When the Outpatient Physical Exam Returns, What Should it Look Like?
Alan C Kwan#, Hannah Hardy#, Robert J Siegel*
#Equal contribution
Department of Cardiology, Smidt Heart Institute, Cedars Sinai Medical Center, USA
Received Date: 14/09/2021; Published Date: 11/10/2021
*Corresponding author: Robert J Siegel, Department of Cardiology, Smidt Heart Institute, Cedars-Sinai Medical Center, 127 S. San Vicente Boulevard, Suite A3600, Los Angeles, California 90048, USA
Introduction
The COVID-19 pandemic, which forced us to rely on telemedicine [1], temporarily eliminated the in-person outpatient physical exam [2]. As the pandemic resolves, the opportunity to reassess the structure of outpatient medical visits is present [3]. We believe that the question of whether to ask patients to wear a gown for the cardiac exam deserves an objective evaluation. The superiority of stethoscope-to-skin evaluation for cardiopulmonary auscultation, although often marginal, is indisputable in cases with subtle findings. However, a high proportion of physicians, and in particular trainees, report examination and auscultation through covering garments despite understanding that this may negatively affect the quality of the examination [4]. The reason not to use a gown rests upon patient convenience. Therefore, we set out to objectively quantify positive and negative patient reactions to being asked to wear a gown as part of their physical examination.
Methods
We performed a pre-pandemic quality improvement survey (2019-2020) of patient perspectives of the gowned physical examination. Questionnaires were administered to 100 sequential patients of a single provider in an outpatient cardiology clinic immediately after their office visits. The questionnaires were optional, anonymous, and not distributed by the physician. The survey consisted of four statements with Likert scaling (strongly agree, agree, uncertain, disagree, or strongly disagree): “I feel that wearing a patient gown…” 1) …makes it easier for the doctor to perform a cardiovascular examination, 2) …allows the physician to more extensively and completely examine the heart and lungs, 3) …is part of a professional and comprehensive patient experience, and 4) …makes my clinic visit longer than it has to be. Additionally, there was an option to include “other recommendations to improve the patient visit.”
Results
Overall, of 100 offered questionnaires, 99 were completed the quantitative portion. All answer categories were represented in all questions at least once (Figure 1). The strongest agreement or disagreement was with the statement “I feel that wearing a patient gown makes it easier for the doctor to perform a cardiovascular examination,” with 89% of patients indicating agreement, and the majority strongly agreeing. There was frequent overall agreement (87%) for “I feel that wearing a patient gown allows the physician to more extensively and completely examine the heart and lungs.” Seventy-eight percent felt “that wearing a was part of a professional and comprehensive patient experience.” Eighty-six percent did not feel that wearing made the clinical visit unnecessarily longer. Fourteen patients left comments in the “recommendations to improve the patient visit”. Comments related to gowns were: “make gowns easier to close”, “nicer gowns”, “better gowns”, “get a smaller gown”, “it can be cold – so maybe a blanket over gowns as option”, “YES – wear gown”, “men should just take their shirts off and for women [the doctor] can work around the gown”. The patient who did not complete the quantitative portion of the questionnaire wrote “can hear well through my shirt" in this section.
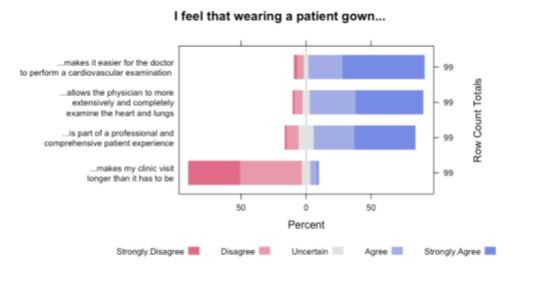
Figure 1: Likert Scale representation of the survey question answers.
Discussion
This study examined patient preferences regarding examination gowns in an outpatient cardiology setting. The cardio-pulmonary exam as well as examination of the skin, lymph nodes, joints, and other findings that may point to a myriad of disorders can only be discovered if evaluated. The results of our study suggest that in the eyes of our patients, a gowned examination offers a higher degree of completeness without an impression of wasted time. Overall, while there is room for improvement through better gown design, we see a positive impression towards the gowned experience.
We report our results to facilitate improving providers’ understanding of patient preferences as in-person visits resume. We acknowledge limitations of our study which originated as an internal quality improvement project, as single-center surveys may be affected by bias. As found during this pandemic, the in-person exam is not simply tradition, but also reflects a balance of risk and benefit: inconvenience and exposure to the medical system versus diagnostic information and patient preferences. If we impose on our patients the request to present in person, we should be obligated to pursue the highest effectiveness of the in-person visit. Our findings indicate that patients appreciate the gowned examination as a more thorough exam. As the pandemic resolves and we remake our medical practices, the gowned examination should be considered for optimizing the doctor-patient interaction.
Funding Sources: Alan C Kwan reports partial support from the Doris Duke Charitable Foundation Grant 2020059
Conflicts of Interest: The authors state no relevant conflicts of interest
References
- Khera A, Baum SJ, Gluckman TJ, Gulati M, Martin SS, Michos ED, et al. Continuity of care and outpatient management for patients with and at high risk for cardiovascular disease during the COVID-19 pandemic: a scientific statement from the American Society for Preventive Cardiology. American Journal of Preventive Cardiology, 2020; 1: 100009.
- Wosik J, Clowse ME, Overton R, Adagarla B, Economou-Zavlanos N, Cavalier J, et al. Impact of the COVID-19 pandemic on patterns of outpatient cardiovascular care. American Heart Journal, 2021; 231: 1-5.
- Fisk M, Livingstone A, Pit SW. Telehealth in the context of COVID-19: changing perspectives in Australia, the United Kingdom, and the United States. Journal of medical Internet research, 2020; 22: e19264.
- Rankin AJ, Rankin SH, Rankin AC. Auscultating heart and breath sounds through patients’ gowns: who does this and does it matter? Postgraduate medical journal, 2015; 91: 379-383.

