COVID-19: A Worldwide Pandemic Challenging Medical Science, Engineering, and Management
Cheryl Ann Alexander1* and Lidong Wang2
1Institute for IT innovation and Smart Health, Mississippi, USA
2Institute for Systems Engineering Research, Mississippi State University, Mississippi, USA
Received Date: 03/11/2020; Published Date: 11/12/2020
*Corresponding author:Cheryl Ann Alexander, Institute for IT innovation and Smart Health, Mississippi, USA. Email: tech.health.sol@gmail.com
Abstract
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and has been a worldwide pandemic. Although bats are regarded as the zoonotic source of SARS-CoV-2, this has not been confirmed and the intermediate host or whether there is an intermediate host remains unknown. Vaccines for COVID-19 are still in the process of development. There is no certified antiviral drug treatment for COVID-19. Mitigating the risk of COVID-19 is a systems engineering issue. A multidisciplinary, coordinated, and cross-sectoral approach based on One Health is required and collaborations among counties in the world are necessary; however, it is difficulty to develop One Health platforms or programs for COVID-19 among counties due to complicated reasons such as politics. During COVID-19, especially in the early stage of the pandemic, many counties had problems in medical supply chains and management, risk management, and disaster relief and operations. COVID-19 has posed challenges in medical science, engineering, and management. This paper introduces the similarities, distinct features, and novelties of COVID-19 compared with influenza SARS, and MERS. The infection and spread of COVID-19, the status of vaccines and therapeutics for COVID-19, and challenges during the pandemic are presented. The crisis management (such as resource allocation, operations, and logistics) and the use of telemedicine, Big Data analytics, Internet of Things (IoT) and artificial intelligence (AI) in fighting the COVID-19 pandemic are also discussed.
Keywords: COVID-19; SARS-CoV-2; SARS; MERS; Systems engineering; Management; Telemedicine; Big Data analytics; Internet of Things (IoT); Artificial Intelligence (AI)
Introduction
COVID-19 has become a worldwide pandemic. It is a novel coronavirus disease and can lead to Acute Respiratory Distress Syndrome (ARDS). Patients who develop ARDS are typically artificially oxygenated with a high-flow mechanical ventilation strategy which may cause a permanent or long-lasting impairment in lung function and fibrosis once they are discharged. Furthermore, in patients who may have been ventilated with protective tidal volumes and plateau pressures, higher driving pressures correlate with a deteriorating long-term pulmonary function and structure, stressing the probable role of driving pressure in lasting effects (Junior et al., 2018) [1].
COVID-19 is like predecessors such as SARS, Zika, Ebola, and avian influenza which are zoonotic, or starting in the animal population (Eddy et al., 2020) [2]. Lessons learned from viral disease outbreaks such as COVID-19 spotlight the global need to move to a more unified, proactive, and holistic paradigm, for example implementing the One Health method. One Health focuses on the relationships between the wellbeing of animals, plants, humans, and their shared environment. Therefore, this process fosters a deeper insight into and the capacity for addressing complex social and economic factors of health and successfully and effectively handle challenges via a coordination of services within sectors and disciplines. Although there is an intensified dedication to a global One Health approach, realizing a One Health approach in practice is still a challenge. The promotion of a nationwide One Health policy and platform could be essential to improve the management and assimilation of actions and platforms throughout most regions (Kelly et al., 2020) [3].
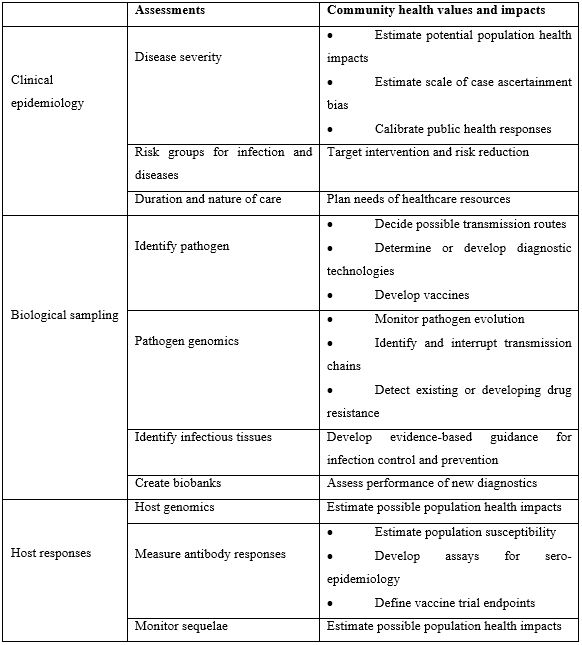
COVID-19 is a systems engineering issue that carries a great impact on public health. The systems engineering approach is necessary for governments to get a handle on all the aspects of this potentially fatal pandemic. Public health education had to be done without panicking the citizens while carefully controlling essential businesses and nonessential businesses. Table 1 (Rojek and Horby, 2016) [4] lists the public health values and impacts of some key factors which should be gathered from patients by interview or evaluation.
Table 1: Community health values and impacts of patient-centered evaluations.
The purpose of this paper is to present SARS-CoV-2, an introduction to COVID-19 features and challenges in medical science, engineering, and management. Influenza, MERS, and SARS are presented in comparison with COVID-19. A literature search was conducted on the EBSCO database using an ‘Advanced Search’. Papers were deemed suitable if in English, published between December 2019 and September 2020, and in peer-reviewed journals. Search terms included Novel Coronavirus, SARS-CoV-2, COVID-19, 2019-nCoV, influenza, SARS, and MERS. Only above-average papers were chosen for the review. The remainder of this paper is organized in sections: the second section presents influenza; the third section introduces SARS and MERS; section four explains SARS-CoV-2 and COVID-19; the fifth section is discussion; and the final section is a conclusion and future work.
Influenza
Influenza is a viral disease that can be categorized by Types A, B, or C and can cause a serious respiratory disease that can cause pneumonia and other serious illnesses. While the Influenza C virus typically results in a milder disease, Influenza virus Types A and B can cause seasonal epidemics (Witcher et al., 2019) [5]. It is estimated that seasonal influenza can cause as many as 79,400 US deaths and globally 291,243 to 645,832 deaths. The flu vaccine is the major approach for ameliorating the global effect of influenza. The flu virus, with a high case number and death rate correlated with annual or intermittent epidemics, is still at the frontline of community health research (Pleguezuelos et al., 2020) [6].
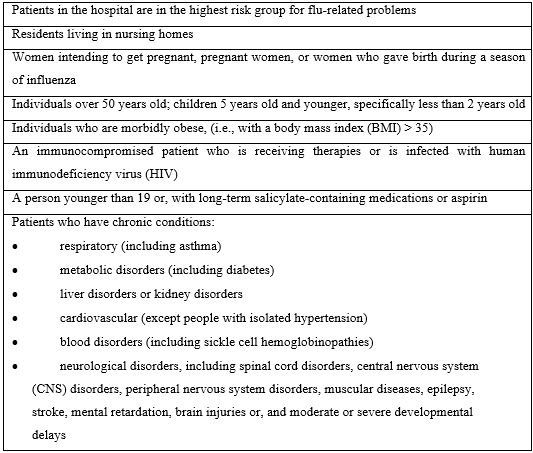
Flu vaccines are available in three distinct forms: cell based, egg based, and recombinant. Most influenza vaccines are manufactured from an embryo within a chicken egg infected with the flu virus. However, it is possible to produce new vaccines by using genomics and other methods (Boerner, 2020) [7]. One of the most frequent individual respiratory illnesses is the flu. Table 2 (Mastalerz-Migas et al., 2020) [8] lists individuals with the probability of developing flu-related problems.
Table 2: Individuals with highest risk of difficulties related to the flu.
SARS and MERS
The SARS pandemic started in winter 2002 to 2003 in China. It spread to Hong Kong, Singapore, Canada, etc. A decade later, the Middle East Respiratory Syndrome (MERS-CoV) surfaced in the Middle Eastern countries. After the SARS pandemic, 8422 cases were recorded in July 2003 with 916 (10.8 %) fatalities. Like SARS-CoV-2, SARS initially emerged in the live animal markets. Small mammals, like civet cats, are sold in these markets and viruses closely related to SARS-CoV have been found in these animals and other small animals. It is most likely that an animal to human transmission probably started at these markets. Although bats were the most likely natural reservoirs and palm civets the best choice for intermediate reservoirs of SARS-CoV, labs have also tailored it for lab cell cultures after isolating it from animals. Palm civets are also thought to have transmitted SARS-CoV to humans in an animal market (Habibzadeh and Stoneman, 2020; Hasöksüz et al., 2020) [9,10]. Most scholars think that many human-to-human transmission situations happened because of direct transmission through respiratory droplets while in close personal contact (Rabenau et al., 2005) [11].
When the first human case of MERS-CoV surfaced in Saudi Arabia, it immediately became a global health fear. Having turned up in 27 countries throughout four continents, MERS was recognized as one of the WHO Research and Development Blueprint priority pathogens (Ramshaw et al., 2019) [12]. A MERS infection straddles the gamut of clinical symptoms, varying from asymptomatic, mild, or severe respiratory symptoms, to death. Most human infections have been transmitted by another human infected with MERS (Rabbani et al., 2020) [13]. MERS produces respiratory symptoms when infected, such as fever, cough, shortness of breath, fatigue, myalgia, and some gastrointestinal symptoms including vomiting, nausea, etc. MERS can cause respiratory failure in cases of severe infections although some cases are asymptomatic. MERS will cause more serious complications when the patient is immunocompromised, such as with a history of lung disease, renal failure, or diabetes (Mutair and Ambani, 2020) [14]. Research reports have provided strong evidence that dromedaries are potential sources of human infection. Transmission of MERS from camels to humans occurs via direct contact with dromedary camels, which are the intermediate hosts, consumption of unpasteurized camel’s milk or raw meat and/or therapeutic usage of camel’s urine (Sayed et al., 2020) [15].
Unfortunately, MERS-CoV can cause a potentially fatal viral respiratory infection and currently, there are no definitive or successful therapeutics or vaccine for MERS. MERS-CoV vaccine candidates have been primarily focused on the viral spike (S) protein because it has a key role in virus transmissibility although other research is focusing on multiple additional viral proteins, for example, the nucleocapsid (N) protein, nonstructural protein 16 (NSP16), and envelope (E) protein have also been studied. Potential vaccine contenders can be cataloged by six categories: viral vector-based, inactivated-whole virus, subunits, a live-attenuated virus, DNA or RNA vaccines, and vaccines from nanoparticle-based viruses (Yong et al., 2019) [16]. At present, countries need to fortify community health systems and make resources available for the One Health agenda which focuses on the earliest detection of pandemics and preventing future MERS-CoV epidemics or other zoonotic viruses, for example, SARS and COVID-19 (Zumla et al., 2016) [17].
Unique Feature of SARS-CoV-2
Distinguishing between SARS-CoV-2 and COVID-19
SARS-CoV-2 is genetically like the SARS coronavirus of 2002 (SARS-CoV, also called SARS-CoV-1) (Kakodkar et al., 2020) [18]. Early in the outbreak of SARS-CoV-2, complete genomic sequences were gathered from patients during this stage; it was noted that the sequence was virtually indistinguishable from SARS-CoV-1 and shared 79.6% of the sequencing identity to SARS-CoV-1. Seven preserved non-structural proteins were analyzed using Pairwise Protein Sequence analysis of domains, which indicated that the SARS-CoV-2 virus belongs to the genus of Severe Acute Respiratory Syndrome-related Coronavirus (SARSr-CoV), and established that SARS-CoV-2 utilizes the identical cell entry receptor as SARS-CoV-1—Angiotensin Converting Enzyme II (ACE2)— (Zhou et al., 2020a) [19].
Although the zoonotic reservoir of SARS-CoV-2 has yet to be verified; bats should be the crucial reservoir based on a sequence-based analysis. Whether there is an intermediate host or not remains unclear, and the initial host is unknown, however, bats are the most likely animal (Ou et al., 2020; Shereen et al., 2020) [20,21]. COVID-19 is caused by an infectious virus and causes disease that has a rapid occurrence of recombination or replication in its positive element and as a result, the swift creation of new viral progeny cells occurs inside the host cell. SARS-CoV-2 apparently has a high rate of mutagenesis and can change structure; therefore, it has created an obstacle for both studies of the disease and the development of therapeutics (Vellingiri et al., 2020) [22].
Similarities and Distinct Features of COVID-19 Compared with the Common Flu, SARS, and MERS
People in many countries did not take COVID-19 seriously during the initial days of the virus because it was like MERS, SARS, and even influenza. More has been discovered about the distinctive characteristics of COVID-19 from the time when it became a global pandemic. The clinical features of SARS-CoV-1, SARS-CoV-2, and MERS-CoV are compared in Table 3 (Singh et al., 2020) [23].
Table 3: Clinical Features Comparison of MERS-CoV, SARS-CoV-1, and SARS-CoV-2.
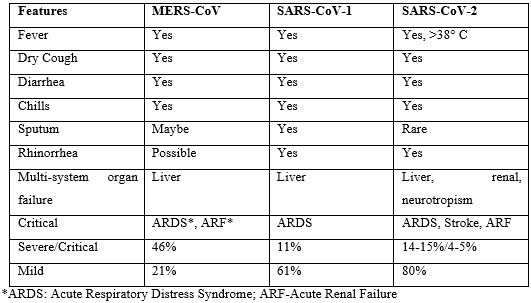
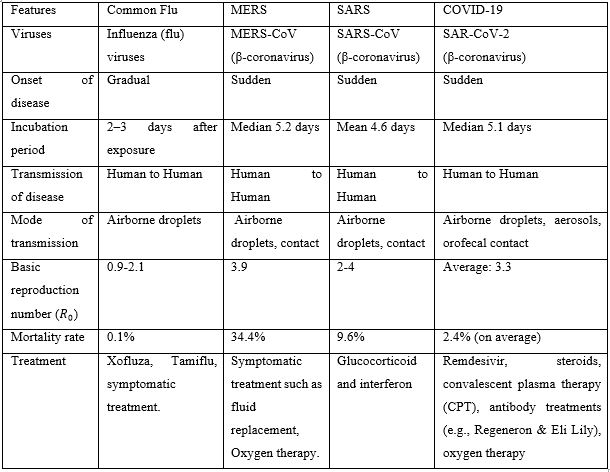
Table 4 shows a comparison between some common features for common flu, MERS, SARS, and COVID-19 (Cheung et al., 2020; Ou et al., 2020; Park, 2020; Shereen et al., 2020; Vellingiri et al., 2020) [20-22,24,25 ]. Individual differences and connections are also summarized. COVID-19 has an incubation period of normally 3-7 days; however, it may expand to as much as 14 days (Hatipoğlu, 2020) [26]. The essential reproduction number describes the typical number of new-found infections per person infected with SARS-CoV-2 in Table 4 (Neher et al., 2020) [27].
Table 4: Contrast of Common Flu, MERS, SARS, and COVID-19.
Infection and Spread of COVID-19
The highly transmissible nature of SARS–CoV-2 and the asymptomatic carrier or individual with mild symptoms contribute to the rapid rate of infection with COVID-19. An increase in the risk for fatal infections among patients with COVID-19 include age and whether the patient has any comorbid diseases. COVID-19 presents less severe clinical symptoms in children contrasted with adults, although children under one seem to manifest an increased risk for the critical illness. Current case-fatality rates estimate ranges between 0.6% to 7.2% according to region and seems to be substantially greater than the 0.1% mortality rate of seasonal flu (Cheng et al., 2020) [28]. Children are not always symptomatic, describing a lack of fever or cough as most adults normally report; these results would seem to indicate that COVID-19 does not always affect children strongly or in the same way as adults, often leaving them asymptomatic or with very mild symptoms which are hard to diagnose as COVID-19. Although children do not often present with the same signs and symptoms as adults, providers should still keep an elevated index of differential diagnoses for COVID-19 among children and monitor the status of those children with pre-existing conditions and infants under a year old, as these are the cases that tend to increase in severity. Individuals who are either asymptomatic or display mild symptoms are most likely to play a role in the acute transmissibility and spread of COVID-19 within the community; therefore, social distancing, masking, hand hygiene, and sanitizing surfaces are the preventive behaviors that can attenuate the transmission of the virus among individuals and slow the spread of infection (CDC, 2020) [29].
Although the main goal for containing the pandemic is to decrease the disease spread through a reduction of the number of individuals in the population who may be susceptible or by a reduction in the basic reproductive number (), it is important to note that R0 may be controlled by other aspects of the virus like the interval that viral shedding occurs, how infectious the virus may be, and an analyzation of the contact matrix among contaminated and vulnerable individuals (Cheng et al., 2020) [28]. Effective countermeasures to battle the onsite and precipitous increase of SARS-CoV-2 cases requires scholars to develop more effective instruments for understanding and monitoring the potential distribution of COVID-19 and the ongoing individual immune response (Grifoni, 2020) [30]. However, numerous issues yet persist unclearly, in spite of the hard work providers, researchers, and scientists have made to comprehend COVID-19 and its effects; for example, the existence of SARS-CoV-2 in patient stools has been found to demonstrate that this virus is most likely also transmitted via the orofecal route (Lai, 2020) [31].
Reductions in prevalence of SARS-CoV-2 could be due to successful interventions as well as seasonal change in transmissibility. Scholars must use cation when comparing total case trajectories from one region as a comparison to objectively utilize those same or similar predictions in another region, although they may be in a similar climate zone because sub-population dynamics may be excessively diverse. Although early in the pandemic, it was hypothesized that a seasonal variant would cause the virus to slow reproduction and attenuate, providing a much needed opportunity for healthcare systems to better prepare with the rapid development of therapeutics and vaccines (Liu, 2020b; Neher et al., 2020) [27,32]. However, the US spike in the pandemic during this summer demonstrated that climate has nothing to do with stopping the pandemic from attenuating or spreading; therefore, it is critical that therapeutics and vaccines be developed as soon as feasible to provide relief to overstressed, overwhelmed, and overpopulated intensive care units (ICUs) and much needed relief to healthcare workers. It is now apparent to scientists that the epidemic is not sensitive to rising temperatures and only the public health measures of social distancing, public masking, hand hygiene, mandated building ventilation changes, and surface sanitation measures can successfully mitigate the spread of COVID-19.
Vaccines and Therapeutics
Vaccines for COVID-19 are still in the process of development. There is no specific antiviral drug treatment for COVID-19, so the treatment of this disease is mainly focused on symptomatic treatment and oxygen therapy. It is also recommended that inflammatory markers, cascade factors, and lymphocyte subsets be monitored during treatment. Because most fatalities and sequelae of COVID-19 are from an immune, inflammatory response known as “cytokine storm”, which cause the ARDS and microthrombi well-documented in this virus, there needs to be a larger focus on immune-related and inflammatory-related research so that providers can get a deeper understanding of the pathogenesis, treatment of the disease can be better guided, and the prognosis can be improved (Lin, 2020) [33].
SARS-CoV-2 is human β-coronavirus (HCoVs). An efficient strategy of discovering drugs to treat COVID-19 is drug repurposing, or using existing drugs meant for another purpose; this could diminish the time and decrease costs in contrast to de novo drug discovery. An integrative and antiviral drug repurposing method was presented that implements a network medication stand centered on systems pharmacology and quantifies the interaction among the HCoV–host interactome and drug targets within the human protein-to-protein interaction network. Powerful system-based methods have been offered for a swift recognition of repurposable drugs that may be candidates for COVID-19 treatment and possible combinations of drugs that target SARS-CoV-2 (Zhou et al., 2020b) [34]. Lopinavir, Ritonavir, and Oseltamivir are currently being studied to determine their effectiveness against COVID-19. The WHO touted a vote of faith on February 24, 2020, the antiviral drug, Remdesivir, a product of Gilead Sciences experiment in the treatment of Ebola; the WHO indicated that Remdesivir had enormous possibilities and was most likely the top candidate and the most hopeful therapy as a therapeutic for COVID-19. Currently, Remdesivir is in ongoing randomized clinical trials, but it has yet to be approved by the US FDA but can be given in an off-label capacity in an emergency access in the US by providers. Remdesivir is also accessible to patients infected with COVID-19 by enrolling in a clinical trial (Cao, 2020; Sanders, 2020; Shereen et al., 2020) [21,35,36].
Traditional Chinese Medicine (TCM) helps cure COVID-19. TCM can block the progression of COVID-19-acquired pneumonias or respiratory infection. Qingfei Paidu Decoction has been utilized as a COVID-19 treatment and originates from a mixture of five classical prescriptions of TCM; it also contains chemicals which have also shown the effect of inhibiting the 3CL protein of the human β-coronavirus. Another clinical formula of TCM based on clinical experience is Pneumonia No.1 Formula (i.e., "Thoroughly Resolving Antifungal Granules") and can also help in the treatment of COVID-19; it is established on traditional Chinese principles of removing heat and toxic substances, dispelling wind and penetrating the exterior, and stimulating qi while feeding yin. For the treatment of a mild case of COVID-19 pneumonia, there is the therapeutic Shufeng Jiedu Capsule (SFJDC) in combination with arbidol, which can have a good quality antiviral effect on respiratory symptoms (Liu, 2020a) [37].
Discussions
The origins of SARS-CoV-2 has never been conclusively determined although the virus had been found in the environmental samples at the Wuhan, China wet market. However, the initial patient and 13 out of 41 other patients had no contact with the Huanan wet market, making the likelihood of this being the official origin highly suspicious. And the first treated patient did not share an epidemiological link with other patients in the cohort. It has been suggested by US officials, some Chinese citizens, and others, that the initial site of infection came from a lab in Wuhan that had experienced some safety breaches in 2018. It was also immediately prior to the Chinese New Year and travel to the region had greatly increased, furthering the possibility that there was more than one source of contamination by the host animal. It is also not clear if SARS-CoV-2 directly infected the initial human host via a bat or an intermediate host (Xu, 2020) [38]. Future research is necessary to experiment further with this virus and the hosts.
Direct-to-consumer telemedicine is beneficial during the pandemic and could potentially cause a significant decrease of in-person patient visits, which could promote self-quarantine and reduce overcrowding of the emergency department. Additionally, telehealth can provide remote monitoring of patients recently discharged with verified COVID-19, a critical measure to contain the pandemic, especially among healthcare providers (Moazzami et al., 2020) [39]. In remote consultations during the pandemic, screening questions were done for COVID-19 at the time of referral or during initial triage; a review of all pre-existing nonurgent provider appointments were appraised for clinical risk and then revised and conducted via the internet, FaceTime, or phone after consent of the patient was obtained. In rural areas and disparate urban areas, reviews were done via telehealth and the face to face provider assessment was limited to high-risk individuals or for those patients requesting it only after a discussion on infection control strategy was done (Kavoor et al., 2020) [40]. Big Data analytics, Internet of Things (IoT), and artificial intelligence (AI) help fight against COVID-19. Specifically, AI helps: 1) provide updated information based on real-time data analysis and prevent the spread of the disease; 2) diagnose and provide treatment early using decision science and digital technologies, thus reducing the workload of healthcare workers; 3) devise new diagnoses and management systems for COVID-19 cases (Vaishya et al., 2020) [41].
There is much work in managing the crisis, including case identification and contact tracking, proactive case finding, quarantine of potential cases, relief to businesses, allocation of resources (e.g., testing, assessing and managing capacity, operations and logistics, etc.), reassurance and education of the public while fighting misinformation, formulation of policies toward childcare and schools, strict control of the borders from land, air, and sea, while negotiating with additional infected countries and regions (Wang et al., 2020a) [42]. Due to the shortage of medical supplies during the SARS-CoV-2 pandemic, developing global cooperative systems to deal jointly with public health emergencies of a global nature (e.g., One Health) in the future (Wang et al., 2020b) [43].
Conclusion and Future Work
Many countries did not take COVID-19 seriously in the early months of COVID-19 due to similar clinical features to MERS, SARS, and even influenza. But COVID-19 does have some distinct features. For example, in COVID-19, the patient could potentially experience the likely fatal cytokine storm which causes ARDS, clotting abnormalities, and neurotropisms. The incubation period of COVID-19 begin after exposure as quickly as 3-5 days yet can extend up to 14 days. The high transmissibility of SARS–CoV-2 and pre-symptomatic or asymptomatic transmissions lead to the difficulty of controlling the prevailing spread of COVID-19. SARS-CoV-2 can be transmitted via droplet, aerosols, the orofecal route, or contact with a contaminated surface. Although COVID-19 cannot live on surfaces exposed to the UV light of the sun more than 30 minutes, it can live on steel, cardboard, paper, and other surfaces for many hours if not exposed to sanitation or UV light, thus infecting the person who may innocently touch the surface and then touch a mucous membrane. Even if the caregiver or provider is wearing an N95 mask, but touches a surface and then their eye, a conjunctivitis can result in a full-blown COVID-19 infection. Although most social distancing measures implemented are for six feet, a poorly ventilated room can facilitate the spread of aerosols for up to more than 60 feet. Frequent handwashing, sanitizing of surfaces, using hand sanitizer with at least a 75% alcohol content, and social distancing measures should be enforced within highly infected regions. Cloth masks can reduce the spread of COVID-19 by up to 17%, a simple surgical mask can reduce the infection by 33%, but an N95 mask may reduce the chance of infection for up to 77%. However, properly fitting masks, remembering not to touch the mask, and changing or washing the mask often is necessary to avoid contaminating oneself with the mask.
Further research on COVID-19 needs to be conducted to deal with challenges in medical science, systems engineering, and management. It is significant to confirm the zoonotic source of SARS-CoV-2 and identify any intermediate host (if it exists). Many countries are speeding up the development process of specific therapeutics and vaccines for COVID-19. Telemedicine, IoT, AI, and Big Data analytics help mitigate the risk of COVID-19. A systems engineering methodology based on One Health for the control of COVID-19, medical supply chains management and operations research on fighting COVID-19, and Big Data analytics for the prediction of trends and infection cases of COVID-19 and future pandemics are our future research topics.
Acknowledgements
Authors thank Technology & Healthcare Solutions, Mississippi, USA for support.
Conflicts of Interest
There is no conflict of interest.
References
- Junior CT, Santiago RRDS, Hirota AS, Carvalho ARS, Gomes S, Amato MBP, et al. Driving pressure and long-term outcomes in moderate/severe acute respiratory distress syndrome. Annals of intensive care, 2018; 8(1): 119.
- Eddy C, Schuster R, Sase E. An All-Hazards Approach to Pandemic COVID-19: Clarifying Pathogen Transmission Pathways toward the Public Health Response. Journal of Environmental Health, 2020; 82(9): 28-35.
- Kelly TR, Machalaba C, Karesh WB, Crook PZ, Gilardi K, Nziza J, et al. Implementing One Health approaches to confront emerging and re-emerging zoonotic disease threats: lessons from PREDICT. One Health Outlook, 2020; 2(1): 1-7.
- Rojek AM, Horby PW. Modernising epidemic science: enabling patient-centred research during epidemics. BMC medicine, 2016; 14(1): 212.
- Witcher R, Tracy J, Santos L, Chopra A. Outcomes and Adverse Effects with Peramivir for the Treatment of Influenza H1N1 in Critically Ill Pediatric Patients. The Journal of Pediatric Pharmacology and Therapeutics, 2019; 24(6): 497-503.
- Pleguezuelos O, James E, Fernandez A, Lopes V, Rosas LA, Cervantes-Medina A, et al. Efficacy of FLU-v, a broad-spectrum influenza vaccine, in a randomized phase IIb human influenza challenge study. NPJ vaccines, 2020; 5(1): 1-9.
- Boerner LK. The Flu Shot and the Egg. ACS Central Science, 2020; 6: 89−92.
- Mastalerz-Migas A, Kuchar E, Nitsch-Osuch A, Mamcarz A, Sybilski A, Wełnicki M, et al. Recommendations for the prevention, diagnosis and treatment of inFLUenza in adults for Primary care physiciAnS: FLU COMPAS PCP–ADULTS. Family Medicine & Primary Care Review, 2020; 22(1): 81-96.
- Habibzadeh P, Stoneman EK. The novel coronavirus: a bird's eye view. The international journal of occupational and environmental medicine, 2020; 11(2): 65-71.
- Hasöksüz M, Kiliç S, Saraç F. Coronaviruses and SARS-CoV-2. Turkish Journal of Medical Sciences, 2020; 50(SI-1): 549-556.
- Rabenau HF, Cinatl J, Morgenstern B, Bauer G, Preiser W, Doerr HW. Stability and inactivation of SARS coronavirus. Medical microbiology and immunology, 2005; 194(1-2): 1-6.
- Ramshaw RE, Letourneau ID, Hong AY, Hon J, Morgan JD, Osborne JC, et al. A database of geopositioned Middle East Respiratory Syndrome Coronavirus occurrences. Scientific data, 2019; 6(1): 1-13.
- Rabbani SA, Mustafa F, Mahtab A. Middle East Respiratory Syndrome (MERS): Awareness among Future Health Care Providers of United Arab Emirates. International Journal of Medicine and Public Health, 2020; 10(1): 8-13.
- Mutair AA, Ambani Z. Narrative review of Middle East respiratory syndrome coronavirus (MERS-CoV) infection: updates and implications for practice. Journal of International Medical Research, 2020; 48(1): 1-6.
- Sayed AS, Malek SS, Abushahba MF. Seroprevalence of Middle East Respiratory Syndrome Corona Virus in dromedaries and their traders in upper Egypt. The Journal of Infection in Developing Countries, 2020; 14(02): 191-198.
- Yong CY, Ong HK, Yeap SK, Ho KL, Tan WS. Recent advances in the vaccine development against Middle East respiratory syndrome-coronavirus. Frontiers in microbiology, 2019; 10: 1781.
- Zumla A, Alagaili AN, Cotten M, Azhar EI. Infectious diseases epidemic threats and mass gatherings: refocusing global attention on the continuing spread of the Middle East Respiratory syndrome coronavirus (MERS-CoV). BMC medicine, 2016; 14(1): 1-4.
- Kakodkar P, Kaka N, Baig MN. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19). Cureus, 2020; 12(4): e7560.
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature, 2020a; 579(7798): 270-273.
- Ou X, Liu Y, Lei X, Li P, Mi D, Ren L, et al. Characterization of spike glycoprotein of SARS-CoV-2 on virus entry and its immune cross-reactivity with SARS-CoV. Nature communications, 2020; 11(1): 1-12.
- Shereen MA, Khan S, Kazmi A, Bashir N, Siddique, R. COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research, 2020; 24: 91–98.
- Vellingiri B, Jayaramayya K, Iyer M, Narayanasamy A, Govindasamy V, Giridharan B, et al. COVID-19: A promising cure for the global panic. Science of the Total Environment, 2020; 725: 138277.
- Singh A, Shaikh A, Singh R, Singh AK. COVID-19: From bench to bed side. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2020; 14: 277-281.
- Cheung KS, Hung IF, Chan PP, Lung KC, Tso E, Liu R, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from the Hong Kong cohort and systematic review and meta-analysis. Gastroenterology, 2020; 1-45.
- Park SE. Epidemiology, virology, and clinical features of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clinical and experimental pediatrics, 2020; 63(4): 119-124.
- Hatipoğlu N. The" New" Problem of Humanity: New Coronavirus (2019-nCoV/COVID-19) Disease. Medical Journal of Bakirkoy, 2020; 16(1): 1-8.
- Neher RA, Dyrdak R, Druelle V, Hodcroft EB, Albert J. Potential impact of seasonal forcing on a SARS-CoV-2 pandemic. Swiss medical weekly, 2020; 150: w20224.
- Cheng MP, Papenburg J, Desjardins M, Kanjilal S, Quach C, Libman M, et al. Diagnostic testing for severe acute respiratory syndrome–related coronavirus-2: A narrative review. Annals of internal medicine, 2020; 1-10, doi:10.7326/M20-1301.
- CDC COVID-19 Response Team. Coronavirus Disease 2019 in Children—United States, February 12–April 2, 2020. Morbidity and Mortality Weekly Report, 2020; 69(14): 422-426.
- Grifoni A, Sidney J, Zhang Y, Scheuermann RH, Peters B, Sette A. A sequence homology and bioinformatic approach can predict candidate targets for immune responses to SARS-CoV-2. Cell host & microbe, 2020; 27: 671–680.
- Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and corona virus disease-2019 (COVID-19): the epidemic and the challenges. International journal of antimicrobial agents, 2020; 55: 105924.
- Liu J, Zhou J, Yao J, Zhang X, Li L, Xu X, et al. Impact of meteorological factors on the COVID-19 transmission: A multi-city study in China. Science of the Total Environment, 2020b; 726: 138513.
- Lin L, Lu L, Cao W, Li T. Hypothesis for potential pathogenesis of SARS-CoV-2 infection–a review of immune changes in patients with viral pneumonia. Emerging microbes & infections, 2020; 9(1): 727-732.
- Zhou Y, Hou Y, Shen J, Huang Y, Martin W, Cheng F. Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2. Cell discovery, 2020b; 6(1): 1-18.
- Cao YC, Deng QX, Dai SX. Remdesivir for severe acute respiratory syndrome coronavirus 2 causing COVID-19: An evaluation of the evidence. Travel Medicine and Infectious Disease, 2020; 101647.
- Sanders JM, Monogue ML, Jodlowski TZ, Cutrell JB. Pharmacologic treatments for coronavirus disease 2019 (COVID-19): a review. Jama, 2020; 323(18): 1824-1836.
- Liu CX. Pay attention to situation of SARS-CoV-2 and TCM advantages in treatment of novel coronavirus infection. Chinese Herbal Medicines, 2020a; 1-8.
- Xu Y. Unveiling the Origin and Transmission of 2019-nCoV. Trends in microbiology, 2020; 28(4): 239-240.
- Moazzami B, Razavi-Khorasani N, Moghadam AD, Farokhi E, Rezaei N. COVID-19 and telemedicine: Immediate action required for maintaining healthcare providers well-being. Journal of Clinical Virology, 2020; 126: 104345.
- Kavoor AR, Chakravarthy K, John T. Remote consultations in the era of COVID-19 pandemic: Preliminary experience in a regional Australian public acute mental health care setting. Asian Journal of Psychiatry, 2020; 51: 102074.
- Vaishya R, Javaid M, Khan IH, Haleem A. Artificial Intelligence (AI) applications for COVID-19 pandemic. Diabetes & Metabolic Syndrome: Clinical Research & Reviews, 2020; 14: 337-339.
- Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. Jama, 2020a; 323(14): 1341-1342.
- Wang X, Zhang X, He J. Challenges to the system of reserve medical supplies for public health emergencies: reflections on the outbreak of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic in China. Bioscience trends, 2020b; 14(1): 3-8.

