Should We Replace Tubal Ligation with Salpingectomy as Permanent Contraception?
Ying Yiing L1, Sahathevan S2 and Avni B3*
1Tunbridge Wells Hospital, Maidstone & Tunbridge Wells NHS Trust, UK
2Princess Royal University Hospital, King’s College Hospital NHS Foundation Trust, UK
3East Surrey Hospital, Surrey and Sussex health care NHS Trust, Redhill, UK
Received Date: 17/08/2020; Published Date: 04/09/2020
*Corresponding author: Sahathevan Sathiyathasan, East Surrey Hospital, Surrey and Sussex health care NHS Trust, Redhill, UK. E-mail: sathya@doctors.org.uk
Abstract
Ovarian cancer is a disease difficult to diagnose in an early stage resulting a poor prognosis. There is no effective screening tool to detect ovarian cancer at an early stage. Primary prevention of ovarian cancer came in the picture through the paradigm shift that the fallopian tube is often the origin of ovarian cancer. Opportunistic bilateral salpingectomy during benign gynaecological and obstetric surgery might have the potential to reduce the risk of ovarian cancer by as much as 65 %. Sterilisation via bilateral salpingectomy is slowly replacing bilateral tubal ligation as it is believed to decrease the incidence of ovarian cancer.
Keywords: Ovarian Cancer; Risk-Reducing; Opportunistic; Prophylactic; Salpingectom; Sterilisation
Introduction
The overall ovarian cancer incidence increases with age with the median age of 63 years at diagnosis [1]. Epithelial ovarian carcinoma (EOC), which accounts for more than 85% of all ovarian cancers, is more aggressive than non-EOC and it is responsible for 90% of deaths due to ovarian cancer. Despite increasing awareness, symptoms of ovarian cancer are often vague and the majority of patients are not diagnosed until advanced-stage disease with poor survival outcome [2]. Unlike successful screening programs for cervical and breast cancer, there is no simple and reliable screening test to detect and treat pre-invasive disease in ovarian cancer.
For women at high risk of developing ovarian cancer, secondary to genetic mutations in BRCA1 or BRCA2 (found in 12-15% of cases of EOC) [3] and/or family history, studies have shown that risk-reducing bilateral salpingo-oophorectomy upon completion of child-bearing should be the standard of care [1]. However, in young premenopausal women with no genetic or family history affecting their baseline risk of ovarian cancer, the risks of early age oophorectomy greatly outweighs the benefits. This leads to recent studies that have focused on the role of fallopian tubes in the development of serous and non-serous ovarian cancer [4] with more specific areas of concern localised to the frimbrial distal end of the fallopian tubes [5]. Thus, it is not surprise that excising all or portions of the fallopian tubes has been shown to decrease the ovarian cancer risk [6]. However, it is important to recognise that there are no randomised trials supporting the practice of risk-reducing bilateral salpingectomy. The most compelling evidence to date comes from retrospective population data showing a reduction in ovarian cancer risk following hysterectomy, tubal ligation and bilateral salpingectomy. None of the women included in the study had a salpingectomy for sterilisation, and the fact that they required a rarely indicated operation may not make them representative of the average population in terms of ovarian cancer risk.
Benefits of Salpingectomy for Ovarian Cancer Reduction
Tubal ligation has a protective effect specifically against endometrioid and clear cell carcinomas of the ovary which support the theory that these tumours may be related to retrograde menses of endometrial cells [7]. Results from the Nurses’ Health Studies show that women who had undergone a tubal ligation had a 24% lower risk of ovarian cancer compared with women who did not have the procedure [8]. A population based cohort study in Sweden showed a similar decreased risk of ovarian cancer in women undergoing sterilisation [9]. By performing salpingectomy when patients undergo an operation during which the fallopian tubes could be removed in addition to the primary surgical procedure (eg, hysterectomy), the risk of ovarian cancer is reduced. In the Swedish study, women who underwent bilateral salpingectomy had a 65% reduction in the risk of ovarian cancer and women who underwent sterilisation had a 28% reduction in risk compared with women who did not undergo sterilisation, salpingectomy, hysterectomy, or bilateral salpingo-oophorectomy [10].
Prophylactic Salpingectomy During Hysterectomy
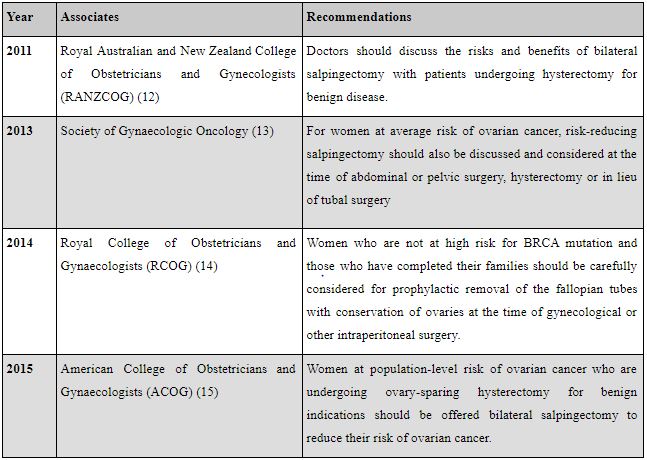
Prophylactic salpingectomy is increasingly performed in many countries. Salpingectomy at the time of hysterectomy appears to be safe and does not increase the risk of complications such as blood transfusions, readmissions, postoperative complications, infections, or fever compared with hysterectomy alone [11]. Several professional gynaecological organisations have recommended offering women at average risk of ovarian cancer opportunistic salpingectomy at the time of benign gynaecological surgery (Table 1) [12-15].
Table 1: Statements on prophylactic salpingectomy by professional gynaecological organizations.
In one large study looking at the duration of surgery, performing an opportunistic bilateral salpingectomy (OBS) during a hysterectomy may however slightly extend the operating time regardless which route either with laparoscopy (12 minutes; p < 0.001) or laparotomy (16 minutes; p < 0.001) [16]. In exceptional cases, and certainly during vaginal hysterectomy, removal of the fallopian tubes is challenging. In experienced hands routine removal of free mobile fallopian tubes during abdominal or laparoscopic surgery is easily done. Removal of diseased fallopian tubes whether or not adherent to other pelvic structures could increase operation time and the complication rate.
Prophylactic Salpingectomy during Caesarean Section
In British Columbia, Canada, recent trends regarding permanent contraception are shifting towards the use of the bilateral salpingectomy. The increased frequency of salpingectomy is largely due to emerging theoretical evidence suggesting that epithelial ovarian cancers may originate from the fallopian tube, and removing the fallopian tubes may play a role in preventing ovarian cancer [17]. Despite this practice change in the field of gynaecology, it has not expanded much to the obstetric population.
Venkatesh et alhad analysed the impact that adoption of bilateral salpingectomy at the time of cesarean would have on the medical system and in prevention of ovarian cancer, the authors performed a cost-effectiveness analysis using estimated costs per procedure, peri-operative complications, years of life expectancy gained (in quality adjusted life-years), prevention of future pregnancies, and number of ovarian cancer cases and deaths prevented [18]. Their analysis compared 3 strategies: bilateral tubal ligation, bilateral salpingectomy, and postpartum long-acting reversible contraception. Across all outcomes, long-acting reversible contraception was costlier and less effective, both in pregnancy and ovarian cancer prevention. Tubal ligation was initially less expensive than salpingectomy (£2833 vs £2883), but was less effective, resulting in fewer quality-adjusted life years. Furthermore, using the previously demonstrated ovarian cancer risk reduction with salpingectomy of 64%, it was concluded that salpingectomy would result in 422 fewer ovarian cancer diagnoses and 252 fewer ovarian cancer deaths in the study population (110,000 pregnant women desiring permanent sterilisation at the time of cesarean) over 10 years. As a result, the base case analysis ind cates that salpingectomy is more cost-effective and beneficial than any other method. A recent RCT comparing OBS and bilateral tubal ligations at the time of caesarean delivery in women desiring permanent contraception, showed that an OBS added 15 minutes to the total operating time (p = 0.004) with no difference in total procedure estimated blood loss or in postoperative complications [19].
Discussions
In the United Kingdom, female sterilisation will not be available on non-medical grounds unless the woman has had at least 12 months’ trial using Mirena or long acting etonogestrel-releasing implant (such as Nexplanon) and found it unsuitable (in line with the UK Medical Eligibility Criteria for Contraceptive Use 2009). If a woman has a personal history of breast or other hormonal cancer and wish to avoid all hormonal methods then a copper intrauterine device should be suggested for the trial period. Female sterilisation is funded by the Clinical Commissioning Groups (CCG) if the criteria is met. The Faculty of Sexual and Reproductive Healthcare guidance for female sterilisation is restricted to tubal occlusion only whether it can be performed at the time of caesarean section or at an interval after pregnancy using modified Pomeroy or Filshie clips [20]. Therefore, sterilisation with salpingectomy is not widely used in the United Kingdom due to the guidance from the local professional bodies that we have adopted.
The available evidence so far suggests that opportunistic salpingectomy is safe and likely to be effective and cost-effective as an ovarian cancer prevention strategy. However, there has been skepticism about the safety and absolute benefit of this practice [21]. There are no long-term studies confirming that salpingectomy does not compromise ovarian function. Opportunistic salpingectomy does not appear to affect ovarian function in the short term. Morelli et al. demonstrated no significant difference in pre- and postoperative levels of anti-Mullerian hormone (AMH), follicle stimulating hormone (FSH), antral follicle count, mean ovarian diameter, and peak systolic velocity, as measures of ovarian function assessed 3 months after hysterectomy [22]. On the other hand, Ye et al. reported that bilateral salpingectomy was associated in decreased AMH and increased FSH levels in women seeking IVF, compared to those not having tubal surgery [23]. It is suggested that salpingectomy undermines ovarian reserve, although there was no difference in the total number of follicles and oocytes retrieved from both ovaries. These outcomes will remain unknown for at least another one or two decades. As sterilisation procedures are generally performed on a younger population, any detrimental effect on ovarian function could have a greater negative impact. The absolute benefit from opportunistic salpingectomy is estimated at a number needed to treat (NNT) of 273 to prevent one case of ovarian cancer during hysterectomy, and NNT of 366 for surgical sterilisation (instead of tubal ligation). While these NNT estimates seem high, they are comparable to the NNT of 324 to prevent one case of cervical cancer with human papilloma virus vaccination [24], which reflect the relatively low incidence of ovarian and cervical cancers in our population.
There are several small studies supporting the feasibility of bilateral salpingectomy at caesarean section, but larger studies are required to confirm this finding, as common-sense-based medicine would suggest an increased risk of complications due to the engorged adnexa in the peripartum period. The downside in changing from a tubal sterilisation to an OBS, could mean adding additional port(s) (three ports instead of two) and it could also include the use of another surgical instrument with its own energy and complication rate. When OBS is considered in patients for sterilisation, we need to underline the definite character of this technique as 2-5% of patients will show regret later in life, especially in younger patients (younger than 40).
In a study looking at immediate and short-term complications and surgical duration among women having laparoscopic salpingectomy (n=81) or tubal occlusion (n=68) for female sterilisation there was no difference in complication rate, but the average surgical time was 6 min longer for salpingectomy compared to occlusive methods (44±13 min versus 38±15 min, respectively, p=0.018) [25]. There is no doubt thatperforming salpingectomy to the fallopian tubes that are adherent to other pelvic structures could increase operation time and the complication rate. Laparoscopic sterilisation with tubal occlusion is classified as basic laparoscopic surgery training in the RCOG training matrix for the trainees in the United Kingdom. If we are replacing tubal occlusion with salpingectomy, a higher level of training level is required and the trainees will not be able to get this laparoscopic or open salpingectomy competency signed off until they become senior trainees. This will have an impact in the training programme.
Conclusion
Early diagnosis of ovarian cancer is a challenge. It may be more beneficial to focus on prevention strategies rather than early diagnostic tools. Based on the current understanding of the aetiology of ovarian cancer, performing a bilateral salpingectomy for postpartum sterilisation provides an attractive and effective method for reducing the risk of developing this life threatening disease. However, the current evidence makes it difficult to make a clear recommendation of salpingectomy over tubal occlusion for sterilisation. Women should be informed of the potential benefits and risks of the different procedures, including the uncertainty around the effect of salpingectomy on ovarian function. If the sterilisation is performed during a caesarean section, the theoretical risk of increased bleeding should be discussed. The potential benefits of salpingectomy should not influence the choice of contraceptive method and non-surgical alternatives, or even male surgery, can be recommended unless contraindicated. It is worth noting that even with an optimistic estimate of the reduction in ovarian cancer risk, over 300 salpingectomies would be required to prevent one case of ovarian cancer. With the new and innovative method of permanent contraception being introduced, it is important to have health policy and guidelines for contraceptive techniques and methods to reflect current evidence. Time will tell if the benefits warrant subjecting women to the inherent risks of surgery.
References:
- Morgan RJ Jr, Armstrong DK, Plaxe SC, et al. NCCN ovarian cancer practice guidelines. Natl Compr Cancer Netw. 2017;1:MS4-8.
- Torre LA, Trabert B, DeSantis CE, Miller KD, Samimi G, Runowicz CD, et al. Ovarian cancer statistics, 2018. CA Cancer J Clin. 2018;68:284-96.
- Hennessy BT, Timms KM, Carey MS, Gutin A, Meyer LA, Flake DD 2nd, et al. Somatic mutations in BRCA1 and BRCA2 could expand the number of patients that benefit from poly (ADP ribose) polymerase inhibitors in ovarian cancer. J Clin Oncol. 2010;28:3570-6.
- Tone AA, Salvador S, Finlayson SJ, et al. The role of the fallopian tube in ovarian cancer. Clin Adv Hematol Oncol. 2012;10:296-306.
- Crum CP, Drapkin R, Kindelberger D, et al. Lessons from BRCA: the tubal fimbria emerges as an origin for pelvic serous cancer. Clin Med Res. 2007;5:35.
- Rice MS, Hankinson SE, Tworoger SS. Tubal ligation, hysterectomy, unilateral oophorectomy, and risk of ovarian cancer in the Nurses’ Health Studies. Fertil Steril. 2014;102:192.
- Garavaglia E, Sigismondi C, Ferrari S, Candiani M. The origin of endometriosis-associated ovarian cancer from uterine neoplastic lesions. Med Hypotheses. 2018;110:80-2.
- Rice MS, Hankinson SE, Tworoger SS. Tubal ligation, hysterectomy, unilateral oophorectomy, and risk of ovarian cancer in the Nurses’ Health Studies. Fertil Steril. 2014;102:192-8.e3.
- Falconer H, Yin L, Gronberg H, Altman D. Ovarian cancer risk after salpingectomy: a nationwide population-based study. J Natl Cancer Inst. 2015;107(2):dju410.
- Yoon SH, Kim SN, Shim SH, Kang SB, Lee SJ. Bilateral salpingectomy can reduce the risk of ovarian cancer in the general population: a meta-analysis. Eur J Cancer. 2016;55:38-46.
- McAlpine JN, Hanley GE, Woo MM, Tone AA, Rozenberg N, Swenerton KD, et al. Opportunistic salpingectomy: uptake, risks, and complications of a regional initiative for ovarian cancer prevention. Ovarian Cancer Research Program of British Columbia. Am J Obstet Gynecol. 2014;210:471.e1-11.
- Brand AH. The RANZCOG College Statement on prophylactic oophorectomy in older women undergoing hysterectomy for benign disease: is the evidence sufficient to change practice? Aust N Z J Obstet Gynaecol. 2011;51:296-300.
- Society of Gynecologic Oncology. SGO clinical practice statement: salpingectomy for ovarian cancer prevention [Internet]. Chicago (IL): Society of Gynecologic Oncology; [cited 2018 Jul 19]. Available from: https://www. sgo.org/clinical-practice/guidelines/sgo-clinical-practice-statement-salpingectomy-for-ovarian-cancer-prevention/.
- Royal College of Obstetricians and Gynecologists. High-grade serous carcinomas, the distal fallopian tube as the origin of non-uterine pelvic (scientific impact paper No. 44). London: Royal College of Obstetricians and Gynaecologists; 2014.
- American College of Obstetricians and Gynecologists; ACOG Committee on Practice Bulletins--Gynecology; ACOG Committee on Genetics; Society of Gynecologic Oncologists. ACOG Practice Bulletin No. 103: hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2009;113:957-66.
- McAlpine JN, Hanley GE, Woo MMM et al. Opportunistic salpingectomy: uptake, risks, and complications of a regional initiative for ovarian cancer prevention. Am J Obstet Gynecol. 2014;210:471.e1-471.e11.
- McAlpine JN, Hanley GE, Woo MMM, et al. Opportunistic salpingectomy: uptake, risks, and complications of a regional initiative for ovarian cancer prevention. Am J Obstet Gynecol. 2014;210(5):471.e1-e11.
- Venkatesh KK, Clark LH, Stamilio DM. Cost-effectiveness of opportunistic salpingectomy vs tubal ligation at the time of cesarean delivery. Am J Obstet Gynecol. 2019;220:106.e1-10.
- Subramaniam A, Blanchard CT, Erickson BK et al. Feasibility of Complete Salpingectomy Compared With Standard Postpartum Tubal Ligation at Cesarean Delivery. Obstet Gynecol. 2018;132:20-7.
- Faculty of Sexual and Reproductive Healthcare Clinical Guideline: male and female sterilisation, September 2014.
- Narod SA. Salpingectomy to prevent ovarian cancer: a countercurrents series. Curr Oncol. 2013;20:45-7.
- Morelli M, Venturella R, Mocciaro R, Di Cello A, Rania E, Lico D, et al. Prophylactic salpingectomy in premenopausal low-risk women for ovarian cancer: primum non nocere. Gynecol Oncol. 2013;129:448-51.
- Ye XP, Yang YZ, Sun XX. A retrospective analysis of the effect of salpingectomy on serum antiMullerian hormone level and ovarian reserve. Am J Obstet Gynecol. 2015;212:53.e1-10.
- Brisson M, Van de Velde N, De Wals P, Boily MC. Estimating the number needed to vaccinate to prevent diseases and death related to human papillomavirus infection. CMAJ. 2007;177:464-468.
- Westberg J, Scot F, Creinin MD. Safety outcomes of female sterilization by salpingectomy and tubal occlusion. Contraception. 2017;95:505-8.
-

