Feasibility and Safety of Single-Stage Laparoscopic Cholecystectomy with ERCP for Concomitant Gallstones and Bile Duct Stones
Easwaramoorthy S*, Pranesh Sridhar, Gurusamy Govindan, Haridra S, Sakthivel C and Venkatesh
Department of Surgery, Lotus hospital & Research Centre, India
Received Date: 03/05/2025; Published Date: 09/06/2025
*Corresponding author: Dr. Sundaram Easwaramoorthy, Prof & HOD, Department of Surgery, Lotus hospital & Research Centre, Erode, Tamil Nadu, India
Abstract
Background: In patients with gallstones, nearly 15% of them have concomitant bile duct stones. 2 stage management with ERCP followed by Laparoscopic cholecystectomy has been the common practice. But single session management could be safe and economical.
Aim: To evaluate the feasibility of single-stage laparoscopic cholecystectomy along with ERCP as a treatment option for gallstones and CBD stones.
To compare the outcomes of one-stage management to the conventional two-stage approach.
Methodology: It was a prospective observational study at a tertiary care teaching hospital in India. All cases of gallbladder stones with bile duct stones were assessed clinically, along with Liver function tests and serum amylase. Patients had undergone either CT upper abdomen or MRCP to confirm the presence of both GB and CBD calculi. A select group of cases with concomitant GB and CBD stone was taken up for single-stage Laparoscopic cholecystectomy with intra-operative ERCP. Total operative time, number of days of stay, and incidence of post-ERCP pancreatitis were the key outcome measures noted.
Inclusion Criteria:
- Radiologically confirmed GB and CBD stones.
- ASA grades 1,2 &3.
Exclusion Criteria:
- Jaundice >5mg.dl
- Large CBD stones >10mm
- Previous major upper abdomen surgeries
- Acute cholangitis
- Acute severe pancreatitis
- Pregnancy
- Malignancy
Study Design: Single Centre Prospective Observational study.
Result: On comparing various aspects, it is evident that single-stage management of concomitant GB and CBD stones has advantages like a significant reduction in hospital stay (p-value <0.001), single anesthesia, reduction in overall cost, less incidence of post-ERCP hyperamylasaemia (p-value 0.002) without compromising stone clearance with a stone clearance rate of 96.5%,
Conclusion: Single-session Lap cholecystectomy with ERCP is feasible with acceptable morbidity, provided the required resources and expertise are available in the center. Several prospective studies have substantiated their superiority over the two-session approach, and a prospective randomized study is the need of the hour.
Keywords: Single session laparoscopic cholecystomy with ERCP; Concomitant GB and CBC stone; MRCS; Post ERCP pancreatitis; Intra-operative ERCP; Cholelithiasis; Choledocholithiasis; Endoscopic Retrograde Cholangio Pancreatography (ERCP); Laparoscopic cholecystectomy (LC)
Introduction
In case of cholelithiasis, 15% of patients have concomitant bile duct stones [1-3]. Delayed or failed management of bile duct stones could lead to cholangitis, biliary pancreatitis, etc. Currently, laparoscopic cholecystectomy (LC) is the treatment of choice for gallbladder stones, while there are several options for the management of bile duct stones. There still exists a dilemma in choosing therapy for concomitant gallstones and CBD stones. Pre-operative ERCP followed by laparoscopic cholecystectomy (pERCP + LC) is the standard of care. However, this twin-stage approach has some disadvantages, such as prolonged hospital stay, the need for 2 sessions of anaesthesia, and increased incidence of postoperative pancreatitis. Therefore, single-session intraoperative ERCP with LC (iERCP + LC) is proposed [4]. Being a tertiary surgical centre with many patients presenting with concomitant gallstones and bile duct stones, we aimed to study the feasibility and safety of a single session approach (iERCP+LC) compared to the conventional two-stage approach (pERCP +LC).
Objectives: To evaluate the feasibility and safety of single-stage (iERCP +LC) as a treatment option for concomitant GB and CBD stones.
Patients and Methodology
It is a single-centre prospective observational study conducted from May 2023 to December 2024. A total of 58 patients who met the eligibility criteria were included namely, radiologically confirmed GB and CBD stones with CBD stone < 1 cm, ASA grade <3. Patients with previous major upper abdomen surgeries, acute cholangitis, pregnancy, and suspected malignancy were excluded. Patients presenting with signs and symptoms of gallstone disease are evaluated with complete blood count, urea, creatinine, liver profile, serum amylase, and prothrombin time. Radiological evaluation done by Ultrasound abdomen, Contrast CT scan of abdomen, and or MRCP, and confirmation of concomitant CBD stones were made. All patients eligible for the study were informed and consented to the single session procedure they would undergo. We performed Laparoscopic cholecystectomy first, followed by ERCP as a routine for all patients under general anaesthesia. The collected outcome data of a single-session study were compared with historical study data of our patients who had undergone a two-session approach before this study period, and also with two more similar international studies. The study aimed to compare the data for the clearance of stones, frequency of imaging, duration of surgery, incidence of post-ERCP pancreatitis, and length of stay.
Operative Procedure
After obtaining informed written consent from the patient, we proceeded with Laparoscopic cholecystectomy under general anaesthesia. Conventional 4-port cholecystectomy was done, and the drain was kept in the subhepatic region. We noted the size of the bile duct and gently stroked the bile duct with the back of the Maryland forceps to facilitate bile drainage through the ampulla. After the completion of the surgery, ERCP was done by the same surgeon with the patient remaining in the supine position, and biliary cannulation was done using CV 150 Olympus duodenoscope and 3-lumen bow wire sphincterotome (Microvasive, Boston Scientific). Selective guidewire-directed biliary cannulation was done, and iodine contrast was injected to determine the size and number of bile duct stones. Sphincterotomy and biliary balloon sweep were done to remove the stones and sludge. Balloon occlusion cholangiogram was done to confirm stone clearance. 7F plastic stent was deployed only if any suspicion of residual stone fragment or sludge. Biliary balloon sphincteroplasty was done in case of a stone bigger than 10mm. Prophylactic rectal indomethacin suppositories (100mg) were administered in all cases.
Postoperatively, serum amylase and bilirubin were monitored, and all outcome variables were noted. The drain was removed after 24 to 48 hours, and the biliary stent was removed after 10 days.
Results
Table 1: Demographics.
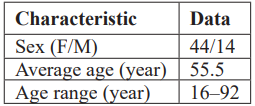
The mean value of pre-op bilirubin is 2.46 ± 2.33 standard deviation (shapiro wilk p value <0.001). The mean stone size is 5.56mm with SD of ±1.71mm. The mean CBD diameter is 7.10mm (±1.72mm). Nineteen patients had presented with biliary pancreatitis with mean serum amylase level of 315U/L. Other important parameters like presence of comorbidities, average duration of surgery, total length of hospital stay, and number of scans were collected and analysed.
Table 2: Comparison of pre-op vs post-op amylase and bilirubin levels.

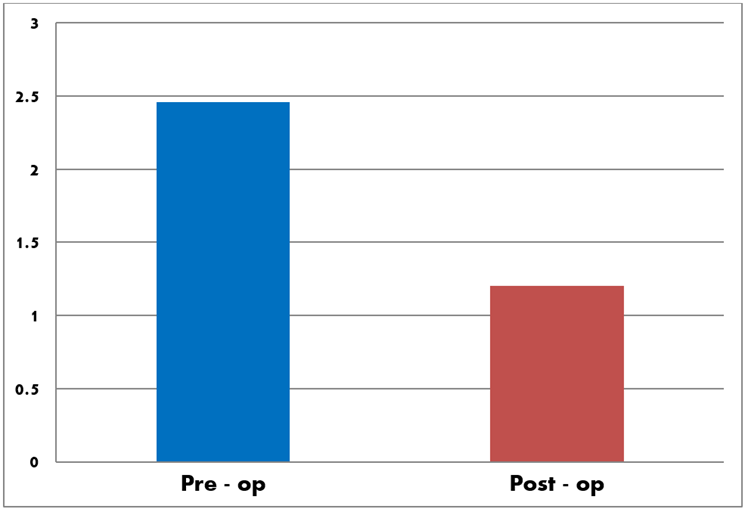
Figure 1: Comparison of mean value of pre-op bilirubin to post- op levels.
From the above data (Table 2), it is evident that a significant drop in 48-hour serum bilirubin (Figure 1) and amylase (Figure 2) was achieved in the single session approach (iERCP+LC). The efficacy of iERCP+LC in tackling biliary pancreatitis (p value <0.012) is established with no compromise in other parameters, as discussed later.
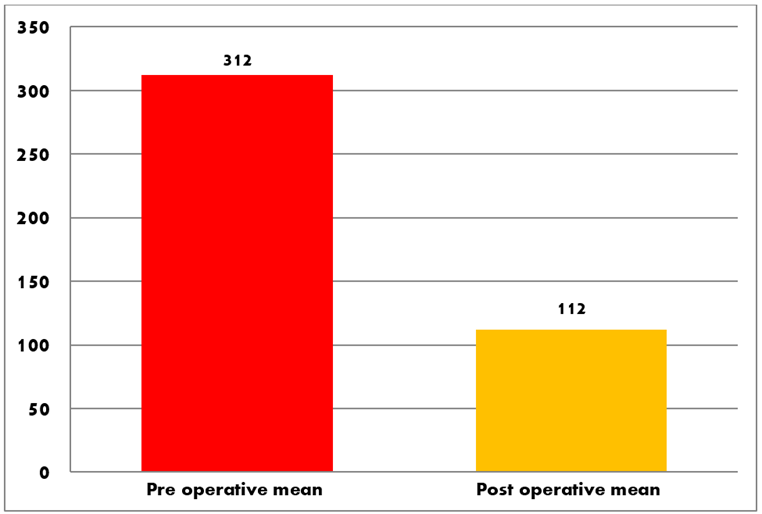
Figure 2: Comparing pre operative amylase with post procedure levels.
As mentioned earlier data from single stage procedure from our study is compared with data of the other stage procedure of two different studies which are Liu et al 2017 [6] and Rabago et al 2006 [7]. The following data were compared,
Table 3: Comparison of various variables of one stage vs two stage procedure.
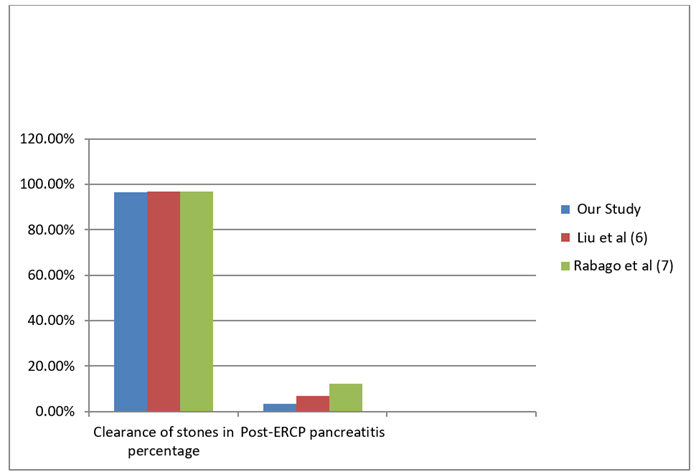
Figure 3: Comparision of CBD clearance and pancreatitis among various studies.
The above data clearly showed the advantages of a single session approach compared to the interval approach in terms of statistically significant reduction in total duration of surgery [8]. Patients also required less hospital stay [10,14] without compromise in clearance of stones or incidence of pancreatitis [4,9]. Though the incidence of pancreatitis post procedure is not statistically significant, yet the percentage of patients landing with post-ERCP hyper-amylasemia in a single-stage approach is less when compared to two-stage procedures [9,11]. Tackling both bile duct stones and gall bladder stones in a single sitting has decreased the need for repeat radiology for the patients, as in Bahtiyar Muhammedoğlu et al [11]. In our study, only 7 patients out of 58 required repeat radiological evaluation, which constitutes around 12 %. Whereas in two-stage procedures, patients will be invariably subjected to repeat radiology to know the current status of the CBD before proceeding with definitive lap. cholecystectomy, which is avoided in case of single-stage procedures [22].
Though not directly compared, it is proven from various studies that iERCP +LC has an overall lesser cost compared to conventional staged procedures [12]. The fact that the need for fewer scans, single surgery, and fewer hospital days are factors that contribute to overall lower cost. The same was also studied and published in Maris Jones et al [13], in which the mean total hospital charge in the one-step group was $58,145.00 and $78,895.00 in the two-step group (p = 0.033). We had zero mortality, and morbidity rates were comparable or less compared to two-stage procedures.
Discussion
Currently, the management of obstructive jaundice remains an ongoing topic of debate in the literature. Today, single-session ERCP and LC is a safe and feasible method performed based on studies cited in the literature [13]. Initially, single-stage procedures were done by combined surgeons and gastroenterologists [16,17], but in our it was a single surgeon doing both laparoscopic cholecystectomy and ERCP. This further emphasises the importance of endoscopic training as a part of curriculum for surgeons, as we witness there is an ongoing shift from minimally invasive surgery to endo-surgery in the coming decades [18].
Results of our showed single stage procedure has various advantages when compared to two stage surgery in terms of less hospital stay (mean 3.34 days, P value <0.001) [19], less duration of surgery (mean value 85 minutes, p value <0.001), less incidence of Post ERCP pancreatitis (3.34%, p value 0.131), a smaller number of repeat scans, single anesthesia, overall reduced cost to the patient.
In a single-stage procedure, above mentioned advantages were achieved without compromise in key factors, which is evident from statistically significant reduction in serum bilirubin and amylase levels (p value <0.001), stone clearance rates of 96.5 and higher in certain studies like Lella et al [20]
From above above-concluded data, it can be safely said that single-stage management of concomitant Gall bladder and common bile duct stones is safe and feasible when expertise and resources are available. Several studies have also concluded the same results and showed the superiority of a single-stage procedure over a two-stage procedure [15]. Less incidence of post-ERCP pancreatitis when the single session policy was adopted.
Besides the biochemical and surgical outcomes, patients undergoing a single-stage procedure had an overall good compliance and happiness compared to the two-stage group, as posited by Del Rio et al [21]. When a single surgeon does both procedures, as in our study, the follow-up and communication with patients becomes less hustle and easier. Doing laparoscopic cholecystectomy first, followed by ERCP, as in our centre, we also noted additional advantages like less bowel distension and an easier and safer laparoscopic procedure. Since we do ERCP second, any accidental slippage of microlithiasis or sludge during traction in LC can be tackled during ERCP, giving a complete CBD clearance rather than ERCP followed by cholecystectomy, where there is a theoretical possibility of accidental stone slippage.
Conclusion
Single session ERCP + laparoscopic cholecystectomy has proven its superiority over conventional staged procedures time and again. Under careful selection of patients, iERCP+LC is a safe and sound option in a select subset of patients. Our study further proves the same and emphasises that single-stage is feasible, safe, and should be practiced when expertise and equipment are available. We further emphasise that Endoscopy training for surgeons is a necessity rather than a luxury in the coming years.
References
- Nie S, Fu S, Fang K. Comparison of one-stage treatment versus two-stage treatment for the management of patients with common bile duct stones: A meta-analysis. Front Surg, 2023; 10: 1124955. doi: 10.3389/fsurg.2023.1124955.
- Jones M, Johnson M, Samourjian E, Schlauch K, Ozobia N. ERCP and laparoscopic cholecystectomy in a combined (one-step) procedure: a random comparison to the standard (two-step) procedure. Surg Endosc, 2013; 27(6): 1907-1913. doi: 10.1007/s00464-012-2647-z.
- Song ME, Chung MJ, Lee DJ, Oh TG, Park JY, Bang S, et al. Cholecystectomy for Prevention of Recurrence after Endoscopic Clearance of Bile Duct Stones in Korea. Yonsei Med J, 2016; 57(1): 132-137. doi: 10.3349/ymj.2016.57.1.132.
- Nie S, Fu S, Fang K. Comparison of one-stage treatment versus two-stage treatment for the management of patients with common bile duct stones: A meta-analysis. Front Surg, 2023; 10: 1124955. doi: 10.3389/fsurg.2023.1124955.
- Rodriguez Gatta D, Huidobro L, Petermann-Rocha F, Van de Wyngard V, Godoy F, Cid V, et al. Sex disparities in gallstone disease: insights from the MAUCO prospective population-based cohort study. BMJ Open Gastroenterol, 2024; 11(1): e001457. doi: 10.1136/bmjgast-2024-001457.
- Liu Z, Zhang L, Liu Y, Gu Y, Sun T. Efficiency and Safety of One-Step Procedure Combined Laparoscopic Cholecystectomy and Eretrograde Cholangiopancreatography for Treatment of Cholecysto-Choledocholithiasis: A Randomized Controlled Trial. The American SurgeonTM, 2017; 83(11): 1263-1267. doi:10.1177/000313481708301129.
- Rábago LR, C Vicente, F Soler, M Delgado, I Moral, Guerra I, et al. Two-stage treatment with preoperative endoscopic retrograde cholangiopancreatography (ERCP) compared with single-stage treatment with intraoperative ERCP for patients with symptomatic cholelithiasis with possible choledocholithiasis. Endoscopy, 2006; 38: 779–786. doi: 10.1055/s-2006-944617.
- Lella F, Bagnolo F, Rebuffat C, Scalambra M, Bonassi U, Colombo E. Use of the laparoscopic-endoscopic approach, the so-called ‘‘rendezvous’’ technique,in cholecystocholedocholithiasis: a valid method in cases with patient-related risk factors for post-ERCP pancreatitis. Surg Endosc, 2006; 20: 419–423. doi: 10.1007/s00464-005- 0356-6.
- Sahoo M, Pattnaik A, Kumar A. Randomized study on single stage laparo endoscopic rendezvous (intraoperative ERCP) procedure versus two stage approach (preoperative ERCP followed by laparoscopic cholecystectomy) for the management of cholelithiasis with choledocholithiasis. J Minim Access Surg, 2014; 10: 139–143. doi: 10. 4103/0972-9941.134877.
- Mallick R, Rank K, Ronstrom C, Amateau SK, Arain M, Attam R, et al. Single-session laparoscopic cholecystectomy and ERCP: a valid option for the management of choledocholithiasis. Gastrointest Endosc, 2016; 84(4): 639-645. doi: 10.1016/j.gie.2016.02.050.
- Muhammedoğlu B. Single-stage treatment with ERCP and laparoscopic cholecystectomy versus two-stage treatment with ERCP followed by laparoscopic cholecystectomy within six to eight weeks: a retrospective study. Turk J Surg, 2019; 35(3): 178-184. doi: 10.5152/turkjsurg.2018.4204.
- Bansal VK, Misra MC, Rajan K, Kilambi R, Kumar S, Krishna A, et al. Single-stage laparoscopic common bile duct exploration and cholecystectomy versus two-stage endoscopic stone extraction followed by laparoscopic cholecystectomy for patients with concomitant gallbladder stones and common bile duct stones: a randomized controlled trial. Surg Endosc, 2014; 28: 875–885. doi: 10.1007/s00464-013-3237-4.
- Jones M, Johnson M, Samourjian E, Schlauch K, Ozobia N. ERCP and laparoscopic cholecystectomy in a combined (one-step) procedure: a random comparison to the standard (two-step) procedure. Surg Endosc, 2013; 27(6): 1907-1912. doi: 10.1007/s00464-012-2647-z.
- Tzovaras G, Baloyiannis I, Kapsoritakis A, Psychos A, Paroutoglou G, Potamianos S. Laparoendoscopic rendezvous: an effective alternative to a failed preoperative ERCP in patients with cholecystocholedocholithiasis. Surg Endosc, 2010; 24(10): 2603–2606. doi: 10.1007/s00464-010-1015-0.
- Wright BE, Freeman ML, Cumming JK, Quickel RR, Mandal AK. Current management of common bile ductstones: Is there a role for laparoscopic cholecystectomy and intraoperative endoscopic retrograde cholangiopancreatography as a single-stage procedure. Surgery, 2002; 132: 729–737. doi: 10.1067/msy.2002.127671.
- La Greca G, Barbagallo F, Di Blasi M, Chisari A, Lombardo R, Bonaccorso R, et al. Laparo-endoscopic “rendezvous” to treat cholecysto-choledocolithiasis: effective, safe and simplifies the endoscopist’s work. World J Gastroenterol, 2008; 14(18): 2844–2850. doi: 10.3748/wjg.14.2844.
- Enochsson L, Lindberg B, Swahn F, Arnelo U. Intraoperative endoscopic retrograde cholangiopancreatography (ERCP) to remove common bile duct stones during routine laparoscopic cholecystectomy does not prolong hospitalization: a 2-year experience. Surg Endosc, 2004; 18(3): 367–371. doi: 10.1007/s00464-003-9021-0.
- Singh SS, Shinde RK. Minimally Invasive Gastrointestinal Surgery: A Review. Cureus, 2023; 15(11): e48864. doi: 10.7759/cureus.48864.
- Morino M, Baracchi F, Miglietta C, Furlan N, Ragona R, Garbarini A. Preoperative endoscopic sphincterotomy versus laparoendoscopic rendezvous in patients with gallbladder and bile duct stones. Ann Surg, 2006; 244(6): 889–893. doi: 10.1097/01.sla.0000246913.74870.fc
- Lella F, Bagnolo F, Rebuffat C, Scalambra M, Bonassi U, Colombo E. Use of the laparoscopic–endoscopic approach, the so-called “rendezvous” technique, in cholecystocholedocholithiasis: a valid method in cases with patient-related risk factors for post-ERCP pancreatitis. Surg Endosc, 2006; 20(3): 419–423. doi: 10.1007/s00464-005-0356-6.
- Del Rio P, Dell’Abate P, Labonia D, Negri M, Sianesi N, Arcuri MF, et al. Choledocholithiasis and endo-laparoscopic rendezvous. Analysis of 59 consecutive cases. Ann Ital Chir, 2011; 82(3): 221–224.
- Gerosa Martino, Guttadauro Angelo, Stillittano Domenico, Sassun Richard, Sileo Annaclara, Vignati Barbara, et al. Single stage laparoscopic cholecystectomy with intraoperative endoscopic retrograde cholangiopancreatography for cholecysto-choledocholithiasis. Lesson learnt from the COVID-19 pandemic. Frontiers in Surgery, 2024; 11: 1398854. 10.3389/fsurg.2024.1398854.

