetes, Seyitoglu et al. Examined the relationship between stress management and individual characteristics in diabetics. Types of stress management can be divided into two types: emotional and problem solving. In this study, it was found that among people with type 2 diabetes, emotional stress control, which is associated with older age, female gender, lower level of education and lower income, is also associated with longer duration of diabetes. Problem-solving stress control, which is more common in men, was less associated with HbA1c. As a result, people with problem-solving stress control were more likely to have severe diabetes than those with emotional stress control [52].
As mentioned, using this link between stress and diabetes in the clinic and in improving the condition of diabetic patients is very important. In this regard, studies have been conducted on various methods of stress management and their impact on the condition of diabetics. One of the most important ways to reduce stress is mindfulness-based stress reduction (MBSR) exercises, which include yoga, meditation, breathing exercises, exercise and sleep hygiene exercises. Studies of people with type 2 diabetes have shown that after several months of mindfulness and exercise, the test group's HbA1c and blood sugar levels, as well as their levels of depression, stress, anxiety, and emotion, are regulated. Significantly reduced; While in the control group there was no significant difference in these indicators. Together, these changes ultimately increase the quality of life and control of people with type 2 diabetes. As a result, this method can be used as a non-invasive and appropriate method to improve the condition of these patients [53-55]. In another study, which also used the Mindfulness method during 9 weekly sessions, a significant reduction in HbA1c, depression and relocation stress was seen in the intervention group compared to the control group [56].
Research has also been done on other methods of stress management and their effect on people with diabetes. One of these methods is Training Stress Management programs. These programs reduced stress, depression, anxiety, and diabetic distress in people with type 2 diabetes, as well as significantly reduced HbA1c [57,58]. In addition to reducing stress, another method called Riciation and relaxation treatment reduced the severity of cortisol and increased positive thinking and relaxation [59]. Pythagorean Self-Awareness Intervention, a type of meditation with daily mental and physical exercises to reduce stress, in addition to lowering HbA1C, decreased hair cortisol (long-term stress marker) and increased anti-aging markers such as leukocyte telomere length (LTL) and proteasome. [60]. Group Cognitive behavioral therapy (GCBT) also generally reduced anxiety and depression in people with diabetes mellitus and decreased HbA1c in the long term [61].
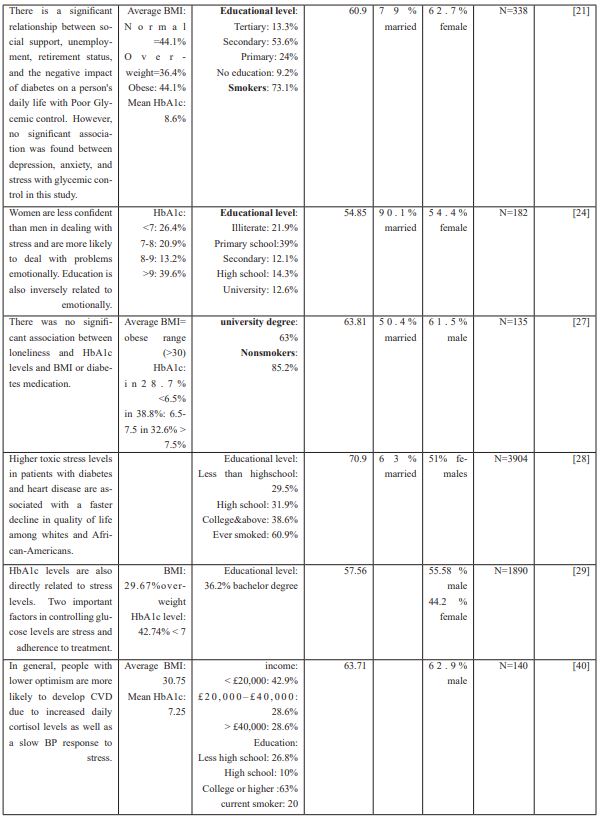
Table 2: At the end of this discussion, we tried to examine and compare studies in this field in more detail in Table 2.

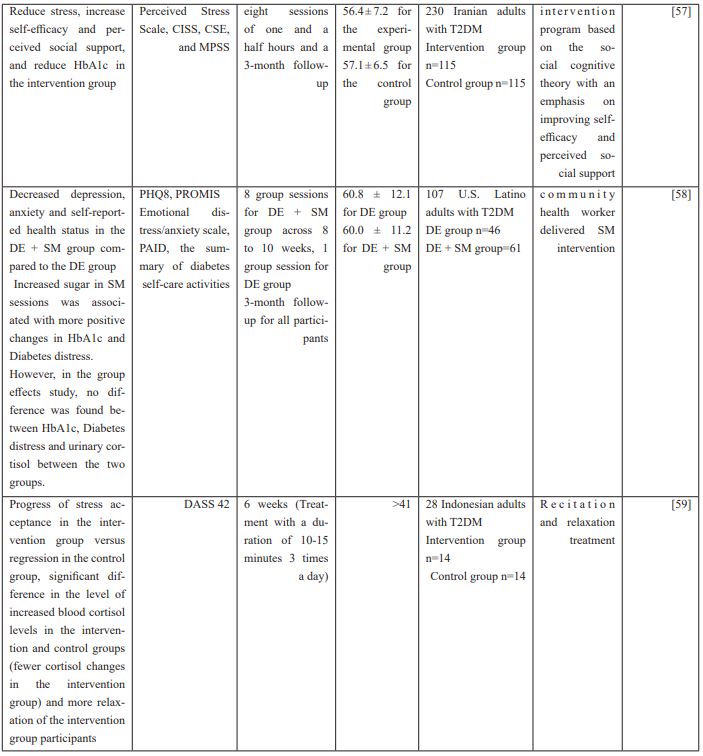
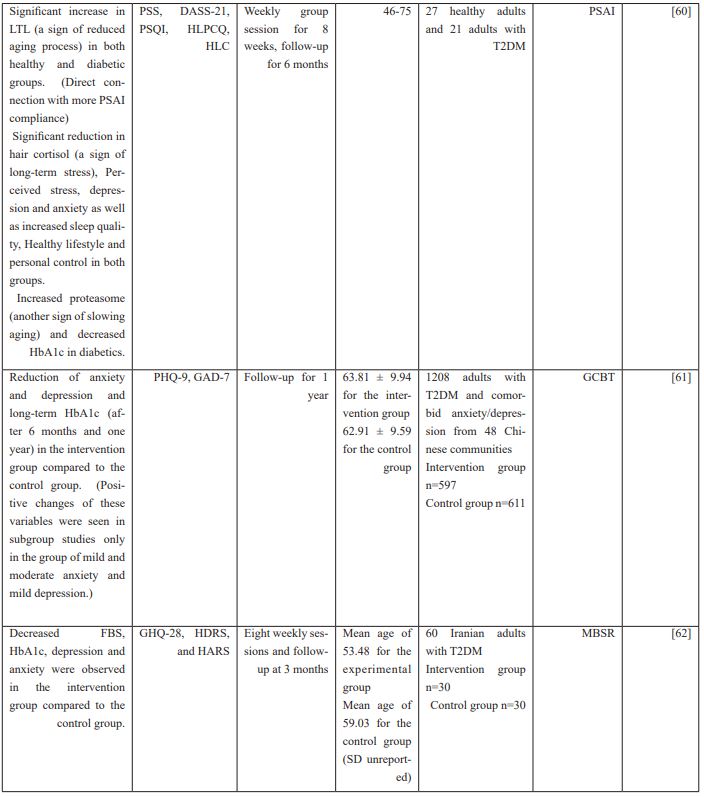
Table 2. MBSR = Mindfulness-Based Stress Reduction, T2DM = Type 2 Diabetes Mellitus, GHQ = General Health Questionnaire , HDRS = Hamilton Depression Rating Scale , HARS = Hamilton Anxiety Rating Scale , FBS = Fasting Blood Sugar, HbA1c = Hemoglobin A1C, CERQ = Cognitive Emotion Regulation Questionnaire, DASS = Depression, Anxiety and Stress Scale, CISS = Endler and Parker’s Coping Inventory for Stressful Situations, CSE = The Coping Self-Efficacy, MPSS = The Multidimensional scale of Perceived Social Support, DE = Diabetes Education, SM = Stress Management, PHQ = Personal Health Questionnaire, PAID = Problem Areas in Diabetes, GCBT = group cognitive behavioural therapy, GAD = General Anxiety Disorder questionnaire, PSAI = Pythagorean Self-Awareness Intervention, PSS = Perceived Stress Scale, PSQI = Pittsburgh Sleep Quality Index, HLPCQ = Healthy Lifestyle and Personal Control Questionnaire, HLC = Health Locus of Control Scale, LTL = Leucocyte Telomere Length
The effect of diet and sleep control
T2DM patients have higher stress, lower sleep quality and poorer mental health than healthy individuals, and stress and sleep disorders lead to poor glycemic control and biochemical changes in various organs, which ultimately leads to chronic complications [63].
Perceived stress and diabetes-related distress have a significant effect on eating behavior (restrained, emotional, external). Emotional coping mediates the effect of stress on eating behavior, so that diabetes-related stress has an indirect effect on restrained, emotional, and external eating behavior through emotional coping, and T2DM individuals respond to diabetes-related stress as a result of emotional coping. Overeating or undereating occur, but for general stress with an emotional response, only overeating behavior occurs. It was also found that in reastrained eating behavior, a person eats less by adopting a wrong reaction because he is emotion oriented in response to an unhealthy stress response. However, when T2DM individuals perform conscious dietary interventions, their cognitive control and control of eating behavior are improved and their overeating and uncontrollability are significantly reduced, which should include personal, family, and social aspects of T2DM individuals [64,65].
In a study of 117 people with diabetes, it was found that family support and self-efficacy had a positive relationship and stress had a negative relationship with dietary behaviors in diabetics. The strongest relationships between family support and self-efficacy with managing diet challenges and choosing a healthy and the strongest association of stress with the inability to determine the number of calories needed and then, the inability to manage dietary challenges, the inability to choose a healthy diet to the extent and ultimately reduce the ability to prepare meals [66].
Education's level of education affects food choice; The higher the level of education, the wider the selection of foods that are more nutritious, which affects a person's health. Diet plays an important role in people with diabetes who cannot manage their diet according to 3J settings. The 3J diet pattern includes program, type, and amount, and this can cause a diabetic to experience high blood sugar [67].
A study of 126,279 middle-aged Korean people found that with increased stress, consumption of carbohydrates and grains was higher, but consumption of all other nutrients, fruits, vegetables, and protein foods was lower. Higher stress was significantly associated with lower DVS (dietary variety score) and the combination of high stress and low DVS was significantly associated with an increased risk of type II diabetes [68].
There is an inverse relationship between fiber intake and FBGL (Fast Blood Glucose Level), magnesium intake and FBGL. Zinc intake is negatively correlated with FBGL and physical activity and FBGL is negatively correlated. Also, the mean FBGL in T2DMs with lower stress was better than patients with moderate stress levels [69].
As a result, unhealthy eating behavior is associated with higher BMI as well as higher levels of cortisol and cortisone [70].
In young people with T2D, variable risk factors such as stress, decreased physical activity and insufficient sleep were observed. Immigrants are also at higher risk for T2D [71].
There is also evidence of decreased sleep quality in diabetics due to the negative effect of blood glucose on sleep [72].
By examining the effect of sleep regulation and stress on T2D in 35 Emirati patients, it was observed that the patients in the experimental group significantly lost weight, BMI, improvement in HbA1C and improvement in recovery level after 24 weeks compared to control patients. And duration of stress decreased in the experimental group but increased in the control group; Cholesterol, triglyceride, HDL and LDL reductions were also higher in the experimental group, but these differences were not statistically significant [73].
Sleep disorders are gender-related and are more common in women than men. People taking diabetes medications are more likely to have sleep disorders, and people with widespread sleep disorders have higher levels of cortisol on a normal day (over the course) as well as cortisol in the evening; But it has no significant relationship with morning cortisol and 45min post-task cortisol. Therefore, in people with sleep disorders, the level of cortisol concentration that results from stress is low. Sleep disturbance increases the risk of cardiovascular disease by having a detrimental effect on the neuroendocrine system (in which cortisol plays a key role in the diabetic process) [74].
Evaluation of cortisol levels and changes in different conditions:
Cortisol is a glucocorticoid hormone that is released under stress. Cortisol secretion raises blood sugar. Due to the close relationship between cortisol and stress, especially blood sugar, changes in this hormone and the hypothalamus-pituitary-adrenal axis are considered in diabetes [75]. In other words, cortisol was considered as a bridge between depression and stress with insulin resistance and eventually diabetes, although according to studies, other factors such as increased glucagon hormone in the development of hepatic insulin resistance, especially in non-diabetics are known [76,77]; In the following, focusing on the studies conducted, we will deal with the communications raised in this field.
The association between high cortisol levels and type 2 diabetes in patients with this disease has been investigated in several studies. In most of these studies, an effective relationship has been seen between the two. People with type 2 diabetes had higher cortisol levels than the control group [78]. This association has been stronger in the presence of depression along with diabetes [79]. This association was observed in both men and women, although there were slight differences depending on the sex. For example, cortisol levels in the LNSC (Late-Night Salivary Cortisol) test were higher in women with diabetes than in healthy people, but on the other hand. In diabetic men, cortisol levels were higher in the CAR (Cortisol Awakening Response) test than in healthy individuals [80]. However, in another study, despite a significant difference in wake-up cortisol during the 6-year study of the diabetic group and the control group, there was no difference in cortisol curve features between the two groups. This showed that the overall performance of the HPA axis was not different between the two groups [81].
Research has also been done on the ratio of cortisol to cortisone in diabetics. In a study, Liu et al. Found that the ratio of cortisol to cortisone was negatively associated with diabetes [82]. Also, in diabetics, the activity level of the cortisone-to-cortisol-converting enzyme called 11BHSD1 is higher, and metformin has an intensifying effect on this enzyme. Therefore, it is recommended to take metformin with 11BHSD1 inhibitor to prevent this complication and maximize the effectiveness of metformin [83]. However, in another study, despite the higher level of cortisol in diabetics compared to the control group, the level of cortisone and the ratio of cortisol to cortisone were not significantly different between the two groups. In fact, the results of this article contradicted the previous two articles and showed that high cortisol in diabetics is not related to changes in the levels of cortisone and cortisol-converting enzymes. This difference may be due to the small number of samples in this article [84].
Among diabetics, studies have been performed on the relationship between disease severity and cortisol levels. One of the markers that can be considered to assess the severity of diabetes is HbA1c, which indicates the average level of glucose in the last 2 to 3 months in a person. HbA1C also indicates the state of glucose metabolism in the body and can indicate the severity of metabolic disorders. Correlations have been observed between HbA1c levels and cortisol levels; Of course, the results are inconsistent. In the study mentioned above, in addition to the mentioned findings, a significant relationship was seen between the level of HbA1c and the level of LNCS in women and CAR in men [80]. It should be noted, however, that in another study examining the level of accuracy of the LNSC test compared to the DST test, which is an accepted test, the accuracy of this test was estimated to be 30% compared to the DST test, indicating that reliance on the LNSC test alone is sufficient. It is not and this test is not completely reliable. On the other hand, some studies that examined the association of diabetes markers such as BMI, HbA1C with cortisol levels did not find this relationship [85-87]. Another marker of interest is Impaired Fasting Glycemia (IFG), which indicates a prediabetic condition. In this regard, the relationship between IFG and pre-diabetic conditions with higher cortisol levels has been observed [86].
Impaired cortisol response is another case study that differentiates between diabetic and control individuals. impaired cortisol response is important because it causes more hospitalizations and worse patient conditions during hypoglycemia. The incidence of Impaired cortisol response in hypoglycemic conditions is also higher in diabetic individuals than in healthy individuals, which is directly related to age and Admission Rate and inversely related to male gender and duration of diabetes, growth hormone levels and ACTH levels. The opposite relationship with the duration of diabetes is due to lower blood glucose in people who have a shorter duration of the disease, which increases the number of hypoglycemias and more regulatory disorders. [88].
Complications of diabetes are also very significant cases in this disease that cause many problems for people with diabetes. One of these complications is microalbuminuria, which is the first sign of diabetic nephropathy. In a study aimed at finding a relationship between microalbuminuria and cortisol levels, it was found that cortisol levels were higher in diabetic individuals with albuminuria than in normoalbuminuric diabetics [85].
Studies have also been done on the relationship between stress, cortisol and diabetes. One of the factors that can cause stress in adulthood is Childhood neglect, which itself is divided into two categories: Emotional and physical neglect. In a study of the relationship between childhood neglect and plasma cortisol levels in response to stress in diabetics, the combination of type 2 diabetes and physical neglect was associated with increased stress levels and further changes in cortisol after stress induction. On the other hand, the combination of type 2 diabetes and Emotional neglect was significantly associated with an increase in basal ACTH levels as well as an increase in tension levels after stress induction.
In general, this study showed that there is a significant relationship between Childhood Neglect and the response of diabetics to stress and the level of cortisol changes and their basal ACTH level [89]. Other types of stress include overall distress and physician-related distress, which are directly related to morning cortisol in diabetics [90]. In another study, a study was conducted between Distress induced and cortisol levels in diabetic adolescent girls. In this study, they found that mindfulness, by increasing the concentration of the voluntary senses, caused the negative effects of stress to be less felt, but had no direct effect on cortisol levels [91].
Another link between exercise, cortisol and diabetes. The effect of exercise on the improvement of type 2 diabetes has been proven. In this regard, studies have focused specifically on the effect of exercise on cortisol levels in people with type 2 diabetes. In a study of obese women with type 2 diabetes, the effect of aerobic exercise on cortisol levels was investigated. In this study, women who did aerobic exercise for 6 weeks at the end of these 6 weeks had significantly lower final cortisol levels than the placebo group. Also, the group that did aerobic exercise and took Spirulina supplementation (a type of algae with it) had lower cortisol levels at the end of the study than the previous two groups. Finally, it can be concluded that the addition of exercise program and even the use of herbal supplements can be effective in controlling the disease and cortisol levels in diabetics [92].
References
- Harris ML, Oldmeadow C, Hure A, Luu J, Loxton D, Attia J. Stress increases the risk of type 2 diabetes onset in women: A 12-year longitudinal study using causal modelling. PloS one, 2017; 12(2): e0172126.
- Mishra DN. Stress Etiology of Type 2 Diabetes. Current Diabetes Reviews, 2022.
- Devaraju K, Shetty SC. Perceived stress, cognitive function test, and handgrip strength in type 2 diabetes mellitus. National Journal of Physiology, Pharmacy and Pharmacology, 2019; 9(7): 678-682.
- Takahashi K, Kamino T, Yasuda T, Suganuma A, Sakane N. Association Between Psychological Distress and Stress-Related Symptoms and Increased Risk of Type 2 Diabetes in Male Individuals: An Observational Study. Journal of Clinical Medicine Research, 2020; 12(12): 816.
- Khode V, Nagalakshmi V, Ruikar K, Dugani R. Detection of cognitive impairment in Type 2 diabetes mellitus by choice auditory and visual reaction times during acute mental stress: A case–control study. National Journal of Physiology, Pharmacy and Pharmacology, 2020; 10(10): 870-873.
- Putri A, Rustam JS. Psychological stress and long-term risk of type 2 diabetes mellitus among civil servant: a prospective cohort study. Malaysian Journal of Medical Research (MJMR), 2021; 5(1): 19-24.
- Lysy Z, Da Costa D, Dasgupta K. The association of physical activity and depression in Type 2 diabetes. Diabetic Medicine, 2008; 25(10): 1133-1141.
- Alzahrani A, Alghamdi A, Alqarni T, Alshareef R, Alzahrani A. Prevalence and predictors of depression, anxiety, and stress symptoms among patients with type II diabetes attending primary healthcare centers in the western region of Saudi Arabia: a cross-sectional study. International journal of mental health systems, 2019; 13(1): 1-7.
- Nguyen MM. Associations Between Serum Osteocalcin and Subjective Stress in People with Depression and Type II Diabetes (Doctoral dissertation, University of Toronto (Canada)).
- Ruissen MM, Regeer H, Landstra CP, Schroijen M, Jazet I, Nijhoff MF, et al. Increased stress, weight gain and less exercise in relation to glycemic control in people with type 1 and type 2 diabetes during the COVID-19 pandemic. BMJ Open Diabetes Research and Care, 2021; 9(1): e002035.
- Chlebowy DO, Batscha C, Kubiak N, Crawford T. Relationships of depression, anxiety, and stress with adherence to self-management behaviors and diabetes measures in African American adults with type 2 diabetes. Journal of racial and ethnic health disparities, 2019; 6(1): 71-76.
- Rizqillah AF, Ma’rifah AR, Ardilla B. Stress, Quality of Life, and Health Seeking Behavior Among Type 2 Diabetes Mellitus in Wangon, Banyumas, Indonesia. Age, 2020; 35(44): 11.
- Sherman LD, Comer-Hagans D, Pattin AJ. Experiences with Stress Among African American Men Living with Type 2 Diabetes: A Qualitative Inquiry. SAGE Open Nursing, 2019; 5: 2377960819871806.
- Kumar A, Kumari R, Singh LK, Kumar D. Socio-economic Status, Stress and Type 2 Diabetes: An Exploring Link. Our Heritage, 2020; 68(1): 10565-10574.
- Panagi L, Poole L, Hackett RA, Steptoe A. Sex differences in interleukin‐6 stress responses in people with Type 2 diabetes. Psychophysiology, 2019; 56(6): e13334.
- Gautam SK. Prevalence of Depression, Anxiety and Stress among Patients of Type-2 Diabetes Mellitus and Effect of Glycemic Control on Depression Anxiety and Stress in Tertiary Care Center. International Journal, 2020; 3(2): 226.
- Seyitoglu DC, Gunes G, Gokce A, Tekin Ç. Glycemic control and coping with stress in type 2 diabetes patients. International Journal of Community Medicine and Public Health, 2018; 5(2): 466.
- Bo A, Pouwer F, Juul L, Nicolaisen SK, Maindal HT. Prevalence and correlates of diabetes distress, perceived stress and depressive symptoms among adults with early‐onset type 2 diabetes: Cross‐sectional survey results from the Danish DD2 study. Diabetic Medicine, 2020; 37(10): 1679-1687.
- Pan KY, Xu W, Mangialasche F, Fratiglioni L, Wang HX. Work‐related psychosocial stress and the risk of type 2 diabetes in later life. Journal of internal medicine, 2017; 281(6): 601-610.
- Crump C, Sundquist J, Winkleby MA, Sundquist K. Stress resilience and subsequent risk of type 2 diabetes in 1.5 million young men. Diabetologia, 2016; 59(4): 728-733.
- Shuhaida MH, Suhaila MY, Azidah KA, Norhayati NM, Nani D, Juliawati M. Depression, anxiety, stress and socio-demographic factors for poor glycaemic control in patients with type II diabetes. Journal of Taibah University Medical Sciences. 2019 Jun 1;14(3):268-276.
- Hackett RA, Steptoe A. Type 2 diabetes mellitus and psychological stress—a modifiable risk factor. Nature Reviews Endocrinology, 2017; 13(9): 547-560.
- Jain N, Singla M, Chaudhary R. Correlation of Type 2 Diabetes Mellitus with Percieved Stress and Family Functioning. Canadian Journal of Diabetes, 2018; 42(5): S33.
- Kalka D, Karcz B. Personality, coping with stress and quality of life in individuals at risk of type 2 diabetes in late adolescence-mediation model testing. European Journal of Developmental Psychology, 2020; 17(2): 165-178.
- Singla M, Jain NP, Chaudhry R. Correlation of type 2 diabetes mellitus with perceived stress and family functioning. Diabetologie und Stoffwechsel, 2018; 13(S 01): P-57.
- Trisnadewi NW, Adiputra IM, Oktaviani NP, Suapriyanti PA, Saraswati NL. Correlation between stress level and family support towards fasting and postprandial glucose level in type 2 diabetes mellitus. Age (year), 2020; 25(1): 1-3.
- Hackett RA, Poole L, Hunt E, Panagi L, Steptoe A. Loneliness and biological responses to acute stress in people with Type 2 diabetes. Psychophysiology, 2019; 56(6): e13341.
- Nkwata AK, Song X, Zhang M, Ezeamama AE. Change in quality of life over eight years in a nationally representative sample of US adults with heart disease and type 2 diabetes: minority race and toxic stress as keysocial determinants. BMC public health, 2020; 20: 1-2.
- Meebunmak Y, Khamthana P, Intana J, Voraroon S, Siramaneerat I. The Relationship Between Stress and Type 2 Diabetes Mellitus Management In Ratchaburi Province, Thailand. Psychology and Education Journal, 2021; 58(4): 2112-2116.
- Setyorini A, Supriyadi S. Stress of Type 2 Diabetes Mellitus Patients in Implementation Self Care Management. STRADA Jurnal Ilmiah Kesehatan, 2020; 9(2): 1250-1257.
- Mann JI. Diet and risk of coronary heart disease and type 2 diabetes. The Lancet, 2002; 360(9335): 783-789.
- Schulze MB, Hu FB. Dietary patterns and risk of hypertension, type 2 diabetes mellitus, and coronary heart disease. Current atherosclerosis reports, 2002; 4(6): 462-467.
- Maryam Mahdavi Afshar, Mohaddeseh Parsay, Meisam Gholami, Alex Avakian, Seyed Ali Hosseini Zavareh, et al., A Review of Diabetic Wound Healing Methods Based on Using Stem Cells. Am J Biomed Sci & Res, 2021; 15(1). AJBSR.MS.ID.002066.
- Pah AM, Bucuras P, Buleu F, Tudor A, Iurciuc S, Velimirovici D, et al. The importance of DS-14 and HADS questionnaires in quantifying psychological stress in type 2 diabetes mellitus. Medicina, 2019; 55(9): 569.
- Gariani K, Marques-Vidal P, Waeber G, Vollenweider P, Jornayvaz FR. Salivary cortisol is not associated with incident insulin resistance or type 2 diabetes mellitus. Endocrine connections, 2019; 8(7): 870-877.
- AA A. Exercise, Stress, Cholesterol, and Hypertension as Risk Factors of Type 2 Diabetes Mellitus in South Sulawesi, Indonesia. Indian Journal of Public Health Research & Development, 2019; 10(8).
- Siddiqui A, Madhu SV, Sharma SB, Desai NG. Endocrine stress responses and risk of type 2 diabetes mellitus. Stress, 2015; 18(5): 498-506.
- Sørensen MH, Bojer AS, Pontoppidan JR, Broadbent DA, Plein S, Madsen PL, et al. Reduced myocardial perfusion reserve in type 2 diabetes is caused by increased perfusion at rest and decreased maximal perfusion during stress. Diabetes Care, 2020; 43(6): 1285-1292.
- Soerensen MH, Bojer AS, Madsen PL, Gaede P. P4469 Reduced myocardial perfusion reserve in type 2 diabetes is caused by increased rest perfusion as well as decreased maximal perfusion during stress. European Heart Journal, 2019; 40(Supplement_1): ehz745-0866.
- Puig‐Perez S, Hackett RA, Salvador A, Steptoe A. Optimism moderates psychophysiological responses to stress in older people with Type 2 diabetes. Psychophysiology, 2017; 54(4): 536-543.
- Wagner JA, Feinn R, Lampert R, Bermúdez-Millán A, Pérez-Escamilla R. Changes in negative affect and changes in heart rate variability among low-income Latinos with type 2 diabetes in a randomized, controlled stress management trial. Journal of psychosomatic research, 2019; 124: 109774.
- Nkwata AK, Song X, Zhang M, Ezeamama AE. Change in quality of life over eight years in a nationally representative sample of US adults with heart disease and type 2 diabetes: minority race and toxic stress as keysocial determinants. BMC public health, 2020; 20: 1-2.
- Vaccarino V, Goldberg J, Magruder KM, Forsberg CW, Friedman MJ, Litz BT, et al. Posttraumatic stress disorder and incidence of type-2 diabetes: a prospective twin study. Journal of psychiatric research, 2014; 56: 158-164.
- Evriany N, Fatimah GN, Chalidyanto D. Relationship between depression and stress with blood sugar levels in patients with diabetes melitus type II. EurAsian Journal of BioSciences, 2020; 14(2): 2709-2713.
- Scherrer JF, Lustman PJ. Posttraumatic Stress Disorder and Incident Type 2 Diabetes: Is Obesity to Blame? Chronic Stress, 2019; 3: 2470547019863415.
- Roberts AL, Agnew-Blais JC, Spiegelman D, Kubzansky LD, Mason SM, Galea S, et al. Posttraumatic stress disorder and incidence of type 2 diabetes mellitus in a sample of women: a 22-year longitudinal study. JAMA psychiatry. 2015; 72(3): 203-210.
- Arigo D, Juth V, Trief P, Wallston K, Ulbrecht J, Smyth JM. Unique relations between post-traumatic stress disorder symptoms and patient functioning in type 2 diabetes. Journal of health psychology, 2020; 25(5): 652-664.
- Scherrer JF, Salas J, Norman SB, Schnurr PP, Chard KM, Tuerk P, et al. Association between clinically meaningful posttraumatic stress disorder improvement and risk of type 2 diabetes. JAMA psychiatry, 2019; 76(11): 1159-1166.
- Arigo D, Juth V, Trief P, Wallston K, Ulbrecht J, Smyth JM. Unique relations between post-traumatic stress disorder symptoms and patient functioning in type 2 diabetes. Journal of health psychology, 2020; 25(5): 652-664.
- Bassi G, Gabrielli S, Donisi V, Carbone S, Forti S, Salcuni S. Assessment of Psychological Distress in Adults with Type 2 Diabetes Mellitus Through Technologies: Literature Review. Journal of medical Internet research, 2021; 23(1): e17740.
- Tohid H, Papo M, Ahmad S, Sumeh AS, Jamil TR, Hamzah Z. Self-care activities among patients with Type 2 Diabetes Mellitus in Penampang, Sabah and its association with depression, anxiety and stress. Malaysian Journal of Public Health Medicine, 2019; 19(1): 117-125.
- Seyitoglu DC, Gunes G, Gokce A, Tekin Ç. Glycemic control and coping with stress in type 2 diabetes patients. International Journal of Community Medicine and Public Health, 2018; 5(2): 466.
- Ravari ON, Mousavi SZ, Babak A. Evaluation of the effects of 12 weeks mindfulness-based stress reduction on glycemic control and mental health indices in women with diabetes mellitus type 2. Advanced Biomedical Research, 2020; 9.
- Tavakoli Z, Kazemi-Zahrani H. The Effectiveness of Mindfulness Based Stress Reduction Intervention on Emotion Regulation Problems and Blood Sugar Control in Patients with Diabetes Type II. Global Journal of Health Science, 2018; 10(3): 111.
- Armani Kian A, Vahdani B, Noorbala AA, Nejatisafa A, Arbabi M, Zenoozian S, et al. The impact of mindfulness-based stress reduction on emotional wellbeing and glycemic control of patients with type 2 diabetes mellitus. Journal of diabetes research, 2018; 2018.
- Chen SM, Lin HS, Atherton JJ, MacIsaac RJ, Wu CJ. Effect of a mindfulness programme for long‐term care residents with type 2 diabetes: A cluster randomised controlled trial measuring outcomes of glycaemic control, relocation stress and depression. International journal of older people nursing, 2020; 15(3): e12312.
- Zamani-Alavijeh F, Araban M, Koohestani HR, Karimy M. The effectiveness of stress management training on blood glucose control in patients with type 2 diabetes. Diabetology & metabolic syndrome, 2018; 10(1): 1-9.
- Wagner JA, Bermudez-Millan A, Damio G, Segura-Perez S, Chhabra J, Vergara C, Feinn R, Perez-Escamilla R. A randomized, controlled trial of a stress management intervention for Latinos with type 2 diabetes delivered by community health workers: outcomes for psychological wellbeing, glycemic control, and cortisol. Diabetes research and clinical practice, 2016; 120: 162-170.
- Amir F, Mastutik G, Hasinuddin M, Putra ST. Dhikr (recitation) and relaxation improve stress perception and reduce blood cortisol level in type 2 diabetes mellitus patients with OAD. Folia Medica Indonesiana, 2018; 54(4): 249-255.
- Athanasopoulou S, Simos D, Charalampopoulou M, Tentolouris N, Kokkinos A, Bacopoulou F, et al. Significant improvement of stress and aging biomarkers using a novel stress management program with the cognitive restructuring method" Pythagorean Self-Awareness Intervention" in patients with type 2 diabetes mellitus and healthy adults. Mechanisms of Ageing and Development, 2021; 198: 111538.
- Xu C, Dong Z, Zhang P, Chang G, Xiang Q, Zhang M, et al. Effect of group cognitive behavioural therapy on psychological stress and blood glucose in people with type 2 diabetes mellitus: A community‐based cluster randomized controlled trial in China. Diabetic Medicine, 2021; 38(2): e14491.
- Armani Kian A, Vahdani B, Noorbala AA, Nejatisafa A, Arbabi M, Zenoozian S, et al. The impact of mindfulness-based stress reduction on emotional wellbeing and glycemic control of patients with type 2 diabetes mellitus. Journal of diabetes research. 2018; 2018.
- Rahim A, Andylim NF, Mansor MA, Yaacob N. Stress and Poor Quality of Sleep: Risk Factors Contributing to Type 2 Diabetes Mellitus.
- Park M, Quinn L, Park C, Martyn-Nemeth P. Pathways of the relationships among eating behavior, stress, and coping in adults with type 2 diabetes: A cross-sectional study. Appetite, 2018; 131: 84-93.
- Park M, Quinn L, Park C, Martyn-Nemeth P. Pathways of the relationships among eating behavior, stress, and coping in adults with type 2 diabetes: A cross-sectional study. Appetite, 2018; 131: 84-93.
- Putra KW, Toonsiri C, Junprasert S. Self-efficacy, psychological stress, family support, and eating behavior on type 2 diabetes mellitus. Belitung Nursing Journal, 2016; 2(1): 3-7.
- Sari NA, Nurhayati C, Rustini SA. Relationship of Stress Levels and Diet with Blood Sugar Levels In Patients Of Type 2 Diabetes Mellitus. STRADA Jurnal Ilmiah Kesehatan, 2020; 9(1): 241-247.
- Shin Y, Kim Y. Psychological Stress Accompanied by a Low-Variety Diet Is Positively Associated with Type 2 Diabetes in Middle-Aged Adults. Nutrients, 2020; 12(9): 2612.
- Putri RT, Wahyuni Y, Jus' at I. Glycemic load, fiber, magnesium, zinc, physical activity, stress factor and fasting blood glucose level. Darussalam Nutrition Journal, 2021; 5(1): 1-3.
- Ganesan N, Priya J, Devi G. Estimation of cortisol in Type II diabetes mellitus among South Indian population. Drug Invention Today, 2019; 12(9).
- Dave S, Suntharamoorthy K, Mohyiddin SS, Muhammad U, Malik S, Gupta N. 2163-PUB: Prevalence of Multiple Stress Factors in Young Adults with Type 2 Diabetes.
- Khosravan S, Alami A, Golchin Rahni S. Prevalence of sleep disorder in type 2 diabetes Mellitus patients and it's related factors. Journal of Research and Health, 2015; 5(3): 298-304.
- Mussa BM, Schauman M, Kumar V, Skaria S, Abusnana S. Personalized intervention to improve stress and sleep patterns for glycemic control and weight management in obese Emirati patients with type 2 diabetes: a randomized controlled clinical trial. Diabetes, metabolic syndrome and obesity: targets and therapy, 2019; 12: 991.
- Hackett RA, Dal Z, Steptoe A. The relationship between sleep problems and cortisol in people with type 2 diabetes. Psychoneuroendocrinology, 2020; 117: 104688.
- Vallejo L, Zapater M, Montoliu T, Puig Pérez S, Nacher J, Hidalgo V, Salvador A. No effects of acute psychosocial stress on working memory in older people with type 2 diabetes. Frontiers in Psychology, 2020; 11: 3759.
- Basu A, Yadav Y, Carter RE, Basu R. Novel Insights into Effects of Cortisol and Glucagon on Nocturnal Glucose Production in Type 2 Diabetes. The Journal of Clinical Endocrinology & Metabolism, 2020; 105(7): e2378-88.
- Joseph JJ, Golden SH. Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 diabetes mellitus. Annals of the New York Academy of Sciences, 2017; 1391(1): 20-34.
- Prabu P, Poongothai S, Shanthirani CS, Anjana RM, Mohan V, Balasubramanyam M. Altered circulatory levels of miR-128, BDNF, cortisol and shortened telomeres in patients with type 2 diabetes and depression. Acta diabetologica, 2020; 57(7): 799-807.
- Sang YM, Wang LJ, Mao HX, Lou XY, Zhu YJ, Zhu YH. Correlation of lower 2 h C-peptide and elevated evening cortisol with high levels of depression in type 2 diabetes mellitus. BMC psychiatry, 2020; 20(1): 1-1.
- Johar H, Emeny RT, Bidlingmaier M, Kruse J, Ladwig KH. Sex-related differences in the association of salivary cortisol levels and type 2 diabetes. Findings from the cross-sectional population based KORA-age study. Psychoneuroendocrinology, 2016; 69: 133-141.
- Spanakis EK, Wang X, Sánchez BN, Roux AV, Needham BL, Wand GS, Seeman T, Golden SH. Lack of significant association between type 2 diabetes mellitus with longitudinal change in diurnal salivary cortisol: the multiethnic study of atherosclerosis. Endocrine, 2016; 53(1): 227-239.
- Liu X, Jiang J, Liu X, Luo Z, Wang Y, Dong X, et al. Gender-specific independent and combined effects of the cortisol-to-cortisone ratio and 11-deoxycortisol on prediabetes and type 2 diabetes mellitus: from the Henan rural cohort study. Journal of diabetes research, 2019; 2019.
- Anderson AJ, Andrew R, Homer NZ, Jones GC, Smith K, Livingstone DE, et al. Metformin increases cortisol regeneration by 11βHSD1 in obese men with and without type 2 diabetes mellitus. The Journal of Clinical Endocrinology & Metabolism, 2016; 101(10): 3787-3793.
- Balikcioglu PG, Balikcioglu M, Soros A, Chalew S. The 24-hour average concentration of cortisol is elevated in obese African-American youth with type 2 diabetes. Journal of Diabetes and its Complications, 2021; 35(7): 107933.
- Zhang X, Deng X, Zhou J, Qiu K, Deng M, Lin Z, et al. The Association of Serum Cortisol Level with Microalbuminuria in Patients With Type 2 Diabetes And Prediabetes. International journal of medical sciences, 2020; 17(18): 2998.
- Bellastella G, Maiorino MI, De Bellis A, Vietri MT, Mosca C, Scappaticcio L, Pasquali D, Esposito K, Giugliano D. Serum but not salivary cortisol levels are influenced by daily glycemic oscillations in type 2 diabetes. Endocrine, 2016; 53(1): 220-226.
- Steffensen C, Thomsen HH, Dekkers OM, Christiansen JS, Rungby J, Jørgensen JO. Low positive predictive value of midnight salivary cortisol measurement to detect hypercortisolism in type 2 diabetes. Clinical endocrinology, 2016; 85(2): 202-206.
- Rhyu YA, Jang JY, Park S, An JH, Kim DL, Kim SK, Song KH. Impaired cortisol and growth hormone counterregulatory responses among severe hypoglycemic patients with type 2 diabetes mellitus. Endocrinology and Metabolism, 2019; 34(2): 187-194.
- Monzer N, Hartmann M, Buckert M, Wolff K, Nawroth P, Kopf S, Kender Z, Friederich HC, Wild B. Associations of Childhood Neglect with the ACTH and Plasma Cortisol Stress Response in Patients with Type 2 Diabetes. Frontiers in Psychiatry. 2021; 12: 986.
- Bawa H, Poole L, Cooke D, Panagi L, Steptoe A, Hackett RA. Diabetes-related distress and daily cortisol output in people with Type 2 diabetes. Diabetes Research and Clinical Practice. 2020; 169: 108472.
- Skoranski A, Kelly NR, Radin RM, Thompson KA, Galescu O, Demidowich AP, et al. Relationship of mindfulness to distress and cortisol response in adolescent girls at-risk for type 2 diabetes. Journal of child and family studies, 2018; 27(7): 2254-2264.
- Akbarpour M, Ebrahimzadeh ZS. Effect of Spirulina supplementation and aerobic exercise on the level of cortisol and body composition in women with type 2 diabetes. Advancements in Life Sciences, 2019; 6(3): 116-124.

