Serious Antimalaria Resistance, Genetic Markers of Kelch 13, Plasmepsine 2 Cnv Associated with Dihydroartemisinine - Piperaquine Resistance in Plasmodium Falciparum Population in Malaria Endemic Zone Of Dak Lak Province, 2019-2020
Huynh Hong Qu2*, Chau Van K1, Nguyen Thanh TN2 and Nguyen DH1
1Institute of Malariology, Parasitology, and Entomology IMPE) Quy Nhơn,Vietnam
2Oxford University Clinical Research Unit, Vietnam
Received Date: 24/09/2020; Published Date: 28/10/2020
*Corresponding author: Huynh Hong Quang, Oxford University Clinical Research Unit, Institute of Malariology, Parasitology, and Entomology. Quy Nhon, MoH Vietnam
Abstract
Backgrounds: Dihydroartemisinin-piperaquine is a current frontline drug recommended in global by WHO for the treatment of Plasmodium falciparum malaria (WHO, 2015), but is now failing in Vietnam provinces where border Cambodia, and has emerged and spread. The purpose of this study was to evaluate efficacy and molecular markers of dihydroartemisinin-piperaquine failures in Dak Lal province.
Methods: A study design of non-randomized controlled study design for the 42 day-course follow-up in vivo test, and the molecular markers analysis.
Findings: The data showed that adequate clinical and parasitological response was sharply declined of 12,1%, late clinical failure of 51.5%, late parasitological failure of 36.4%, proportion of positive parasitemia at D3 is 37%, slope half-life of 5.36 hrs, and progressive parasite clearance PC50, PC75, PC 90, PC95, and PC99 were 13.24; 19.29; 25.69; 29.97 and 39.15 hrs, respectively. Molecular markers of C580Y Kelch mutation observed 100% (50/50) in the patients, increased of Plasmepsine 2 CNV of 72% (36/50), and both K13 and Plasmepsine 2 of 72% (36/50).
Conclusions: The DHA-PPQ efficacy severely decreased of 12.1%, overall treatment failure of 87.9% with the prominent C580Y mutant plus increased Plasmepsine 2 copy number variation in delayed asexual P. falciparum parasite clearance. These obvious data need to urgently change antimalarial policy in DHA-PPQ resistance zones.
Keywords: Plasmodium Falciparum; K13 Propeller; Plasmepsine 2 Copy Number Variation (CNV)
Introduction
Artemisinin-resistant Plasmodium falciparum threatens to the malaria elimination process in the Greater Mekong Subregion (GMS) [18]. K13-propeller mutation and the increased copy number variations (CNVs) in Plasmepsine 2 were considered as markers associated with artemisinin-resistance and piperaquine-resistance, respectively, and had a role in the extended period of asexual development [1], which consequently caused delayed parasite clearance after treatment with ACTs [2,3]. These markers were detected in several countries in GMS. Binh Phuoc, and many provinces in Central Highlands already have reduced sensitivity, treatment failure and resistance to dihydroarteminsinin-piperaquin (DHA-PPQ), especially in Dak Nong, Quang Nam, Khanh Hoa and Gia Lai. Krong Nang district in Dak Lak province is one of the hot spots in terms of malaria cases in Central Highlands, and border Dak Nong, Khanh Hoa, Gia Lai, Phu Yen, then, are there in vivo resistance to DHA-PPQ and resistance markers in these provinces? Therefore, this study was conducted to evaluate DHA-PPQ efficacy in P. falciparum treatment and molecular markers (K13-propeller mutation and Plasmepsine 2) in two P. falciparum populations.
Subjects and Methods
Study Sites and Duration
+ Ea Dak, Dlie Ya and Ea Puk communes in Krong Nang district, Dak Lak province.
+ From February 2019 to February 2020.
Study Design
+ Non-randomized controlled study design for the 42 day-course follow-up according to the WHO template protocol for therapeutic efficacy studies (TES) (WHO, 2019).
+ Molecular markers analysis at Molecular biology unit of Pasteur Institute, Cambodia.
Study Population
+ Inclusion criteria: patients with age between 3 and 70 years, mono-infection with P. falciparum, parasitaemia between 1000 and 100000/µl of asexual forms, presence of tympanic temperature ≥ 37,5oC, no prior antimalarial drugs, informed consent from patient or from a parent or guardian in the case of children.
+ Exclusion criteria: patients with age under 3 years or more than 70 years, pregnancy or breastfeeding, patients with mental health disorders, epilepsy, severe vomiting or diarrhea, or inability to absorb oral medications, complicated malaria or co-infected diseases, mixed-infection with another Plasmodium species, patients with prior antimalarial drugs, women in child-bearing age have to take pregnancy test.
Study Sample Size
The proportion of DHA-PPQ treatment failure in a previous study in Binh Phuoc was 15%. Therefore, 15% has been chosen as the estimated therapeutic failure rate of the drug, with a confidence level of 95% and with a precision around the estimate of 10%. The estimated minimum sample size was n = 50.
Study Assessment
All patients who meet the basic enrolment criteria will be evaluated for clinical information, malaria parasite density, parasite clearance measurement, molecular biological analysis, K13 mutation (artemisinin-resistance) identification, increased CNV in Plasmepsine 2 (piperaquine-resistance) detection by RT-PCR with Synb green staining.
Statistical Analysis
+ In vivo software (WHO 2015, version 2017) will be used for data management and analysis.
+ The proportion of K13-profeller and Plasmepsine 2 mutation will be calculated per total analyzed sample.
Results
Baselines of study patient’s characteristics
Table 1: Characteristics of study population.
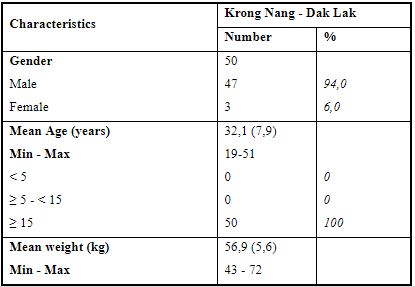
In all 50 patients who were mono-infected with P. falciparum in Krong Nang, Dak Lak, there was a male predominance with 47 cases (94%), while there were only 3 female patients (6%). The mean age was 32.1 years and all patients were more than 15 years old (100%). The mean weight was 56.9 kg.
Table 2: Clinical manifestations, spleen examination and P. falciparum parasite density.
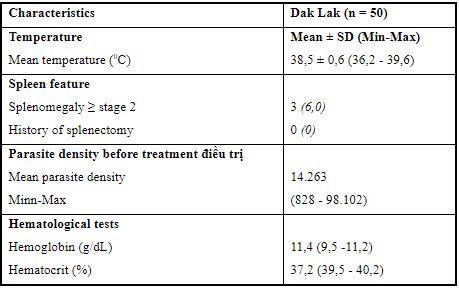
The mean temperature of all patients was 38.5 ± 0.6oC, spleen examination detected only 3 patients with splenomegaly greater or at stage 2 (%), there was no patient with a history of splenectomy. The mean parasite density at D0 (before treatment) was 14.263/µl. The mean haemoglobin (Hb) was 11.4 g/dL (9.5 – 11.2) and mean haematocrit (Hct) was 37.2% (39.5-40.2), these two figures were in normal range.
The efficacy of DHA-PPQ in treatment of P. falciparum
Table 3: The efficacy of treatment of P. falciparum at study sites.
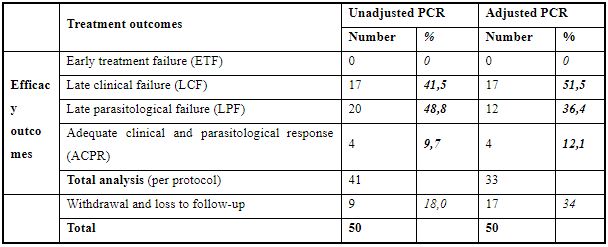
In 50 patients who were followed-up to 42 days, the number of Adequate clinical and parasitological response (ACPR) to DHA-PPQ after PCR was 4 (12.1%), 17 patients (51.5%) had late clinical failure (LTF) and 12 patients (36.4%) had late parasitological failure (LPF), there was no late treatment failure. The number of withdrawing and loss to follow-up patients was 17 (34%)
Table 4: Treatment efficacy and asexual parasite detection after treatment with DHA-PPQ.
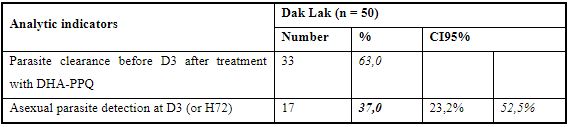
The proportion of asexual parasite detection at D3 after treatment was 37%.
Table 5: Indicators of P. falciparum parasite clearance in follow-up.
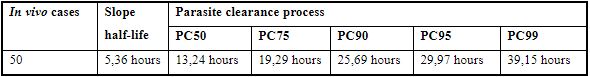
Detailed analysis indicated that slope half-life was 5.36 hours. The 50%-clearance of parasite (PC50) was 13.24 hours. PC75, PC90, PC 95 and PC 99 were 19.29 hours, 25.69 hours, 29.97 hours and 39.15 hours, respectively.
Identification of K13 mutation and increased Plasmepsine 2 CNV
Table 6: Markers analysis of K13 propeller and plasmepsine 2 CNV.
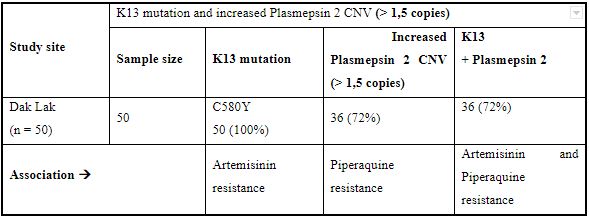
Molecular analysis of P. falciparum in 50 patients who attended to the study in Krong Nang district, Dak Lak province, showed that 50 cases (100%) had C580Y mutation, associated with resistance to artemisinine;
The number of increased Plasmepsine 2 CNV (1,5 copies) in P. falciparum population was 36 (72%), it was considered as a marker of resistance to piperaquin phosphate and the number of cases which had both those two makers was 36 (72%), which means resistance to two molecules in DHA-PPQ.
Table 7: Comparison between mutation type and WHO K13 mutation classification.
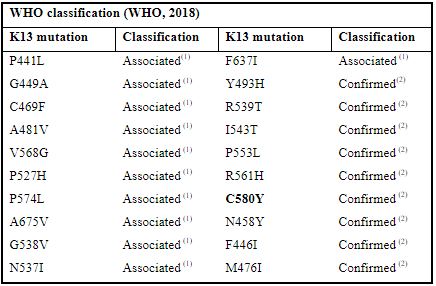
(1)Associated is a mutation classification which associate to P. falciparum resistance
(2)Confirmed is a mutation classification which confirm P. falciparum resistance
Discussion
Baseline data of clinico-laboratory profile of P. falciparum malaria patients
In the total of 50 cases of uncomplicated falciparum malaria, male gender is 47 cases (94%) and female 3 casses (6%). Average age of 32.1 and all of them are adult, average weight of 56.9kg. Average body temperature of 38,5 ± 0.60C, and 6.0% (3/50) of cases have spleen enlarge. Asexual mean geometric malaria parasite of P. falciparum at day D0 is 14,263/μl, and haematological parameters in study group is in normal range, especially is haemoglobine of 11.4 g/dL (9,5-11,2) and haematocrite percentage of 37.12% (39,5-40,2), and these data are similar to other therapeutic efficacy studies in Dak Nong, Quang Tri provinces (Vietnam), and Cambodia, and Myanmar sentinel sites.
Efficacy of DHA-PPQ in the treatment for uncomplicated falciparum malaria
Total of 41/50 cases of P. falciparum were followed-up to day 42 showed that PCR adjusted-adequate clinical and parasitological response (ACPR) is 12.1% (4/41), late clinical failure (LCF) of 51.5% (17/41), late parasitological failure (LPF) of 36.4% (12/41), and no early treatment failure (ETF). After the DHA-PPQ 3-day course dose treatment, the day D3 positive of asexual parasite of 37.0% (CI95%: 23,2-52,5). This data evoked that DHA-PPQ efficacy is seriously reducing, and cure rate only 12.1%, total treatment failure of 87.9%. Compared of ACPR to other border-line in Dak Nong province (border Cambodia) and Quang Tri province (border Lao PCR) were 88.1% and 100%, respectively. In particular, data in Dak Nong with LCF of 9.5%, LPF of 2.4% (n=46), and D3 positive was 41.7%. According to WHO terminology that proportion of D3 > 10% as indirect marker of partial resistance of artemisinin and its derivatives. Hence, out of TES data and positive D3 > 10%, WHO-validated molecular markers analysis will strongly confirm the artemisinine and partner drugs status. On the other hand, slope half-life is 5.36, and detailted parasite clearance time of parasite biomass gradually PC50, PC75, PC90, PC95, and PC99 are 13.24; 19.2; 25.69; 29.97, and 39.15, respectively.
These data are similar of other confirmed TES in malaria endemic areas in Central Highlands and Binh Phuoc province of Vietnam [13],[14]. Proportion of ACPR are from 94.7-100% and D3 positive of P. falciparum sexual form were still high, such as in Binh Phuoc, this parameter increasing step by step, year by year, from 15% to 22%, 30%, 36%, 36.8% in 2010-2015; in Quang Nam with D3 proportion of 29,2%, Khanh Hoa of 17.4%, Gia Lai was from 11% to 23%; 26.4% in 2010-2014. Compared to other sentinel sites of Greater Mekong Subregion countries, this proportion is little lower, especially in Pailin, Rattanakiri, Battambang of Cambodia have ACPR of 90-95% with D3 positive in 2008-2012 period are 26%, 33%, 45%, 54%, respectively or this proportion is higher than Jingyang’s D3 positive in China (D3 of 14%), or in Champassack of Lao PDR is 22% in 2012, or in the Kawthaung, Mon of Myanmar is from 14% up to 19%, 23% (2011-2013), or in the Tak, Maehongson, Kanchanaburi of Thailand [15],[18] with D3 positive is from 9% to 14%, 17%, 25% and 48% in 2009-2014. All these results showed that not only DHA-PPQ resistance is in-country spreading out, but also occurred in GMS countries.
Molecular markers of Kelch13 and Plasmepsine 2 copy number variation
Analysis of P. falciparum isolates by molecular sequencing of K13 propeller mutants (for dihydroartemisinin-DHA resistance) and Plasmepsine 2 CNV (for pieraquine-PPQ resistance), data showed that all of 50 (100%) isolates have C580Y genotype involved to artemisinine resistance, and increased Plasmepsine 2 (>1,5 copy) on P. falciparum population is 72% (36 isolates) as PPQ resistance. The number of samples have K13 plus Plasmepsine 2 markers is 72%.
Conclusions
1. Efficacy of DHA-PPQ in the treatment for uncomplicated P. falciparum with ACPR of 12.1%, LCF of 51.5% and LPF of 36.4%. The positive asexual parasite on D3 is 37.0%;
2. Type of K13 mutant of C580Y is 100% in all isolates and Plasmepsin 2 CNV is 72%, especially in both resistant markers in P. falciparum population is 72%. Both these data showed that the DHA-PPQ efficacy was reduced seriously and need ot change antimalarial drug policyin this areas by new ACTs.
References:
- Nguyen Thi Lien Hanh, Huynh Hong Quang. Study of K13 mutation and delayed parasite clearance of Plasmodium falciparum post-treatment in several Central Highlands provinces (2014-2016). Journal for malaria and parasitic disease control. 2017;96:79-85. (in Vietnamese language).
- Bui Quang Phuc, Huynh Hong Quang, Tran Thanh Duong et al.,. Efficacy of dihydroartemisinin-piperaquin phosphate in the treatment for uncomplicated P. falciparum. Journal for malaria and parasitic disease control. 2015:49-57 (in Vietnamese language).
- Huynh Hong Quang, Nguyen Van Chuong . Resistant phenomenon related in delayed parasite clearance of P. falciparum post-treatment of dihydroartemisinin-piperaquine in malaria endemic areas border Cambodia. Medicine in Ho Chi Minh city. 2014;18(6):247-252 (in Vietnamese language).
- Ta Thi Tinh, Bui Quang Phuc, Huynh Hong Quang et al., Efficacy of several of artemisinine-based drugs (ACTs) in the treatment for Plasmodium falciparum malaria in malaria endemic areas (2005-2012). Journal for malaria and parasitic disease control. 2013;6:90-96.
- Nguyen Thi Minh Trinh, Huynh Hong Quang, Tran Binh Trong. Determination of mutation on Kelch (K13) protein of Plasmodium falciparum and artemisinine resistance in Gia Lai and Ninh Thuan. Journal for malaria and parasitic disease control. 2017;96:228-235.
- Ariey F, Witkowski B, Amaratunga C, Beghain J et al., (2014). A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature. 2014;505 (7481):50-55.
- Ashley EA, Dhorda M, Fairhurst RM, Amaratunga C et al., Tracking resistance to artemisinin. Spread of artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2014;371(5):411-423.
- Cho Naing, Joon Wah Maka, Kyan Aungb et al., Efficacy and safety of dihydroartemisinin-piperaquin for treatment of uncomplicated Plasmodium falciparum malaria in endemic countries: Meta-analysis of randomised controlled studies. Royal Society of Trop. Med. and Hyg. 2013;107(2):65-73.
- Melissa D. Conrad, Victor Bigira, James Kapisi et al., Polymorphisms in K13 and Falcipain-2 associated with artemisinin resistance are not prevalent in Plasmodium falciparum isolated from Ugandan children. PLoS One. 2014;9(8):1-6.
- Thuy Nhien Nguyen, Tuyen Kim Nguyen, Tong Thanh Nguyen, Thanh Viet Ngo, Quang Hong Huynh, Maciej Boni, et al,. Kelch protein gene (K13) mutation in Plasmodium falciparum population in three malaria hot spots of Vietnam. American Society of Tropical medicine and Hygiene. 2016;95(5):192.
- Nguyen Thuy-Nhien, Nguyen Kim Tuyen, Nguyen Thanh Tong et al., K¬13 propeller mutations in Plasmodium falciparum populations in regions of malaria endemicity in Vietnam from 2009 to 2016. Antimicrob Agents Chemother 2017;61:01578-16.
- Bui Quang Phuc, Huynh Hong Quang, Tran Thanh Duong et al., Efficacy and safety of oral artesunate and dihydroartemisinin-piperaquin for the treatment of uncomplicated Plasmodium falciparum malaria in Binh Thuan, Ninh Thuan, Daklak and Gia Lai provinces, Vietnam 2011-2012. Journal for malaria and parasitic disease control. 2013;5:84-89.
- Quang H. Huynh et al., Efficacy of dihydroartemisin-piperaquin and chloroquin in the treatment of uncomplicated Plasmodium falciparu and Plasmodium vivax malaria in Vietnam. American Society of Tropical medicine and Hygiene. 2016;95(5):272.
- Huynh Hong Quang, Nguyen Thi Lien Hanh, Nguyen Thi Minh Trinh. Artemisinins resistance molecular marker Kelch 13 in falciparum malaria in two sentinel sites of Central Highlands of Vietnam. Vietnam Journal of Preventive Medicine. 2017;27(4):68-78.
- Rie Isozumi HU, Isao Kimata, Yoshio Ichinose JL et al., Novel mutations in K13 propeller gene of artermisin-resistant P. falciparum. Emerging infectious diseases. 2015;21(3):490-492.
- Ngo Viet Thanh, Nguyen Thanh Thuy Nhien, Nguyen Thi Kim Tuyen et al., Rapid decline in the susceptibility of Plasmodium falciparum to dihydroartemisinin-piperaquine in the South of Vietnam. Malar J 2017;16:27.
- WHO. Methods for surveillance of antimalarial drug efficacy. 2009.
- WHO. Status report on artemisinin and ACTs efficacy, August 2018.

