The New Norm in an Academic Medical Centre in the Post COVID-19 World: Finding Opportunities in Challenges; How to Adapt, Innovate and Thrive
Lateef F*
Senior Consultant/ Director of Training and Education, Department of Emergency Medicine, Singapore General Hospital; Professor, Dukes-NUS Graduate Medical School and Yong Loo Lin School of Medicine, National University of Singapore; Director, Singhealth Duke NUS Institute of Medical Simulation, Singapore
Received Date: 10/09/2020; Published Date: 25/11/2020
*Corresponding author: Fatimah Lateef, Senior Consultant/ Director of Training and Education, Department of Emergency Medicine, Singapore General Hospital; Professor, Dukes-NUS Graduate Medical School and Yong Loo Lin School of Medicine, National University of Singapore; Director, Singhealth Duke NUS Institute of Medical Simulation, Singapore. E-mail: fatimah.abd.lateef@sgh.com.sg
Abstract
COVID-19 has affected every country and every healthcare system throughout the world. Work flow in our healthcare institutions across Singapore changed quickly to a pandemic model of preparedness which we have trained for and executed previously with other outbreaks of infectious diseases such as Severe Acute Respiratory Syndrome (SARS). Our healthcare organization at Sing Health Duke NUS Academic Medical Centre (AMC), represent a complex system. As such the preparedness plans are also multi-faceted, multi-layered, multi-disciplinary and are made up of multiple algorithmic steps. As we reach a stable state with the numbers of COVID 19 positive cases trending downwards and the community spread almost negligible now, new norms and new practices have become embedded in the population, businesses, systems, organizations, industries and schools. At our AMC, this was also the case. Work has begun on many fronts and the positive ripple effects are already becoming apparent. As we reset ourselves for the new normal, our AMC has identified 5 attributes/ domains to guide our paradigm in the face of a new world. These are known as the 5 Ps: People, Patients, Places (Infrastructure Development), Programmes and (Pandemic) Preparedness. In this commentary, the author shares her views on the changes and the healthcare practices during and post COVID 19. The author is a senior consultant Emergency Physician, who had served as an elected Member of Parliament for 15 years in Singapore. She has retired from politics on 23rd June 2020.
Keywords: COVID-19, Cross-training, Academic Medical Centre, Preparedness; Post COVID-19
Introduction
The COVID 19 pandemic represents an inflection point in our history, affecting our lives and livelihood. It continues to ravage the world as we chart our course and plan our footprints into the future. It is leaving us with many challenges and multiple lessons. Just like with previous outbreaks (eg. SARS, MERS, Ebola), many changes and evolution in healthcare have been sparked off from these experiences. It is all part of the lessons we learn from a crisis and the opportunities we create through the challenges we encounter. Due to COVID 19, certain adoption and adaptation, as well as disruption have been brought forward. These served as the impetus for change, for us to accelerate our plans, drive innovation, capitalize on technology and also transform how we deliver healthcare and other services. These are all encompassing and are integrated across many sectors.
COVID 19 transformed into a pandemic within a relatively short period of time due to high levels of infectivity, including spread by pre-symptomatic and asymptomatic patients. This led to massive numbers of cases in most affected countries. The infection came in waves; whilst some countries saw the numbers infected risevery rapidly in the early stages (eg. China, Europe), other countries only started seeing their first wave much later on ( eg. South America, some states of the United States of America). Both scientists and clinicians struggled to get more information to help in the treatment and ultimate vaccine production, especially in the early days of the pandemic [1-3] Change became a constant, whether it was in workflow, case definition or infectivity, as new findings and observations were evolving and begun to be shared globally. As a result, the COVID 19 pandemic was one that brought about transformative changes, most suited to train the future-ready clinician, medical educators and researchers. It also presented us with a variety of choices for the future, of which our selection will contribute towards the reshaping of healthcare and perhaps, even society.
The Academic Medical Centre in Singapore
Singapore General Hospital (SGH), the oldest and largest training hospital in Singapore forms an Academic Medical Centre with the Duke NUS (National University of Singapore) Graduate Medical School. SGH has 1800 inpatient beds, across 36 different specialties and the Emergency Department serves about 140 000 attendances annually [4]. An Academic Medical Centre (AMC) is a tertiary care hospital that is integrated with a medical school. The hospital is the primary site of education for undergraduates of the medical school as well as post-graduate medical trainees from affiliated medical schools. It conducts medical, academic and research activities utilizing a variety of approved and recognized protocols involving patients in the hospital [5].
In addition to the above definition, JCI (Joint Commission International) accredited academic medical centers must meet some additional criteria: [5]
- The hospital is organizationally or administratively integrated with a medical school.
- At the time of application for accreditation, the hospital is conducting medical research with approval and oversight by an Institutional Review Board (IRB) or research ethics committee.
Being a large organization, infection control training and our emergency preparedness processes and responses are also multi-layered, multi-faceted and complex. Since the SARS (Severe Acute Respiratory Syndrome) outbreak in 2003, the Emergency Department (ED), as well as other departments at Singapore General Hospital (SGH) had undergone changes in both its infection control infrastructure as well as work flow processes [6,7]. These are critical and essential elements in preparedness for handling crises, mass casualty incidents, infectious diseases outbreaks or pandemics. The specialty of Infectious Diseases too has developed further with more specialists, residents-in-training as well as more organized and structured facilities such as negative pressure and isolation rooms, since 17 years ago. These have become part and parcel of our day to day practice. What is important is that these practices remain dynamic and their details are regularly updated and renewed at strategic intervals, including the need for the incorporation of critical new information as it becomes available. Experiences from our responses to new outbreaks or other, directly relevant developments, were also incorporated.With this model of work, it gave us the head-start when COVID 19 first landed on our shores [7,8].
The first COVID 19 case in Singapore was seen at SGH on 23rd January 2020. The daily count remained relatively low until mid-March when a sudden rise of COVID 19 cases amongst dormitory-dwelling migrant workers took the numbers to record highs. Restrictions were enforced, circuit breaker measures were instituted, gatherings were banned, and businesses and schools were closed. People worked from home and students got used to online learning. Today, the numbers have stabilized, there are negligible community spread and all dormitories have been cleared. As of 7 Sept 2020, there have been 57 044 COVID-19 positive cases reported in Singapore, with 27 deaths. That makes the death rate0.00047%. Many restrictions continue to be practiced: wearing masks everywhere, no gatherings of more than 5 persons and safe distancing measures. Our local scientists continue to work hard at producing the COVID-19 vaccine and predictions of the possible trajectories of the pandemic: whether it will be a prolonged epidemic with multiple waves or a pandemic becoming endemic?
In the meantime, new norms and new practices have become embedded in the population, businesses, systems, organizations, industries and schools. At our AMC, this was also the case. Work has begun on many fronts and the positive ripple effects are already becoming apparent. As we reset ourselves for the new normal, our AMC has identified 5 attributes/ domains to guide our paradigm in the face of a new world. These are known as the 5 Ps: People, Patients, Places (Infrastructure Development), Programmes and (Pandemic) Preparedness [6,9] (Figure 1).
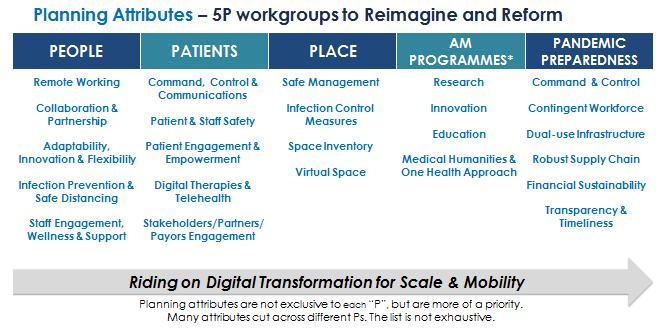
Figure 1: The 5 Ps Planning Attributes Post COVID 19 for the AMC.
The Paradigm Change and the New Norm
People
COVID 19 had an unprecedented toll on healthcare workers all over the world [2,10,11]. The people who ensure the AMC functions efficiently and effectively, are the staff…..every single one of the multi-disciplinary staff during COVID 19. It was critical to ensure their development continues. The building of their capacity and inculcating their capabilities, must be relevant and applicable in the current as well as the post-COVID 19 world. Training and continuing education is important and must be customized. It has to be linked to their ability to learn, unlearn and relearn. The ability to learn is a standard, but unlearning can be challenging. Some staff may hang on to old practices and are unable to let go of these. This is where mindset change and adaptation comes in. How do we get their buy-in? How do we prove the new method is better than the old? How do we combine the traditional with new technology? One good example would be the cutting down of face to face training. With that, medical officers, residents and nurses training sessions have gone virtual. We invested in electronic (E- learning) and online learning in a big way. Didactic and interactive sessions were delivered via Zoom, or other similar platforms [12,13]. Simulation in the sim-lab was converted to computer-based simulation [12]. We also had to ramp up the development of our Virtual and Augmented Reality (VR and AR) applications faster than expected. We very quickly sourced for funds to hasten the completion of our Innovation Arcade at our simulation centre (The SingHealth Duke NUS Institute of Medical Simulation), in preparation for the VR, AR, mixed reality (MR) and serious games applications. We applied for the Learning Technology Adoption Grant (LTAG), from SkillsFuture, Singapore and are working on 14 different serious gaming projects with appointed vendor companies [14]. SkillsFuture is a national movement providing Singaporeans with the opportunity to develop their fullest potential throughout life, regardless of their starting point. The skills, passion and contributions of every individual will drive Singapore’s next phase of development towards an advanced economy and inclusive society. These projects cut across various disciplines, whilst some are inter-disciplinary. All these projects have bearing on our patient care, workflow as well as staff training. Our staff are the subject matter experts in these applications and will champion their use for training and education.
To be able to embark on these projects and ride the latest bandwagon of digital transformation, we have to ensure our people are exposed to the latest developments. We created the awareness by telecasting webinars and virtual seminars on relevant themes. Training sessions are made readily available and accessible. These sessions are provided for all the relevant staff. Empowerment courses are also converted to virtual training format and the numbers of participants increased significantly during the COVID-19 pandemic, despite the heavy workload that we were facing. The focus on mastery of skills and knowledge is important. This, we feel, is a step in the right direction to be able to function in the VUCA (vulnerable, uncertain, complex and ambiguous) world, post COVID-19. Staff motivations must never be taken for granted [15]. That is why messaging and reinforcements must be conducted regularly. This can be through the AMC’s intranet, screen–savers on all computers, posters, email blasts and flyers. This customized faculty development concepts will ensure our future ready workforce is up-to-date, competent, resilient and relevant.
Support for all these relevant changes must come from the leadership and management. In fact they are the ones leading in the AMC’s thrust, mission and vision. Leaders who walk the ground, get involved and are aware of the issues will have a deeper understanding of any situation and this means any policies they craft, are likely to be more practical and responsive. Leaders have the ability to inculcate inclusivity. At our AMC, the Chief Executive Officer session with all the staff is termed as “The Family Meeting”. At the session during the COVID 19 pandemic, attendances increased, with many enthusiastic feedback and questions. Sharing the future directions and main thrusts, reassuring the staff, supporting and empowering them through positive attitude, care and concern can have strong impact on employees. The importance of collegiality and camaraderie across any hierarchy must never be under-estimated. This way the staffare encouraged to bring up constructive ideas and feedback, as this is the way to enhance and improve our performance at the AMC [7].
Being able to embark on all these exciting new developments and projects will not be relevant if our staff are not motivated and unwell. This is why during COVID 19, the AMC had invested and rolled out even more activities and resources related to staff psychological wellness, mindfulness and “Joy At Work” (JAW) initiatives. Mindfulness training during COVID 19 has helped the staff at the AMC in a variety of ways [3,7]. It helps to increase attention span and this was certainly useful with the longer hours at work in modular teams. It helped build and strengthen relationships between all levels of staff and across disciplines as well. This facilitated work processes such as when the Emergency Department (ED) staff made admissions; there were lower incidence of bed blocks. Discussions were collegial. The Infectious Diseases consultant on call took consultations readily and provided collaboratively discussions and advice with the ED staff on admissions to isolation wards, high dependency beds and intensive care units for infection-related diagnoses. The positive attitude demonstrated more gratitude, care and concern for each other. Peer support was enhanced. Wellness ambassadors were appointed and taglines such as “ Its OK to not be Ok” were publicized. Counselling was made available 24 hours a day to any staff who needed this or wanted to talk on any issues [7]. Mindfulness can also help in promoting the more conscious practice of Medicine. A happy and satisfied staff will deliver compassionate care and this is the gateway to patient satisfaction [16]. We cannot have our staff painstakingly creating processes from the vantage point of the patient and not see joy in their own work, come alive.
During the pandemic, there was an opportunity for institutions to review their various KPIs (key performance indicators) and manpower needs. With the new norms, some parameters may have to be altered. For example, due to the donning and doffing of PPE when managing certain groups of patients, more time will be required. This means the average time spent per patient will increase and thus, productivity will be altered as well. Allocation ratios of doctors and nurses in the different areas will also change. COVID 19 also provided an opportunity for the level of trust between individual employees and the AMC to be stepped up. The demonstration of care and concern for the safety of staff must come across clearly. This defines another important compact of the institution. Showcase of gratitude and appreciation for each other is important. With these happening at all levels, instead of post-traumatic stress manifestations, staff are now in the phase we term, “post traumatic growth and development”, since the COVID-19 pandemic started. This way the AMC continues to heighten our capabilities and capacity of our staff as they continue to thrive. In fact the pandemic brought out the best in them. Without the physically and psychologically healthy workforce, the delivery of excellent healthcare will be difficult [7].
Change is hard, challenging and difficult, but when people come together, we can accomplish the impossible. The future will see healthcare staff embracing more global learning, shared knowledge, best practices and the setting up of more communities of practice. This may lead to more standardization and less unscientific variations of care [17,18].
Patients
During COVID 19, there were changes encountered with the AMC’s patients profile and case mix. This was mostly due to the changes observed during the various phases, as the pandemic spanned out. As we move into a more stabilized state of the COVID-19 pandemic in Singapore, many of the changes that have taken place related to patient care will continue [19]. This includesa higher utilization of telehealth and teleconsultation. This can increase productivity and save time for the healthcare providers as well as the patients. In fact, where appropriate the family members can even join in. Of course, not all cases are suited for teleconsult, thus the more appropriate cases and diagnoses were selected: eg. follow up for chronic diseases and primary care type cases [20]. Video-consults and video calls were also used appropriately.The full potential of telehealthcan be summarized as follows:
- For on demand virtual urgent care. This can be for lower acuity emergency visits
- Virtual clinic type consultations: for primary care cases, chronic illnesses follow up or for specialist outpatient clinics consultations
- Virtual home care service. This can cover “virtual visitations” with communications over the computer or smart mobile devices.
- Remote monitoring is also possible when there is cooperation of the parties involved. Digital engagement tools can also be used for education of the public. This is also where telehealth can provide oversight to many aspects of care such as patient controlled analgesia for cancer patients
It will be more challenging to break bad news or manage complex complications virtually. Thus, some aspects of face to face care must still continue.
At SingHealth, an e-learning telehealth course was made available online and for all staff who complete the modules, CME (continuing medical education) points were awarded. Moving on, this has now become the basic fundamental course for Telehealth certification for staff using tele-consultation. This course covered the definition of telehealth and teleconsultation, detailsof the requirements, maintaining confidentiality during tele-consults and even charging mechanisms for primary care physicians utilizing this modality. With the wider use and greater numbers of practitioners subscribing to it, the cost will become more reasonable and thus the service can be offered at lower costs to patients [21].
At the frontline, patient screening evolved and workflow processes were updated. New areas were created to manage infectious patients in negative pressure environment. Senior physicians help reminded the residents and medical officers of the potential blind-spots for other diagnoses, in the midst of their focus in not wanting to miss out diagnosing COVID 19. Besides training and educating staff, patients also went through the ‘journey of change’. They were learning to use their mobile phones for video consults, testing their hands at various mobile applications the AMC had implemented. Some of these applications were derived from our regular hackathons, where new ideas were generated. There werealways staff on hand as well as IT (information technology) ambassadors to assist patients who were not tech-savvy to negotiate these new applications. They were assisted and their queries were sorted out and clarified, to help them leverage technology in this new age. This also aligns with the Singapore’s government initiatives to make the country a ‘smart nation’[22]. In fact during and post COVID 19, the majority of correspondences with patients eg. appointment dates and changes,were via mobile devices. SMSes (Short Message Service) will continue to be used for reminders. Traditional and manual resources were still made available for those who really are not able to cope with new technology.
Places
The post COVID-19 world of healthcare will never be the same as before. There is no going back to what we were used to. The infection control changes, potential risks from new and emerging infectious diseases and some of the technological developments we are all so used to now, will continue on this trajectory. However, the other healthcare trends such as the ageing population, more chronic illnesses and their related complications, higher incidence of cancers and thus immunosuppression, as well as the more complex presentations in our patients will also continue.
The AMC’s facilities and work processes will continue to evolve, as it has since SARS. The negative pressure facilities in the ED continues to be added. With the new ED under construction, forward planning has been done to ensure sufficient space and facilities, eg. separate ports can be converted to negative pressure areas as deemed necessary by demand. These flexibilities will help in handling upsurge in future outbreaks or pandemics management. Whilst planning all these, the patient flow must continue to remain as seamless as possible. The main objectives of the work flow and processes in the ED must ensure that:
- The ED must not allow over-crowding. Innovative distancing measures will have to be implemented
- The ED must not become a reservoir of nosocomial infections
- The ED work flow must ensure safety of the patients as well as the staff working there and
- The timing to manage patients, especially acutely ill and critical patients must not be compromised.
The Infectious Diseases wards and facilities too underwent upgrading during COVID 19. The number of isolation wards and roomshave increased up to some 30 % of our total bed capacity. At the peak of the COVID 19 pandemic, a 5 level multi-storey carpark near the AMC was closed to the public and converted into a consultation and management area for foreign workers from the dormitories. This was termed as our FSA (Fever Screening Area). The ample space, across 5 levels enabled us to use the areas for consultation ( cubicles were constructed), waiting areas for swab results and waiting areas for COVID + patients awaiting admission to negative pressure isolation rooms in the main hospital building. Staffwere seconded to work in this area, with full PPE (personal protective equipment). Before new work areas such as these are opened, we organized insitu simulation to study the workflow processesto realize latent threats. At the same time we did a failure mode effect analyses, to establish best practices.
One of the large open carparks on the AMC campus was cleared and 50 container wards were built quickly. These were all negative pressure rooms for high risk patients. This certainly provided additional bed space for the institution. This was one of our achievements during COVID 19; completion of the building within 30 days. Besides these initiatives, we also have the negative pressure isolation tent available in case it needed to be deployed into any particular area of work, quickly [23] (Figure 2).

Figure 2: The Negative Pressure Isolation Tent which can be deployed where needed within minutes.

Figure 3: SG SAFE Shield booth for healthcare workers to stand in when performing naso- and oro-pharyngeal swabs for COVID-19.
At the ED naso- and oro-pharyngeal swabs were not done inside the department but outside, in a booth as seen in Fig. 3.This represented a new innovation by the Department of Anesthesiology in the AMC [24] (Figure 3). Patients coming into the ED and hospital clinics have to be segregated and spaced accordingly. Everyone was masked up. This was compulsory. The patients were divided into ‘clean’ cases (no fever, URTI, LRTI symptoms , high risk contact with local clusters and low epidemiological risks, etc) and ARI ( acute respiratory illness) cases, and managed in different areas. This means the patients, radiology services and staff in these different areas did not mix and interact. To be able to do this, the triage upfront has to be spot-on and stringent.
Moving on, there will be a new paradigm for infrastructure whereby the distribution of healthcare settings and healthcare providers will evolve. This needs forward planning and must be unified and coordinated. As we see the emergence of new growth opportunities and diversification, there will be faster construction, customized designs with greater agility and potential for repurposing of facilities, equipment and furniture. The future will also see creation of multi-faceted and multi-functional resources, with new hubs of excellence. Capacity for intensive care will have to be expanded. One very progressive option to consider would be virtual ICUs (Intensive Care Units), with the monitoring done from the homes of patients. In Singapore, post COVID-19, we have opened a large scale Urgent Care Centre to provide intermediary care, between that provided by primary care and the care at EDs [25]. Home based care will also see an expansion post COVID 19. This would be linked to higher utilization of phone-based diagnostics and virtual patients engagements. Auxiliary services too may now see more decentralization to enhance accessibility and less crowding at one location. In the AMC, the infrastructure that supports the work of process design and improvement will help ensure the staff continue to be empowered and motivated in an environment where they feel safe at work.
Syndromic surveillance capabilities continue to be enhanced with our computerized and electronic systems. Technology-driven bio-detection will be used more frequently. Notification of infectious diseases and other reportable diseases too are done online and can be tracked readily. Whilst adopting the Internet of Things (IoT), cybersecurity is always at the top of our minds. The AMC has gone through internet separation since 2018 and all the staff have been briefed on this. Everyone was required to take a cybersecurity vigilance course with online assessments. Departments had to procure separate internet enabled computers and only special encrypted, registered external drives were allowed, with close monitoring.
In 2007, JCI came up with the Guiding Principles for the Development of the Hospital of the Future [26]. In this paper, the pointers put forth are relevant to this era of practice. The recommendation for standardized flexibility, which will reduce complexity in the event of increased surge capacity is extremely applicable here, as we have seen during the pandemic. The standardization of patient rooms and room designs had been suggested for optimizing human- system interaction. The use of “loose-fit design” is to design with larger spaces in order to arrange for future adjustments. This is the same with convertible flexibility, whereby a space can be converted to another use when it is needed. In order to offer flexibility in design, utility and communications infrastructure, the master planning strategies must incorporate these concepts from the beginning, so these facilities will be robust enough to accommodate expansion and upgrades. This must align with what is called the ‘plug and play’ infrastructure whereby the horizontal and vertical circulation infrastructure remains in service despite certain departments or wings undergoing upgrades, renovations or are being removed [26].
The interaction and integration between People (staff) and the Physical (infrastructure and environment) is critical. This is something that has to be mainstreamed from the planning stages, but when necessary, customization and improvisation may need to be done.
Preparedness
The importance of preparedness for the 21st century cannot be over-emphasized. Investment into infection control measures, and quality care will drive this [27]. During this pandemic, healthcare systems and countries with lack of readiness and under-par responses, have had to pay a high price. Moreover the preparedness is not just for infectious diseases outbreaks but also for large scale trauma, natural and man-made disasters and even cyber-threats. PPE will become a norm, especially with the frontline disciplines. Screening at the frontline too will continue to be critical. Wearing the appropriate masks will become the minimum standard, post COVID-19. Besides these practices at work, healthcare workers must comply with the distancing guidelines when they are out in the community as well. They set the example for others. By now, every employee at the AMC is familiar with compulsory twice a day temperature log in, use of the contact tracing application and safe distancing measures.
We cannot let down our guardeven as COVID 19 cases start to stabilize downwards. In fact it is necessary to remain vigilant, with the potential for subsequent waves as well as new and evolving infectious diseases today [19].
The healthcare communities in Singapore will continue to work in partnership as this is crucial in sharing best practices, surveillance observations and closing the gaps with local epidemiology and public health. It is important to remain nimble and agile in the current and future climate. Further collaborative studies, data sharing, including the use of big data, will shed more light and set the directions for the future.
The staff of the AMC will drive our preparedness through their teamwork (multidisciplinary collaboration), supportive leadership who are role models, deep understanding of process flow, condusive environmental changes and the relevant, up to date tools. These proper teaming can influence the end metric and goals.
Programmes
Besides the introduction of relevant, new programs, many of the ones started during the COVID 19 pandemic will continue post COVID-19 as well. There will be ‘blending and braiding’ of existing programs with new ones to improve safety and care delivery.(28)These would include telemedicine and telehealth courses, virtual teaching platforms, the use of VR, AR and MR (mixed reality) to supplement teaching and training programs [20,21]. E- learning and online platforms will continue to be enhanced further. Even in organizing local and international conferences, virtual platforms will be added, besides the usual face to face sessions. For many of the conferences which are organized by the AMC departments, hybrid models will be offered, where some components will be offered face to face whilst others more suitable ones will be delivered virtually. Keeping in touch with the community of practice, both locally as well as globally is also important. Currently, virtual connections and teleconferencing keep us connected to share information and best practices across the globe.
Programs such as bulk purchasing training and courses will have value across healthcare clusters. It will help procurement of shared inventories and preparation for stock-piling of certain products and equipment ( eg. masks, PPE). This can be more cost efficient for a small country like Singapore. Simulation will become very helpful in planning the management of more uncertainties, balancing needs against resources. Simulation-based training will continue in smaller groups and is useful in testing workflow, latent threats and can also be applied as insitu simulation. Coupling insitu simulation with failure mode effect analysis can also have value [28].
During the pandemic, staff of the AMC from inpatient departments were seconded to the frontline and busier departments to assist with the work. The departments would include the ED, ICU, ID wards, isolation wards and screening areas. These staff may not be very familiar with the workflow and were given a quick briefing and introduction. Cross-training would be a very useful initiative that can help prepare staff for such secondments. Cross-training can be a strategy to help the staff acquire skills and capabilities of working in areas other than their own discipline. This way they can diversify their skill sets, be more versatile and help to serve where they are needed in crises. Cross-training can ‘energize and strengthen’ these staff, improve teamwork and inter-professionalism, as they learn and understand more of what their colleagues do in the various departments. The level of respect across disciplines can also be enhanced. [29,30].
The AMC has always been very supportive of staff’s innovation and research projects. During the pandemic, one of the grant calls was termed “COVID 19 Innovation Grant Call”. The objectives clearly specify the focus on innovative ideas in the‘new norm’:
- To increase operational efficiency and productivity for work processes affected by COVID 19
- To improve quality of care and patient safety amidst the ‘new norm’
- To ensure the safety of healthcare professionals during the resumption of healthcare services for non-COVID 19 patients and
- To encompass longer term innovations to support strategic goals and operations in the ‘new norm’
The AMC organizers will also assist to match interested parties with internal or external partners as appropriate, e.g. Technological experts, engineers. This really demonstrates the emphasis and inclusivity of all staff in contributing their ideas towards making patient care and work processes as well as system flow better.
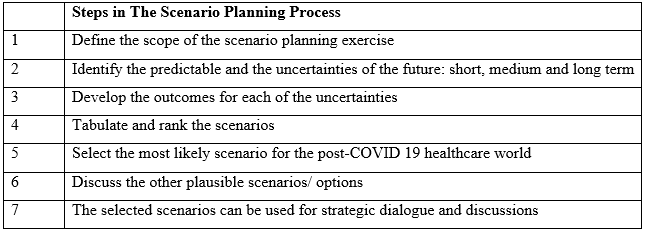
Another springboard for strategic change innovation and implementation is scenario planning, which can generate new initiatives. The staff will put forth their ideas and suggestions, colored by their life experiences, including those derived during the COVID-19 pandemic. Many of these will commence with brainstorming, which starts with critical questions, that can help generate insights into the shared future and what we collectively want, post COVID-19. (Table 1) To be able to continue with these newer modalities, some unlearning and relearning will be required. Training will help bridge the gaps. Acquisition of new knowledge and skills will continue to be robust. To face the disruption and digital transformation, we must all be prepared, both psychologically and physically.
Table 1: Using Scenario Planning for Discussion the Post-COVID 19 situation.
Conclusion
The AMC is committed to leading every day, continually learning and adjusting creatively to change. The energy that drives it is the human desire of all the staff. The life and work at the AMC will have undulations and waves. That is the norm. However, there may be certain critical points whereby the journey can reach a breakpoint. This is where the behavior of the system must change radically. This is the change we will see post-COVID19. This is the change we have been building up to and preparing for. How we functioned during COVID 19 and the decisions we made, will spark off these high-value added changes. How we handled the ‘chaos’ at the start of the pandemic, strived to find the patterns of alignment, will help us reimagine and reinvent the future norms. Through our multi-dimensional lenses, we must look forward, but not forget to look back to the time of the pandemic, as well. The business as usual, post COVID 19, will be the new norm.
References:
- Delrio C, Malani PN. COVID 19: new insights on a rapidly changing epidemic. JAMA February, 2020. Available at : https://doi.org/10.1001/jama.2020.3072.
- Heymann DL, Shindo N. COVID 19: What is next for public health? The Lancet 2020;395(10224):542-545. Available at: https://doi.org/10.1016/S0140-6736(20)30374-3.
- Chaves S. Leng b, Koyfman A, Liang SY. COVID 19: A primer for emergency physicians. Am J of Emerg Med 2020. Available at :https://doi.org/10.1016/j.ajem.2020.03.036.
- About the SingHealth Duke NUS Academic Medical Centre. Available at : www.singhealthdukenus.com.sg/about-us (last accessed on 7 Sept 2020).
- Academic Medical Centre Accreditation. Joint Commission International. Available at:https://www.jointcommissioninternational.org/accreditation/accreditationprograms/academic-medical-center/ (last accessed on 7 Sept 2020).
- Fatimah Lateef. SARS changes the ED paradigm. Am J Emerg Med 2004;22(6): 483-487.
- Fatimah Lateef. Face to face with COVID 19: Maintaining motivation, psychological safety and wellness. Special Article. Journal of Emergency, Trauma and Shock 2020;13:116-123.
- Fatimah Lateef. Through the ethical lenses: There is more than meets the eye with COVID 19. Archives of Emergency Medicine and Intensive Care. 2020;3(1): 6-16.
- SingHealth: About Us. Available at: https://www.singhealth.com.sg/about-Singhealth/corporate-profile/about-us (last accessed on 7 Sept 2020).
- Owen WF Jr, Carmona R, Pomeroy C. Failing another national stress test on health disparities. JAMA 2020; DOI: 10.1001/jama.2020.6547.
- Gaeta C, Brennessel R. COVID 19: Emergency medicine physicians empowered to shape perspectives on this public health crisis. Cureus 2020;12(4):e7504. DOI: 10.7759/cureus.7507.
- Lateef F. Computer-based simulation and online teaching netiquette in the time of COVID 19. Review Article. EC Emergency Medicine and Critical Care 2020;4.8.
- Brazil V. Translational simulation: not where but why: A functional view of insitu simulation. Adv Simulation 2017;2:12
- About SkillsFuture Singapore. Available at : https://www.Skillsfuture.sg/AboutSkillsfuture(last accessed on 7 Sept 2020).
- What VUCA really means for you? Crisis management. Harvard Business Review. Available at : https://www.hbr.org/2014/01/what-vuca-really-means-for-you(last accessed on 7 Sept 2020).
- Fatimah Lateef. The Art of Conscious Practice: Mastering Medicine. Education in Medicine Journal 2016;8(2):53-57.
- Nilsen P, SchildmeijerK, Ericsson C, Seing I, Birken S. Implementation of changes in healthcare in Sweden: a qualitative study of professionals’ change response. Implementation Science 2019;14:51. Available at : https://doi.org/10.1186/s13012-019-0902-6.
- Grama b, Todericiu R. Change: Resistance to change and organization cynicism. Stud Bus Econ 2016;11(3):47-54.
- MOH Situation Report: COVID 19. Available at : https://www.moh.gov.sg/covid-19/situation-report(last accessed on 7 Sept 2020).
- National Telemedicine Guidelines. Ministry of Health. Available at : https://www.moh.gov.sg/resources-statistics/guidelines/national-telemedicine-guidelines(last accessed on 7 Sept 2020).
- Licensing Experimentation and Adaptation Program (LEAP). A MOH Regulatory Sandbox. Ministry of Health, Singapore. Available at : https://www.moh.gov.sg/home/our-healthcare-system/licensing-experimentation-and-adaptation-programme-(leap)---a-moh-regulatory-sandbox(last accessed on 7 Sept 2020).
- Smart Nation, Singapore. Transforming Singapore through Technology. Available at : www.smartnation.gov.sg(last accessed on 7 Sept 2020).
- Fatimah Lateef, Chia SHS, Teo HBA, Tan TC. The evolving demand for negative pressure isolation facilities during COVID 19: Trial of the negative pressure isolation tent. Biomedical Research and Clin Review 2020;1(2). DOI: 10.31579/brcr.2020/011.
- SGH and Biofactory develop SG SAFE and SG SHIELD to keep healthcare workers safe during COVID-19 swab tests. Available at: https://www.singhealth.com.sg/news/tomorrows-medicine/sgh-and-biofactory-develop-sg-safe-and-sg-shield-to-keep-healthcare-workers-safe-during-covid-19-swab-tests(last accessed on 7 Sept 2020).
- Weinick RM, Burns RM, Mehrotra A. many ED visits could be managed at urgent care centres and retail clinics. Health Aff. 2010;29(9):1630-1636.
- Healthcare at the crossroads: Guiding Principles for the development of the hospital of the future. Available at: https://www.jointcommission.org/-/media/deprecated-unorganized/imported-assets/tjc/system-folders/topics-library/hosptal_futurepdf.pdf?db=web&hash=BEDD225214DB9A1BB436C69A2E0C8123 (last accessed on 7 Sept 2020).
- Berwick DM, Shine K. Enhancing the private sector preparedness for 21st century health threats: Principles from a National Acadmies Initiative. JAMA 2020;323(12):1133-1134.
- Pelletier C, Kneebone R. Playful simulation rather than servicing cue: medical simulation on cultural practice. Games Culture 2016;11:365-389.
- Hedges AR, Johnson HJ, Kobulinsky LK, Estock JL, Eibling D, Seybert AL. Effect of cross-training on medical teams’ teamwork and collaboration: use of simulation. Pharmacy 2019;7(13). doi: 10.3390/pharmacy7010013.
- Cannon-Bowers JA, Salas E, Blickensderfer E, Bowers CA. The impact of cross-training and workload on team functioning. A replication and extension of initial findings. Hum Factors. 1998;40:92-101.

