How to Optimised Oncological Treatments: Lessons Learned from the First covid-19 wave
López E1*, Kechagioglou P2, O’Brien P3, Moreno-Olmedo E4, Gonsalves-Pieretti D5, Suárez-Gironzini V6, Fusco JP7, Lewi S8
1Department of Radiation Oncology, La Milagrosa Hospital. Madrid.Chief Medical Officer Genesis Care, Spain
2Department of Clinical Oncology. Windsor. Chief Medical Officer Genesis Care, United Kingdom
3Department of Radiation Oncology. Conjoint Associate Professor. University of Newcastle, Australia
4Department of Radiation Oncology, La Milagrosa Hospital. Madrid. Genesis Care, Spain
5Department of Radiation Oncology. Jerez. Genesis Care, Spain
6Department of Radiation Oncology, La Milagrosa Hospital. Madrid. Radiation Oncology Deputy Genesis Care, Spain
7Department of Medical Oncology, La Milagrosa Hospital. Madrid. Medical Oncology Deputy Genesis Care, Spain
8Global Head of Quality, Alexandria NSW, Australia
Received Date: 22/10/2020; Published Date: 30/11/2020
*Corresponding author: López E. MD, PhD. Department of Radiation Oncology La Milagrosa Hospital. Madrid. GenesisCare Spain. Email: escarlata.lopez@genesiscare.es, Telephone: +34 606 509672
Abstract
Despite the local idiosyncrasies and different viral disease epidemiology resulting in country-specific governmental measures, our 70 centers located in Australia (32), United Kingdom (15) and Spain (21) joined forces and shared knowledge and experiences, which supported an appropriate clinical strategy for each country. The supply of Radio Therapy (RT) and/or Chemo Therapy (CT), and the safeguard of patients and staff in regard to their infectious status have been our priorities. In order to classify the changes in practice made during this pandemic we divide them into four major pillars that have impacted our culture and processes: oncology treatment, infection control, Information Technology (IT) infrastructure and staff connectedness. Facing a health crisis, the doctor leadership should be consolidated and for this reason, a high engagement of our doctors across the network is an essential key point. The oncology sanitary system should be continuously reinforced and should also be flexible plus solid.
Keywords: COVID-19; Chemotherapy; Leadership; Oncology; Radiotherapy; Staff
Introduction
In the first literature report of COVID-19 infection in oncologic patients the authors suggested three major strategies that would represent the backbone in delivery of oncologic treatments [1]. First, postponing adjuvant treatment or elective surgery. Second, personal protection for patient with cancer, cancer survivors and staff. Third, intensive surveillance or treatment in COVID positive patients with cancer.
During this pandemic, Spain was the first of the countries belonging to the Genesis Care (GC) international network affected by this outbreak. The first case in Spain for SARS-CoV-2 was diagnosed on 31 January 2020. By 13 March, cases had been confirmed in all 50 provinces of the country. From 17 March to 14 April, the death rate in Spain was 68% higher than usual and 21,882 excess deaths were recorded. The peak of excess deaths occurred during the week of 27 March to 3 April and was five times larger than the flu season of 2019.
Thus, Spain faced the main challenge to integrate strategies to minimize the deleterious effect of delayed diagnosis and treatment in cancer patients considering new ways of treating them, avoiding to postpone the start of treatments.
Despite the local idiosyncrasies and different viral disease epidemiology resulting in country-specific governmental measures, the three national chief medical officers of our 70 centers located in Australia (32), United Kingdom (15) and Spain (21) joined forces and shared knowledge and experiences, which supported an appropriate clinical strategy for each country. The supply of radiotherapy (RT) and/or chemotherapy (CT), and the safeguard of patients and staff in regard to their infectious status have been our priorities [2,3].
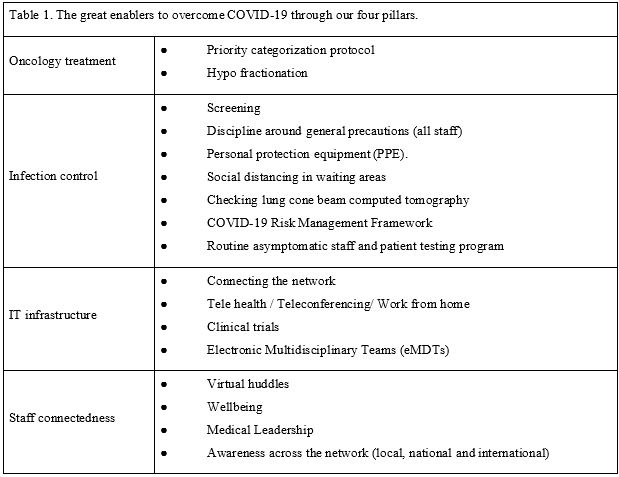
In order to classify the changes in practice made during this pandemic we divide them into four major pillars that have impacted our culture and processes: oncology treatment, infection control, Information Technology (IT) infrastructure and staff connectedness. The great enablers that have facilitated to treat our patients during the COVID-19 pandemics through the four pillars are shown in Table 1.
Table 1: The great enablers to overcome COVID-19 through our four pillars: oncology treatment, infection control, information technology (IT) infrastructure and staff connectedness
Our first pillar is oncology treatment looking for efficacy measures, we implemented two strategies: 1) To apply a tumor categorization protocol (Table 2) to determine the priority for RT delivery. Based on different factors such as tumor type and staging, intention-to-treat,
Table 2: Priority categorization protocol.
RT= Radiotherapy. SVCS= Superior Vena Cava Syndrome. SCLC= Small Cell Lung Cancer. SBRT= Stereotactic Body Radiotherapy. SPOT= non-melanoma skin cancer.9
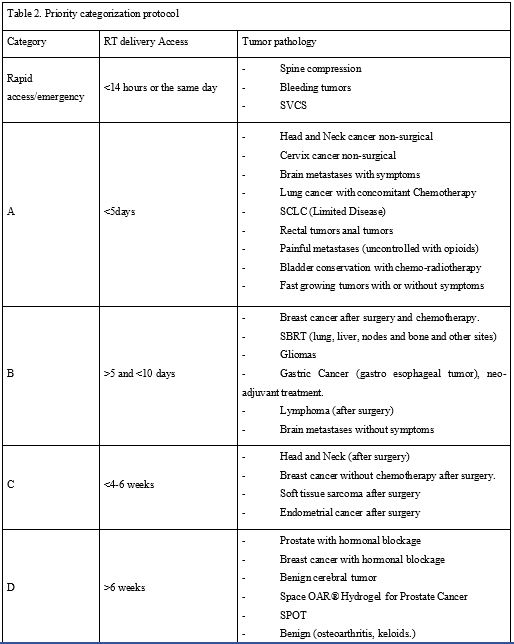
General patient performance status and potential radiotherapy schedule approach, we classified the patients into 5 categories: rapid access/emergency radiotherapy (<14 hours or in the same day), A (<5days), B (>5 and <10 days), C (<4-6 weeks) and D (>6 weeks). This has allowed us, in an unprecedented situation, to balance the risk and benefit between treatments versus prevention of virus infection. 2) To increase the rate of hypo fractionated radiotherapy, achieving the same effectiveness with fewer sessions, in order to increase capacity in radiotherapy departments and reduce patient footfall in our centers. For instance, following the results of the Fast Forward trial, breast RT extreme hypo fractionation (26Gy/5#) is now an option for eligible patients (in two weeks we treated more than 90 patients). Similarly, in prostate cancer, moderate and ultra-hypo fractionation protocols such as 20# daily, 5# SABR and weekly 6# (total 36Gy) have been accepted as evidence-based protocols. Finally, for lung cancer patients who are also vulnerable to respiratory illness, a SABR regimen can be considered to standard fractionation. Staff and doctors have worked together to enable the implementation of the above protocols.
Regarding infection control, symptoms screening in patients and personnel before entering an oncology center presented an opportunity to identify possible cases with COVID-19 [4]. Discipline around general precautions by all staff including doctors and reinforcing the cleaning was used in order to keep a clean circuit. Besides, security lines, fixed screens for administrative staff and social distancing in waiting areas by re-arranging sitting areas to keep the 2m rule were performed and may remain as a global social change. The appropriate combination of personal protection equipment (PPE), selected through a risk assessment, was also used for infection prevention. Other useful measures were: Checking lung cone beam computed tomography of all patients with lung, breast or gastrointestinal superior cancers. This allowed not only to check the PTV we were treating but also to detect any abnormality which might be consistent with COVID-19. All these measures are included in our COVID-19 risk management framework [5] which should continue besides testing patients and staff when they screen positive for symptoms, with isolation measures in case of positive testing. An incidence was raised for any patient delay due to COVID-19 through a Multidisciplinary Team (MDT). COVID-MDT met with patient’s doctor, CMO and center manager to decide on patient treatment in case of positive swab for covid-19 [3]. A decision to treat end of day or delay treatment based on risks and benefits was made at the MDT. From our experience, we encourage the case-by-case assessment by a specialized board in future cases. Furthermore, routine asymptomatic staff and patient testing program should rule out to keep centers COVID-19 clean. In the first rapid testing around a 10.47% of our staff in Spain has been in contact with the disease and has generated IgG immunity.
Our third pillar is the IT infrastructure supporting a global network where some activities continued to ensure efficiency. A high percentage of staff members have worked from home through remote access to their platforms, having access to patient history and treatment planners (tele health). Oncologic follow ups were done by phone to reduce the people flow in the centers. Long survival follow-up (> 5 years) were also continued by phone with rapid access if it was needed. Also, psycho-oncologic attention was delivered by phone/digital media. The educational programs were done as Webinars and virtual congresses (teleconferencing). Electronic multidisciplinary teams (eMDT) were established at a time when clinician collaboration for patient care was more needed than ever [6]. It is run through a remote and safe platform, where clinicians can join in a synchronous or asynchronous way, record decisions and share report with the doctor, referrer, GP and patient if they so wish. To increase the communication through the whole network has been one of our priorities.
On the other hand, research continued for life saving trials and trials in set up. Two studies have been developed: Low doses of lung radiation therapy in cases of COVID-19 pneumonia: prospective, multicentric study in Radiation Oncology Centers (ClinicalTrials.gov Identifier: NCT04394182) and Genesis Care UK SARS-CoV-2 Antibody testing Program (both ongoing).
Our fourth pillar is staff connectedness. Regional managers and function managers worked very close to help physician unit coordinators with daily COVID-19 virtual huddles to discuss operational and quality issues and make decisions about center backup e.g.: minimizing the number of staff on site treating patients, having a schedule of backup in case staff fall ill, fewer face to face meetings and more virtual meetings, with staff spending more time home with their families and having time for home schooling Awareness across the network (local, national and international) has increased and this has fed into wellbeing. These plus the exercise and wellbeing program together with a strong medical leadership as part of the Integrative Cancer Care (ICC) holistic vision has led to the emergence of a solid team concept (“All for one and one for all”) that has generated a very strong engagement.
Our Oncology Departments have done a huge job, in a very short time. But now, with deescalated measures in Spain and other countries, we are presented with a unique opportunity to be a part of a cultural transformation in Oncology: The challenge of renaissance in the era post-COVID-19.
Some of the changes in practice which occurred in the COVID era are here to stay for several reasons. They improve patient and staff safety, lead to operational efficiencies, and efficacy in treatment, improve quality and team workflow and engagement. In addition, by continuing such strategies, we can be ready in case of another wave of this or a similar pandemic. This is an example of flexibility in our company, not only we have adapted to the difficult situation but also, we have learnt (innovation and improvement). Facing a health crisis, the doctor leadership should be consolidated and for this reason, a high engagement of our doctors across the network is an essential key point. The oncology sanitary system should be continuously reinforced and should be flexible plus solid as an accordion.
References:
- Liang W, Guan W, Chen R. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020. doi: 10.1016/S1470-2045(20): 30096-6.
- Portaluri M, Banbace S, Tramacere F, Errico A, Carbone S, Portaluri T. Stall and patients´protection in radiation oncology departmentes during COVID-19 pandemic. Advances in Radiation Oncology. 2020.
- Simcock R, Vengaloor T, Mercy CE, Filippi AR, Katz MA, Pereira IJ, Saeed H. COVID-19: Global Radiation Oncology’s Targeted Response for Pandemic Preparedness. Clin Trans Oncol. PII: S2405 2020; 6308(20): 30022-30027. DOI: 10.1016/j.ctro.2020.03.009
- Associazione Italiana de Radioterapia Oncologica (AIRO). Documento de indirizzo per la valutazione e la gestione del rischio dei pazienti e degli operatori nei reparti de radioterapia oncológica in corso di diffusione del COVID-19. 19 March. 2020.
- Suárez V, Moreno-Olmedo E, Pérez M, González J, Rivas D, Fusco J, Kechagioglou P, López E. Spanish Risk Management Framework across 17 Radiation Oncology Centers during COVID-19 pandemic. Radiat Oncol, 2020; 148: 267-269.
- Prades J, Remue E, van Hoof E, Borras JM. Is it Worth Reorganising Cancer Services on the Basis of Multidisciplinary Teams (MDTs) a systematic review of the objectives and organization of MDTs and their impact on patient outcomes? Health policy, 2015; 119 (4): 464-474.

