Pathology Terminology Dilemmas in Gynaecology – To Act Upon or Treat as Normal?
Ying Yiing L1, Sahathevan S2 and Avni B3*
1Tunbridge Wells Hospital, Maidstone & Tunbridge Wells NHS Trust, UK
2Princess Royal University Hospital, King’s College Hospital NHS Foundation Trust, UK
3East Surrey Hospital, Surrey and Sussex health care NHS Trust, Redhill, UK
Received Date: 17/08/2020; Published Date: 04/09/2020
*Corresponding author: Sahathevan Sathiyathasan, East Surrey Hospital, Surrey and Sussex health care NHS Trust, Redhill, UK. E-mail: sathya@doctors.org.uk
Introduction
We often come across terminology in pathology reports which makes us think whether to act on the report or to treat as normal. In this article we have tried to consolidate a few of the histopathological diagnosis. The list is not exhaustive and we have tried to focus on the frequently occurring non common terminologies.
Meaning of Common Terms
Hyperplasia- Proliferation of Cell
Metaplasia- Conversion in cell type
Atypia- Structural abnormality in cells
Dysplasia- Change in cell
Neoplasia- Abnormal proliferation
Pleomorphism- Variability in the size, Shape and Staining of Cells and/or their nuclei.
Vulva-Pagets Disease of Vulva
James Paget was the first to describe Paget disease (PD) in 1874, while extramammary Paget disease (EMPD) was first described by Crocker in 1888 [1]. The condition consists of an intraepithelial adenocarcinoma. In general, EMPD lesions are found in areas such as the vulva, anus, perianal region, and axillae in which the density of apocrine glands is high. In women, the most common site of EMPD is the vulva; however, EMPD is responsible for less than 1% of all vulvar neoplasms [2]. Diagnosis of EMPD usually occurs between 50 and 80 years of age, with the disease being more common in Caucasian women [3]. The most common clinical symptom is pruritus. The lesion may be erythematous or eczematous, with islands of hyperkeratosis [4]. Surgical resection with wide margins is considered the standard treatment; however, successful surgical excision of the disease is a challenge and recurrences are com- mon. Alternative treatments such as photodynamic therapy, laser therapy, radiotherapy, topical treatments such as 5% imiquimod cream, or even chemotherapy have been the subjects of debate and it is important to evaluate the available evidence [5].
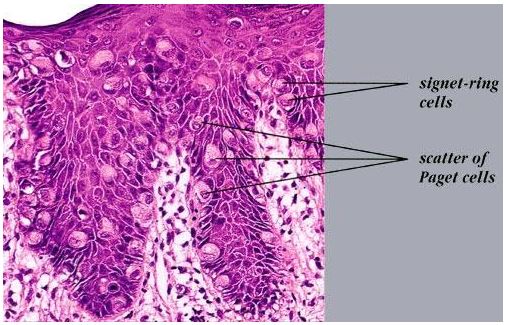
Figure 1: Extra Mammary Pagets Disease.
Cervix –ECUS
The term epithelial changes of uncertain significance (ECUS) describes a minor degree of nuclear pleomorphism limited to the basal layers of cervical epithelium in the absence of severe inflammation with associated normal mitoses, koilocytosis, or koilocytosis associated features. Comparison of follow up data in this study revealed a similar prognosis in the two groups in terms of regression to normal, persistence of low grade disease, or progression to high grade CIN giving us the conclusion that low grade cervical disease (ECUS and CIN1) should be managed according to similar treatment protocols [6].
Cervix- Microglandular Hyperplasia Cervix
Benign, nonneoplastic proliferation of endocervical glands. Also called microglandularadenosis, microglandular change. Microglandular hyperplasia (MGH) of the cervix is an epithelial (endocervical mucosa) benign abnormality (lesion) associated with gland proliferation.It is common in reproductive aged women and associated with birth control pills (progestins) or pregnancy in young women, although also present in postmenopausal women. Usually incidental, may grow as a polypoid mass [7].
Figure 2: Ovaries - Leydig Cell Hyperplasia.
If we perform oophorectomy and get the histological report of Leydig cell hyperplasia the next step should be removal of both ovaries. Also with exclusion of adrenal origin and other obvious ovarian disease, virilization in postmenopausal women may be the result of Leydig cell hyperplasia for which a bilateral salpingooopherectomy or bilateral oophorectomy is the cure [8]. A hyperandrogenic phenotype has a detrimental effect on the quality of life in postmenopausal patients as increased facial hair and loss of scalp hair may cause emotional and psychological distress [9].
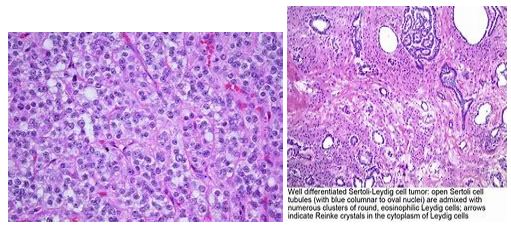
Figure 3: Fallopian Tubes – Atypical Tubal Metaplasia.
Tubal (or ciliated cell) metaplasia of the endometrium is a frequent finding in endometrial sampling specimens and is commonly associated with the follicular phase of the menstrual cycle and with anovulatory cycles[10]. Occasionally, tubal metaplasia with cytologic atypia (atypical tubal metaplasia) is encountered in non-neoplastic endometrial biopsy or curettage specimens. The features of atypical tubal metaplasia may histologically resemble some cytologic features seen in uterine serous carcinoma and serous endometrial intraepithelial carcinoma. This study evaluated the immunoprofile of atypical tubal metaplasia and the long-term outcomes in these patients. The study shows that the clinical behavior of atypical tubal metaplasia differs from that of invasive or intraepithelial serous carcinoma, as after an average follow-up period of 5 years, the presence of atypical tubal metaplasia in endometrial samplings did not increase the risk of developing hyperplasia or malignancy.
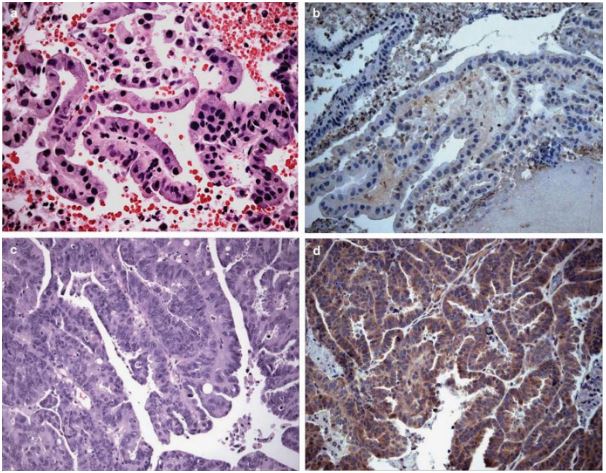
Figure 4: Atypical tubal metaplasia with pleomorphic, hyperchromatic nuclei (a) is negative for TERT (b), whereas serous adenocarcinoma (c) displays cytoplasmic staining with TERT (d). (a–d—20 x).
References:
-
- D. Barmon, L. Imchen, A. Kataki, and J. Sharma, “Extra mam- mary Paget?s disease of the vulva,” Journal of Mid-life Health. 2012;3(2):100-102.
- E. S. Trindade, P. A. Polcheira, D. B. Bas ́ılio, Z. N. Rocha, J. L. Rocha Ju ́nior, and G. R. Primo, “Invasive Paget's disease of the vulva and perianal region: a case report,” RevistaBrasileira de Ginecologia e Obstetr ́ıcia. 2004;26:329-335.
- C. O. Onaiwu, P. T. Ramirez, A. Kamat, L. C. Pagliaro, E. E. Euscher, and K. M. Schmeler, “Invasive extramammary Paget’s disease of the bladder diagnosed 18 years after noninvasiveextramammary Paget’s disease of the vulva,” GynecologicOncol- ogy Case Reports. 2014;8:pp. 27-29.
- S. K. Simon, I. K. Bolancˇa, K. Sˇentija, V. Kukura, J. Valetic ́, ˇ and A. Skrtic ́, “Vulvar Paget’s disease a case report,” Collegium Antropologicum. 2010;34(2):649-652.
- K. A. Edey, E. Allan, J. B. Murdoch, S. Cooper, and A. Bryant, “Interventions for the treatment of Paget’s disease of the vulva,” The Cochrane Database of Systematic Reviews. 2013;10:CD009245.
- M K Heatley, “The prognosis in cervical epithelial changes of uncertain significance is similar to that of cervical intraepithelial neoplasia grade 1 “ J ClinPathol. 2001;54:474-475.
- BrankoPerunovic, D.M., FarnazHasteh, M.D. “2007-2020, PathologyOutlines.com, Inc.”
- Jaya M. Mehta et al. Case Reports In EndocrinologyOvarian Leydig Cell Hyperplasia: An Unusual Case of Virilization in a Postmenopausal Woman.
- U. Blume-Peytavi, S. Atkin, U. Gieler, and R. Grimalt, “Skin academy: hair, skin, hormones and menopause—current sta- tus/knowledge on the management of hair disorders in menopausal women,” European Journal of Dermatology. 2012;22(3):310-318.
- Crum CP, Nucci MR, Mutter GL. Altered endometrial differentiation (metaplasia) In: Crum CP, Lee KR (eds). Diagnostic gynecologic and obstetric pathology. Elsevier Saunders: Philadelphia. 2006;51-544.

