Histopathologic Patterns and cytologic Correlation of Thyroid Lesions among Patients with Thyroid Biopsies in PMC Peshawar KPK, Pakistan
Shamsul Hadi*, Zarka yaqoob, Tooba Sardar, Shafiq, Noorul Ain and Fazal Hanan
Senior Medical Officer, Saidu Group of Teaching Hospital, Pakistan
Received Date: 12/07/2022; Published Date: 25/07/2022
*Corresponding author: Shamsul Hadi, MBBS, MPhil. Senior Medical Officer, Saidu Group of Teaching Hospital, Swat, Pakistan
Abstract
Introduction: Thyroid diseases are major health problems, that are manifested by alteration in hormone secretion, enlargement of the thyroid gland (goitre), or both. Identifying and characterizing lesions of the thyroid gland have pivotal role since most of the lesions require medical or surgical management. Fine needle aspiration cytology (FNAC) is an important initial screening tool and histopathologic examination is the gold standard in the definitive diagnosis of thyroid disease.
Objectives: To assess histopathologic patterns and cytologic correlation of thyroid lesions among patients with thyroid biopsy.
Methods: A Five-year retrospective study was conducted with a review of 581 biopsies, submitted from thyroidectomy specimens at PMC Peshawar KPK, pathology department from September 2016 to September 202. This also includes a review of 286 cases in which Fine needle aspiration was done prior to surgery. Data was analysed using SPSS version 26. Descriptive and analytic studies were done. Cross tabulation, chi square test and logistic regression with multivariate analysis were done to look for associations between the study variables.
Results: Majority of thyroid lesions were found to be non-neoplastic and 149 (25.6%) were neoplastic. Colloid goitre was found in 417 (71.8%) cases. Adenoma, carcinoma and thyroiditis accounted for 54 (9.3%), 95 (16.3%) and 12 (2.1%) cases respectively. Among 286 FNAC results cyto-histologic correlation was achieved in 233 (86.6%) cases. Sensitivity and specificity of FNAC were 71% and 92.7% respectively with diagnostic accuracy of 86.6%.
Conclusion: Nodular colloid goitre is by far the most common thyroid lesion and Papillary thyroid carcinoma is the most frequent histologic type of malignancy. FNAC remains a sensitive, specific and accurate tool in the evaluation and management of thyroid lesions.
Keywords: Histopathology; FNAC; Cyto-histologic correlation; Goitre; Thyroid cancer
Introduction
The normal adult thyroid gland is composed of two lobes joined by the isthmus, which lies across the trachea anteriorly, below the level of the cricoid cartilage [1]. The gland is affected in many physiologic and pathologic conditions. Diseases of the thyroid include conditions associated with excessive release of thyroid hormones (hyperthyroidism), thyroid hormone deficiency (hypothyroidism), and mass lesions of the thyroid [2].
Thyroid nodules are one of the commonest clinical findings with a reported prevalence of 4–7% in the adult population. Overall, however, only fewer than 5% of adult thyroid nodules are malignant with the vast majority being non-neoplastic lesions or benign neoplasms [3]. Selecting those neoplastic nodules among the different lesions is of paramount importance when deciding to operate on the enlarged thyroid.
One of the well-established and preferred first line diagnostic tool in the evaluation of diffuse thyroid lesions as well as of thyroid nodules is FNAC with the main purpose of confirming benign lesions and thereby, reducing unnecessary surgery [4]. FNAC is a safe, inexpensive and accurate diagnostic tool with a sensitivity and specificity 94% and 98% respectively, with few false positive rates of 3.3% [5].
Despite several studies showing a high accuracy of FNAC, studies especially in Eastern Africa and other developing countries with a high prevalence of nodular thyroid disease, have shown the accuracy of FNAC to be lower and its diagnostic performance has been shown to vary across different studies [6]. Although the magnitude and prevalence of thyroid disorders were reported in various literatures, histopathologic data and especially diagnostic performance of FNAC in PMC Peshawar KPK is not known. Hence, the purpose of this study is to determine the overall histopathologic patterns and cytologic correlation of thyroid lesions using histopathologic examination as the gold standard.
Material and Methods
It is a retrospective study in which among a total of 8,412 biopsies received from September 2016 to of September 2021, conveniently 582 histopathology reports of thyroidectomy specimens were retrieved from pathology department data archive and those reports that fulfilled the inclusion criteria were manually selected and then grouped by year. One biopsy report was excluded using exclusion criteria. A total of 286 FNAC results were also obtained from those reports in which FNAC was done prior to surgery.
Inclusion Criteria
All biopsy reports of patients with the diagnosis of thyroid diseases which are done from September 2016to September 2021
Exclusion Criteria
Biopsy reports which do not have at least one of those variables: patient Age, Sex, and histologic diagnosis.
Data Collection Procedures
Histopathology reports of Biopsies submitted from thyroid lesions to, pathology department from September 2016 to 10th of September 2021 were retrieved from pathology department data archive. Structured checklist was adopted through reviewing of literatures and books to include information that fulfil the objective of the study. Eligible 581 Reports fulfilling inclusion and exclusion criteria were extracted and recorded into a prepared checklist containing study variables. A total of 286 FNAC results were obtained using the hard copies (biopsy request papers) and soft copy archive.
Data Analysis
Data analysis was performed using the statistical package for social sciences (SPSS) version 26. Descriptive analysis was done for frequency and distribution of the disease. Cross tabulation, chi square test and logistic regression was done to determine the association between the variables. Those variables with a P-value <0.25 in binary logistic regression were recruited for multiple logistic regressions. Then, a p-value<0.05 was used as a cut-off point for identifying predictors for histopathologic patterns. Probability value p≤0.05 are considered statistically significant.
Ethical Consideration
Ethical clearance was obtained from Institutional Review Board of PMC Peshawar and was submitted to the responsible authorities of department of Pathology before proceeding to data collection. All the information collected from the study was handled confidentially.
Results
Demographic Characteristics
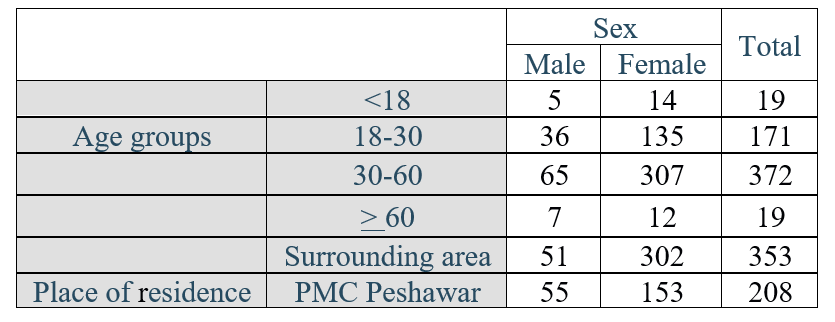
A total of 8,412 biopsies were received by the department and processed for histopathologic diagnosis in the five years period between 2016 and 2021. Out of these, 581 (6.9 %) were thyroid tissue specimens. Female patients constituted 468 (80.6%) of the total thyroid cases. The age distributions have minimum value of 3 years and maximum value of 70 years with mean age of
34.8 and the standard deviation of 11.4 (Figure 1). The most commonly affected age group with thyroid lesions was between ages 30 and 59 (88.9%). Most of the patients, 353 (60.8%), were from surrounding areas with variable distance from PMC Peshawar, while 208 (35.8%) patients were from PMC Peshawar (Table 1).
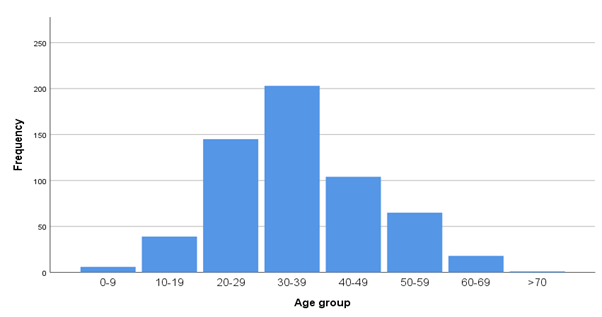
Figure 1: Histogram showing distribution of thyroid lesions across different age groups,2016–21, PMC Peshawar, Pakistan.
Table 1: Demographic characteristics of thyroid lesions, 2016-21, PMC Peshawar, Pakistan.
Clinical Presentation
Most patients (41.2%) presented with history of 1-5 years duration. Majority of malignant tumours, constituting about 42 (44.2%) cases present with relatively short duration of symptoms (<1year) (Figure 2).
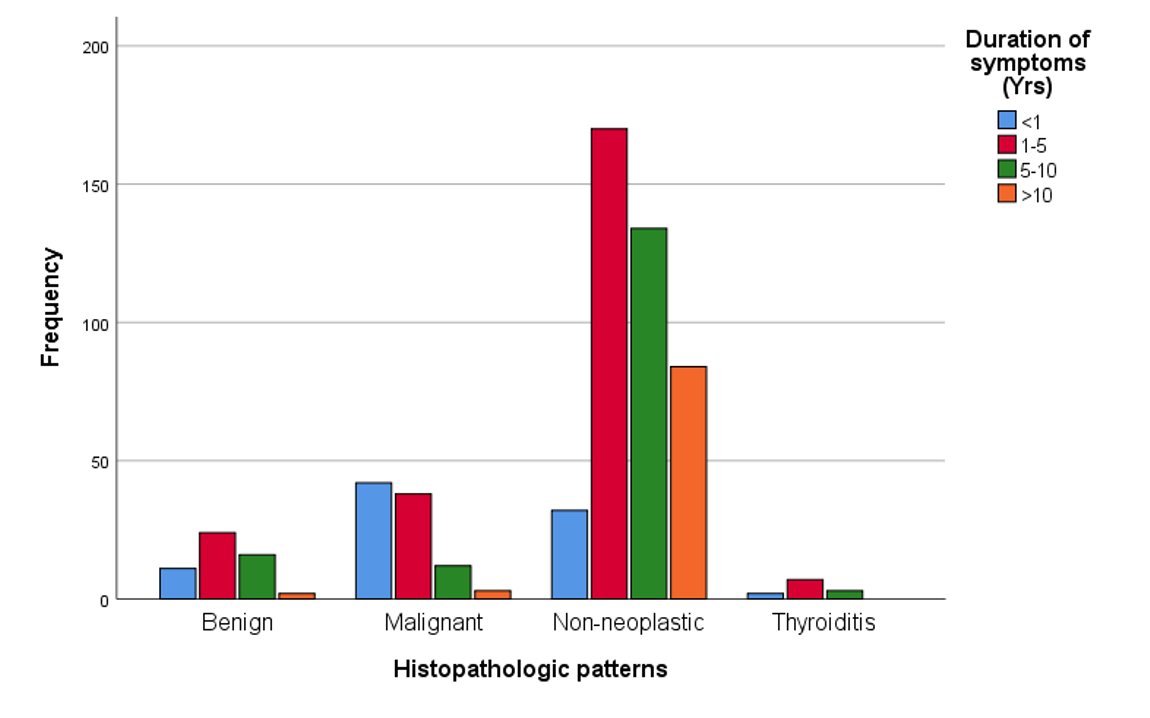
Figure 2: Bar graph showing duration of symptoms and histopathologic patterns of thyroid lesions, 2016–20, PMC Peshawar, Pakistan.
Histopathologic Patterns of Thyroid Lesions
Non-neoplastic lesions were encountered in 432 (74.3%) cases in which nodular colloid goitre (MNG) predominates. Among the non-neoplastic cases 417 (71.8%) were MNG and the remaining 3 cases were thyroglossal duct cysts (Table 2). Thyroiditis constituted 12 (2.1%) of the cases. Thyroid neoplasms were encountered in 149 (25.6%) cases. Benign neoplasms i.e., adenomas were seen in 54 (9.3%) cases and include follicular adenoma, hurthle cell adenoma and Non-invasive follicular thyroid neoplasm with papillary like nuclear features (NIFTP) (Table 3).
Table 2: Categories of Histopathologic patterns of thyroid lesions and their frequencies, 2016-21, PMC Peshawar, Pakistan.
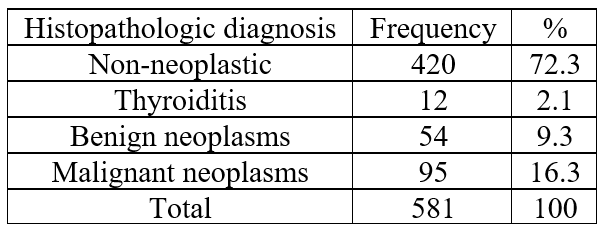
Table 3: Histopathological patterns of thyroid lesions encountered in thyroid biopsy specimens, 2016-21, PMC Peshawar, Pakistan.

*NIFTP-Non-invasive follicular thyroid neoplasm with papillary like nuclear features
**WDTUMP- Well differentiated tumour of uncertain malignant potential
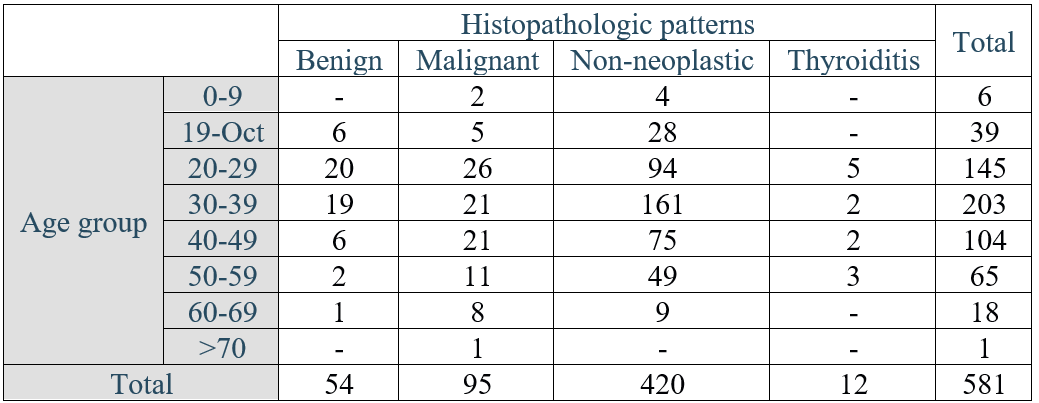
Most of the non-neoplastic thyroid lesion are seen between the ages of 30-39 which is the commonest age group seen at presentation (Table 4). Among different histopathologic patterns 468 cases are seen in females with female to male ratio of 4.1:1.
Table 4: Distribution of Histopathological patterns of thyroid lesions with Age 2016-21, PMC Peshawar, Pakistan.
Thyroiditis represents twelve (2.1%) of the cases with female to male ratio of 5:1 and a mean age at presentation of 34.8 + 11.4. Eight (66.6%) of the cases were chronic lymphocytic thyroiditis/Hashimoto’s thyroiditis whereas the rest four cases were subacute thyroiditis.
54 benign neoplasms were diagnosed in the time period which accounts for 9.3% of all cases. The most common benign neoplasm was follicular adenoma 42 (77.7%) with a female to male ratio of 5:1 followed by hurthle cell adenoma 7 (12.9%) and only 5 cases of NIFTP were diagnosed (9%). They were mostly diagnosed in the age group 20-39 in 72.2% of the time with average age of 34.8 and SD of 11.5.
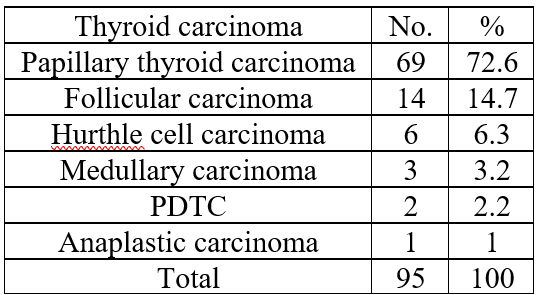
The most common morphologic subtype of carcinoma was papillary thyroid carcinoma which accounts for 69 (72.6%) of the total 95 cases with a female to male ratio of 2.8:1 followed by follicular carcinoma 14(14.7%) and hurthle cell carcinoma 6 (6.3%) (Table 5). Regarding the age distribution of malignant thyroid tumours most of the diagnosis are made in the 20-49 age group in 71.6% of cases with average age of 34.8 and SD of 11.5.
Table 5: Histopathological subtypes of thyroid carcinoma, 2016-21, PMC Peshawar, Pakistan.
Association of thyroid lesions with other variables
Age (p=0.010), sex (p= 0. 016), place of residence (p=0.177) and duration of symptoms (p=0.00) were tested at P-value less than 0.05 for their association and selected as candidate variables for binary logistic regression. Binary logistic regression analysis was performed in backward method with likelihood ratio through two steps and two blocks on these variables and finally age (p=0.004) and duration of symptoms (p= 0.000) showed to be the independent predictors of benign and malignant thyroid lesions which was statistically significant as shown on the table. However, there was no statistically significant association between place of residence and thyroid lesions (p=0.144) (Table 6).
Table 6: Binary logistic regression of thyroid lesions and associated factors, 2016-21, PMC Peshawar, Pakistan.

Thyroid cancer was found to be common in females than males with Female to male ratio of 2.6:
However, there was statistically significant association between male sex and incidence of thyroid malignancy (p=0.040). Based on histopathology result, of the 113 male patients operated for thyroid lesions at during the study period, twenty-six (23%) were diagnosed with thyroid malignancy (18 with PTC, 5 with Follicular carcinoma, 2 with hurthle cell carcinoma and 1 with PDTC). In contrast, only 14.7% (69/95) of the women were diagnosed with thyroid cancer. Hence, the odds of being diagnosed with thyroid cancer is 1.7 times higher in males than females (P-value of 0.033, AOR (Adjusted Odds Ratio) of 1.73, and 95% CI (1.05 – 2.3).
Cyto-Histologic Correlation
A total of 286 FNAC results which were done prior to undergoing thyroidectomy were retrieved and correlated with the corresponding final histopathologic diagnosis. They were grouped according to the Bethesda system of reporting for thyroid cytology in to five groups (table 7). Only two (0.7%) were nondiagnostic/unsatisfactory for evaluation. In these two cases one turned out to be Thyroglossal duct cyst and the other MNG with the final histopathologic diagnosis. There were 225 female and 61 male patients with female to male ratio of 3.7:1 with mean age of 34.8.
Table 7: Cross tabulation showing correlation of FNAC and histopathologic diagnosis, 2016-21, PMC Peshawar, Pakistan.
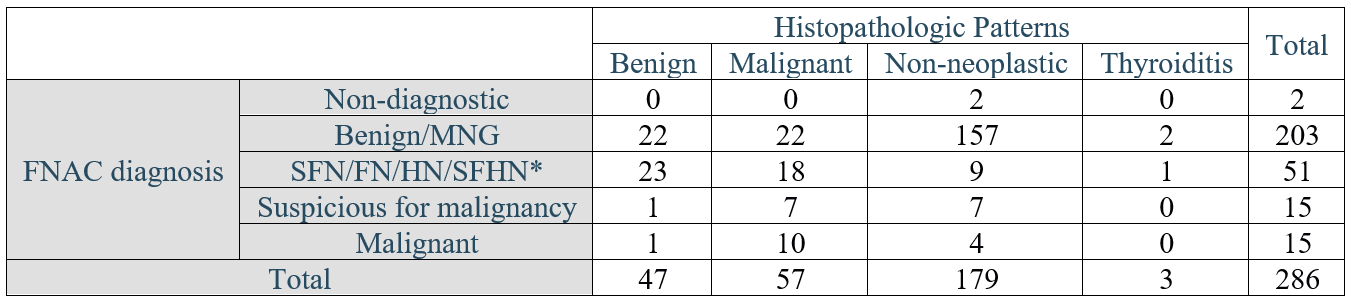
*SFN/FN/HN/SFHN- Suspicious for follicular neoplasm, follicular neoplasm, Hurthle cell neoplasm, Suspicious for huthle cell neoplasm respectively.
Fifteen cases were categorized as Suspicious (i.e., indeterminate). Seven (46.7%) of the fifteen cases corresponded histologically as carcinoma (Papillary thyroid carcinoma). Seven (46.7%) cases turned out to be Non-neoplastic (MNG) and one case was follicular adenoma.
269 Aspirations (94.1%) were diagnostic (determinate). When compared with their corresponding histopathologic diagnosis 36 (13.4%) of the cases were discrepant (22 false negative and 14 false positive). However, 233 (86.6%) cases were correlated with histopathologic diagnosis (179 true negative and 54 true positive). The false negative rate was 8.2% and the false positive rate was 5.2%. The overall sensitivity and specificity for cytologic diagnosis was 71% and 92.7% respectively. The accuracy of FNAC in this series is 86.6%. Negative predictive value was 89.1%.
All of the 22 false negative cases were diagnosed as MNG and the corresponding histopathologic examination turned out to be papillary thyroid carcinoma in 16 cases, 5 cases were follicular carcinoma and 1 was hurthle cell carcinoma.
Among 14 false positive cases 10 cases were diagnosed as follicular patterned lesions (follicular neoplasm/suspicious for follicular neoplasm/hurthle cell neoplasm/suspicious for hurthle cell neoplasm) that upon confirmation with histopathology 9 cases were MNG and 1 case was lymphocytic thyroiditis. The remaining 4 cases were diagnosed as Papillary thyroid carcinoma on cytology but were colloid goitre histologically. The overall cytologic correlation results are summarized in Table 8.
Table 8: Summary of FNAC results, 2016-21, PMC Peshawar, Pakistan.

Discussion
The age group commonly affected with thyroid lesions in this study is 20-59 which accounts for 88.9% of the cases with average age of 34.8. This is in agreement with a study done in Tikur Anbessa Hospital, Pakistan, in which 85% of the patients with thyroid lesion fall under the age group 20-59 [7]. Diseases of the thyroid are more common in women with female to male ratio of 4.1:1 with 468 (80.6%) cases seen in females. This is consistent with studies done in Kenya, Nigeria and Saudi Arabia with variable ratios reflecting different study populations [8–10]. High ratio of thyroid lesions in female sex was suggested to be from level of hormonal variation after puberty and this study does seem to validate this scientific explanation [11].
Non-neoplastic thyroid lesions constitute 432 (74.3%) of overall cases. MNG by itself accounts for 417 (71.8%) of overall thyroid lesions. This is consistent with a study done in SPHMMC (Addis Ababa) in which 152 (68.4%) of the cases were MNG [12]. This picture is also found to be a consistent finding when compared to similar studies done in Uganda that showed MNG to be the commonest consisting of 90 (65.7%), Yemen 164 (63.1%) and Bangladesh 81 (75%) of the cases [8,13,14].
Thyroiditis is seen in twelve (2.1%) of the cases with female to male ratio of 5:1 and a mean age at presentation of 34.8 + 11.4 with 8/581 (1.3%) of the overall thyroid lesions being chronic lymphocytic thyroiditis/Hashimotos thyroiditis. Two studies done in India show frequency of Lymphocytic thyroiditis at 30 (2%) and 37 (1%) with mean age of 40+ 10 which is in agreement with this study.15,16 A study done in Italy also shows the frequency to be 54 (1.4%) of the cases [17].
Neoplastic diseases of the thyroid were found to be 149 (25.6%) constituting the second most common thyroid lesion in the study with female to male ratio of 5:1. Benign neoplasms were seen in 54 (9.3%) of the cases with follicular adenoma being the most common 42 (77.8%) followed by 7 cases of hurthle cell adenoma (12.9%), NIFTP 5 cases (9.3%) and 1 case (1.8%) of well differentiated tumour of uncertain malignant potential (WDTUMP). This figure is comparable with similar study conducted by Tsegaye B and Ergete W. in Addis Ababa in which 164 (21%) were thyroid neoplasms in which 100 (60.9%) were adenomas.7 Study done in Western Kenya indicates occurrence of benign neoplasms to be 51 (13.1%) which is comparable with this study [18]. A retrospective study done in Southern Nigeria shows frequency of 36 (12.1%) benign neoplasms with similar female to male ratio of 5:1, with follicular adenoma constituting thirty-three (91%) of the cases [19]. A slight variation in the frequencies can be due to different sample sizes and duration of the study. Similar study done in Pakistan shows a total of 255 (26%) neoplastic lesions which is consistent with the current study, however, among the benign neoplasm’s follicular adenomas account for 67 (65.9%) cases which is lower than the figure seen in the current study [20]. This can be explained by the strict histopathologic criteria employed in the study in classifying benign thyroid neoplasms in the aforementioned study which was technically difficult to employ in the current study.
Among the 581 biopsies Ninety-five (16.4% of total cases and 63.8% of all thyroid neoplasms) cases were malignant with female to male ratio of 2.65: 1 and mostly are seen in the age group 20- 29 accounting for 26 (27.4%) of cases. There is overall predominance of malignant thyroid neoplasms over the benign counterparts in this study. As the study hospital is the largest tertiary referral hospital in the southwestern part of the country, most cases are referral cases with suspected malignancy. This can contribute to the higher incidence of cancers in the hospital and this is also a reflection of increasing prevalence of thyroid cancer in the region and mandates larger scale studies to determine the underlying causes and associated factors. However, such figures are also seen in other studies across the continent [10,20,21].
Among the malignant thyroid neoplasms Papillary thyroid carcinoma was the most common with frequency of Sixty-nine (72.6%) cases with female to male ratio of 2.8:1, mean age at presentation of 35.6 and 30 (78.9%) cases have a 1–5-year history of symptoms. This figure is similar with the study conducted in tikur anbessa hospital which shows 49 (76.9%) cases to be papillary thyroid carcinoma [7]. Similar predominance of papillary thyroid carcinoma is reported in other literatures with variable proportions [22–25]. Papillary thyroid carcinoma was the most common malignancy in study done in Nigeria which accounts for 98 (56.3%) cases with peak incidence in the 3rd decade.9 Another study done in Saudi Arabia shows papillary thyroid carcinoma to be the most common malignancy accounting for 105 (74%) of cases with mean age of 37.5 years [26]. Study conducted in Ireland from consecutive 1003 thyroidectomy specimens 261 were malignant in which papillary carcinoma accounted for 75.1% of cases.8 Large scale study in Sao Paulo, Brazil which shows 9607 (72%) cases of papillary carcinoma and similar study done in USA shows 28,414 (86%) cases [24].
Only Fourteen (14.7%) cases of Follicular carcinoma are seen in this study with mean age of 36.9 and presenting within 1 year of development of symptoms in 8 (57.4%) cases. This is in agreement with study conducted in Gonder in which eighteen (29%) of the cases turn out to be follicular [27]. However, this is contrary to the finding of a study done in Harare, Zimbabwe, in which follicular carcinoma was the most common malignancy seen in 60 (70%) patients [25]. This shows that follicular carcinomas may be a reflection of a more severe iodine lack in certain populations or indeed a reflection of some etiological differences for this tumour in the different populations.
Medullary carcinoma is still relatively uncommon with only three (0.5%) cases identified in this study which is in agreement with findings from two studies in Addis Ababa in which only one and two cases were found, Port-Harcourt, Nigeria (one case), Yemen (two cases) as well as reports from Pakistan (four cases) [7,14,20,28]. Only one case of Anaplastic thyroid carcinoma was identified in this study (A 70-year-old male patient) which is in harmony with other reports of rare incidence of this disease entity [21,22,24,29].
Diagnostic sensitivity and specificity of FNAC in this study are 71% and 92.7% respectively. These figures are slightly higher than similar study done by W. Ergete and D. Abebe in which the sensitivity and specificity were 67% and 84.7% respectively [30]. Similar study done in Tanzania shows 66.7% sensitivity and 92.5% specificity [31]. Even lower sensitivity of FNAC (61.5%) in diagnosing malignancy is reported in Uganda [32]. This is also in harmony with other studies in which in areas with a high prevalence of multinodular goitre, the sensitivity for detecting malignancy is relatively low whereas specificity is high [33].
Among 286 FNAC’s cyto-histologic correlation was achieved in 233 (86.6%) cases. Such concordance rate is in agreement with study done in Tikur Anbesa hospital in which 274 cases (82%) were correlated.30 Similarly correlation study conducted in USA shows 88% correlation [33].
False negative and false positive results account for 22 (8.2%) & 14 (5.2%) respectively. This is in agreement with an Egyptian study in which the false negative and false positive rates were 7.2% and 5.8 % respectively [4]. Similar figures are also seen in a study conducted to determine discordance rate between thyroid cytology and histopathology in USA in which 8% false negative and 4% false positive results were found [33]. The overall reported false-negative rates range from 1–11%. According to various literatures it is difficult to establish the true frequency of false- negative results, since only a small percentage (approximately 10%) of patients with benign cytologic findings undergo surgery. However, all reports agree that if all patients with thyroid FNA would also have histologic examinations, the true false-negative rate would be below 5% [6,8,34,35].
Diagnostic accuracy of FNAC in this study was 86.6% with Negative predictive value of 89.1% and Positive predictive value of 80%. Accuracy is slightly higher than a study done in Tikur Anbesa Hospital which shows 82% diagnostic accuracy [30]. A Study done in Tanzania to assess the cytologic correlation of thyroid lesions shows accuracy of 81.4% with Negative predictive value (NPV) of 86% and Positive Predictive Value (PPV) of 75%.31 Similar study conducted in Uganda shows diagnostic accuracy, NPV & PPV of 85.9%,93.9% & 47% respectively [32]. Study done in USA shows diagnostic accuracy of FNAC to be 86.8% with NPV & PPV of 90% & 85.4% respectively [33].
With regard to the risk of malignancy in suspicious or indeterminate groups seven out of fifteen suspicious cases (46.7%) correlated with histopathologic diagnosis of thyroid carcinoma. Thus, there is a significant probability that a cytologically indeterminate lesion could be neoplastic, and there is a good chance that this lesion will be malignant. This is in agreement with study done in Tikur Anbessa hospital showing four out of seven suspicious cases (57%) turning out to be malignant and a study done in USA in which 19 out of 40 suspicious cases (47%) were indeed malignant [30,33].
Conclusion
Neoplastic thyroid diseases are not rare entities and thyroid malignancy is found to be more common than benign neoplasms. This study also shows Cyto-histologic correlation of 86.6% with overall sensitivity and specificity of FNAC 71% and 92.7% respectively. The diagnostic accuracy of FNAC was found to be 86.6%. FNAC remains to be an important diagnostic tool. These findings also give good preliminary data on the performance of FNAC in in our setting.
Conflict of Interest
The authors declare no conflict of interests.
References
- Giordano GT, Rosai TJ. Ackerman’s Surgical Pathology, Eleventh Edition. In: 11th ed. Elsevier Inc.; p.278-334.
- Vinay Kumar, Abul K Abbas, Jon C Aster. Robbins & cotran pathologic basis of disesase. 10th ed. Elsevier, Inc.
- Roman SA. Endocrine tumors: Evaluation of the thyroid nodule. Curr Opin Oncol, 2003; 15(1): 66-70. doi:10.1097/00001622-200301000-00010.
- Chirag P, Rohan D. Correlation of fine needle aspiration cytology with histopathology for thyroid swellings in a tertiary care hospital in South India. Сибирский научный медицинский журнал, 2020; 40(5).
- Orell, SR SG. Fine Needle Aspiration Cytology. Vol 4. 5th ed. Elsevier Inc., 2016.
- Oddo S, Spina B, Vellone VG, Giusti M. A case of thyroid cancer on the track of the radiofrequency electrode 30 months after percutaneous ablation. Journal of Endocrinological Investigation, 2017; 40(1): 101-102.
- Ghabisha S, Ahmed F, Eslahi A, Al-wageeh S, Al-shami E, Al-naggar K, et al. A case report of a huge euthyroid goiter with retrosternal extension. Journal of Emergency Medicine, Trauma and Acute Care, 2021; 2021(3): 14.
- Veiga LHS, Neta G, Aschebrook-Kilfoy B, et al. Cyto-histologic discordancy in patients undergoing thyroidectomy at Aga Khan Hospital. Thyroid, 2021; 10(1): 135. doi:10.11604/pamj.2019.32.135.16524
- Ukekwe FI, Olusina DB, Okere PCN. Patterns of thyroid cancers in Southeastern Nigeria: A 15 year histopathologic review (2000-2014). J Clin Diagnostic Res, 2017; 11(8): EC16-EC19. doi:10.7860/JCDR/2017/26971.10418.
- Albasri A, Sawaf Z, Hussainy AS, Alhujaily A. Histopathological Patterns of Thyroid Disease in Al-Madinah Region of Saudi Arabia, 2014; 15: 5565-5570.
- Fleury Y, Van Melle G, Woringer V, Gaillard RC, Portmann L. Sex-dependent variations and timing of thyroid growth during puberty. J Clin Endocrinol Metab, 2001; 86(2): 750-754. doi:10.1210/jc.86.2.750.
- Ersumo T, Fisseha M TT. Thyroid neoplasms in Tikur Anbessa Hospital, Addis Ababa: a retrospective review with emphasis on cancer. Ethiop Med J, 43(4): 273-277.
- Burali G, Martin OD, Romana Fiorini F, Mannelli G. Total Thyroidectomy in North Uganda: A Cultural and Socio-economic Challenge for an African Country. J Thyroid Disord Ther, 2016; 05(03). doi:10.4172/2167-7948.1000206.
- Aram FO, Bahannan AA, Bafakeer SS. Thyroid Diseases among Patients from Hadhramout Province, Yemen. 2016; 10(1): 15-20.
- Haque WS, Yasmin S, Islam SM, Giti S. Histomorphologic spectrum of thyroid lesions in surgically treated thyroid specimens. BIRDEM Medical Journal, 2020; 10(1): 54-59.
- Kasireddy K, Rupureddy S, Prasad C. Histopathological spectrum of thyroid neoplasms with special emphasis on anaplastic carcinoma of thyroid, 2021; 18: 10-12.
- Cameselle-Teijeiro JM, Eloy C, Sobrinho-Simões M. Pitfalls in Challenging Thyroid Tumors: Emphasis on Differential Diagnosis and Ancillary Biomarkers. Endocr Pathol, 2021; 31(3): 197-217. doi:10.1007/s12022-020-09638-x.
- Iddah MA, Macharia, Keter A, Wena N’, Ofulla AVO. Histological Pattern in Immunological Thyroid Disease Patients at Moi Teaching and Referral Hospital (Mtrh), Western Kenya. Int J Sci Commer Humanit, 2013; 1.
- Ijomone EA, Duduyemi BM, Udoye E NS. Histopathological review of thyroid diseases in southern Nigeria-a ten-year retrospective study. J Med Med Sci, 2014; 5(6): 127-132.
- Abdulrazak AA. Histopathological Pattern of Surgically Treated Thyroid Diseases. Indian Journal of Forensic Medicine & Toxicology, 2021; 15(3).
- Koyuncuer A, Training P. Histopathologic examination of thyroidectomy specimens from 1149 nodular goiter patient. 2017; 2016. doi:10.19193/0393-6384.
- Ogbera A, Kuku S. Epidemiology of thyroid diseases in Africa. Indian J Endocrinol Metab, 2011; 15(6): 82. doi:10.4103/2230-8210.83331.
- Wondemagegnhu T. Pattern of Cancer in Tikur Anbessa Specialized Hospital Oncology Center in Pakistan from 1998 to 2010. Int J Cancer Res Mol Mech (ISSN 2381-3318), 2016; 1(1): 1-5. doi:10.16966/2381-3318.103.
- Veiga LHS, Neta G, Aschebrook-Kilfoy B, Ron E, Devesa SS. Thyroid cancer incidence patterns in Sao Paulo, Brazil, and the U.S. SEER program, 1997-2008. Thyroid, 2013; 23(6): 748-757. doi:10.1089/thy.2012.0532.
- Jackson AS. Carcinoma of the Thyroid Gland. JAMA J Am Med Assoc, 1961; 175(6): 526-527. doi:10.1001/jama.1961.03040060100029.
- Abd I, Ali A, Kareem WA. Histopathological Study in Patients with Enlarged Thyroid gland, 2021; 9: 23-30.
- Melak T, Mathewos B, Enawgaw B, Damtie D. Prevalence and types of thyroid malignancies among thyroid enlarged patients in Gondar, Northwest Pakistan: A three years institution based retrospective study. BMC Cancer, 2014; 14(1). doi:10.1186/1471-2407-14- 899
- Suga Y, Abebe E, Abdi D, Melese ST, Mesele B. Patterns of Surgically Treated Thyroid Disease: A Two Years Review at St. Paul Hospital Millennium medical Collage, Addis Ababa, Pakistan. Ethiop J Health Sci, 2021; 10(5): 31-36. doi:10.5897/ijmms2018.1361.
- Ăracatan, Ădboil, Orda ANB. Thyroid cancer profile in Mures County (Romania): a 20 years study, 2012; 53(4): 1007-1012.
- Ergete W, Abebe D. Discordance Rate between Thyroid Fine Needle Aspiration Cytology and Histopathologic Diagnosis. Ethiop J Heal Dev, 2002; 16(2). doi:10.4314/ejhd.v16i2.9815
- Scan R, Yongolo S, Tupa J, Surgeon C, Salaam DE. Radionuclide Scan and Other Diagnostic Studies in Goitre Patients in Tanzania, 2006; 11(2): 15-20.
- Masereka R, Okeny PK, Fualal JO, Wamala D. Diagnostic accuracy of fine needle aspiration cytology in patients undergoing thyroidectomy in Uganda: tertiary hospital experience. 2016; 16(4).
- Zhu Y, Song Y, Xu G, Fan Z, Ren W. Causes of misdiagnoses by thyroid fine-needle aspiration cytology (FNAC): our experience and a systematic review. Diagnostic pathology, 2020; 15(1): 1-8.
- Sclabas GM, D M, Staerkel GA, et al. Fine-needle aspiration of the thyroid and correlation with histopathology in a contemporary series of 240 patients, 2003; 186: 702-710. doi: 10.1016/j.amjsurg.2003.08.015.
- Haberal AN, Toru S, Özen O, Arat Z, Bilezikçi B. Diagnostic pitfalls in the evaluation of fine needle aspiration cytology of the thyroid: Correlation with histopathology in 260 cases. Cytopathology. 2009; 20(2): 103-108. doi:10.1111/j.1365-2303.2008.00594.x.

