Prescribing Trends Of ACE-Inhibitors Post-MI In Chaudhary Pervaiz Elahi Institute of Cardiology, Wazirabad
Fahad Akbar1, Aqna Malik1,2,*, Muhammad Farhan Azam1, Waleed Awais2, Muhammad Asad Ali2, Noor Fatima2, Swera Noor2, Aden Fatima2 and Faiza Batool2
1Department of Pharmacy, University of Chenab, Gujrat
2Department of Pharmacy, University of Lahore, Lahore
Received Date: 12/03/2025; Published Date: 16/04/2025
*Corresponding author: Dr. Aqna Malik, Department of Pharmacy, University of Chenab, Gujrat; Department of Pharmacy, University of Lahore, Lahore.
ORCID: https://orcid.org/0000-0003-3875-9621
Introduction
Myocardial Infarction (MI), commonly referred to as a "heart attack," occurs due to a reduction or total obstruction of blood supply to the heart.MI may occur asymptomatically and remain unrecognized, or it can manifest as a catastrophic event resulting in abrupt mortality [1]. The majority of MIs result from preexisting coronary artery disease. Coronary artery obstruction results in myocardial oxygen deprivation, might result in myocardial cell death and necrosis. Patients may exhibit chest discomfort or pain that radiates to the neck, jaw, shoulder, or arm (Brown & Hamilton, 2014). The standard range for Troponin I levels is often under 0.04 ng/mL. During heart attack post MI Troponin, I level increase markedly, within 12-24 hours and remaining elevated for many days. A result of 0.5 ng/mL or higher signifies MI, with escalating values correlating with the extent of myocardial damage (Mebazaa et al., 2018). The ESC Guidelines for managing acute MI with ST segment advocate for immediate ECG evaluation to verify ST-segment elevation, succeeded by swift reperfusion therapy, ideally primary PCI, if accessible within 120 minutes, or fibrinolysis if not (Brown & Hamilton, 2014). Adjunctive therapy such as antiplatelet medicines, anticoagulants, beta-blockers, ACE inhibitors, and statins are crucial for enhancing results. The ACC/AHA Guidelines recommended aspirin, P2Y12 inhibitors, and adjuvant medications such as beta-blockers and ACE inhibitors early, with oxygen therapy provided only when clinically necessary, for the Management of patients with (STEMI) [2]. The prompt introduction of ACE inhibitors within 24 hours and ARBs within 7 days enhances outcomes. Moreover, the early administration of β -blockers (<24 hours) in MI is associated with persistent HF and can increase the risk of cardiogenic shock [3]. The ACC/AHA Guidelines recommend SGLT-2 inhibitors (SGLT2i) to treat symptomatic HF which may be associated with Reduced Ejection Fraction (HFrEF), the guidelines also endorse a combination of four agents: ARNIs, ACE inhibitors, beta-blockers, and MRAs.
ACE inhibitors are indicated for uncomplicated HTN or HTN associated with concurrent coronary artery disease (including post-MI), and HF with low ejection fraction [4]. A comparison of the efficacy of Angiotensin Receptor-Neprilysin Inhibitor (ARNI) therapy versus (ACEI/ARB) therapy for cardiovascular outcomes in AMI patients indicated that ARNIs are more effective than ACEI/ARB in diminishing long-term adverse cardiovascular outcomes, especially in patients with (LVEF) ≤40% and those aged ≤60 years [5]. The prompt initiation of ACE inhibitors within 24 hours following an MI has been linked to a lowered risk of cardiac rupture. This underscores the significance of the prompt start of ACE inhibitors in alleviating severe consequences and enhancing patient outcomes post-MI. The utilization of ACE inhibitors post-myocardial infarction in individuals with ischemic heart disease was minimal, at merely 27.97%, suggesting incorrect prescribing practices as per the study (Li et al., 2023). Post-MI prescribing trends differ between ACEIs and ARBs. ACEIs are the primary choice; however, ARBs are utilized in cases of intolerance. Selection must take into account patient variables, rather than solely tolerability (Winkelmayer et al., 2006).
Many researchers found in their research that ARNI dramatically decreased all-cause mortality in heart failure with reduced or mildly impaired ejection fraction compared to ACE inhibitors/angiotensin receptor blockers (Kuchulakanti, 2020, Fu et al., 2023).
Despite a lot of advancements in acute management and treatment options, Myocardial Infarction (MI) remains a leading cause of co-morbidities and death worldwide. (ACEI) have been used in treatment regimens post-cardiac attack and have proven to reduce mortality and improve outcomes. However, discrepancies exist in the prescribing trends of ACEI post-MI, raising concerns about adherence to guidelines and potential gaps in optimal patient care. This study seeks to examine the current prescribing patterns of ACEI in post-MI patients, identify factors influencing their utilization, and assess adherence to guideline recommendations, aiming to provide insights into opportunities for improving clinical practice and patient outcomes (Sachdeva et al., 2023).
Aim:
A clinical study was aimed to check the prescribing trends of ACEI drugs in post-MI patients in Chaudhary Pervaiz Elahi Institute of Cardiology, Wazirabad.
Objective:
- To understand the purpose of prescribing ACE Inhibitors to patients post Mi and to check the use of β blockers in Conjunction with ACE Inhibitors.
- ACEI/ARB use within 24h of admission for AMI patients with SBP <100mmHg undergoing PCI was associated with reduced in-hospital major adverse cardiac events.
Material and Methodology
The study was conducted at the Chaudhary Pervaiz Elahi Institute of Cardiology, Wazirabad from October 2023 to April 2024 in which a mixed-methods approach was employed, combining descriptive cross-sectional studies with retrospective analysis of patient records. The study was approved by the IRB committee of the University of Chenab. The primary source for data was prescriptions and laboratory test results. Prior written approval was obtained from the Head of the cardiac department of Hospital administration. The sample size was calculated via the Raosoft Sample Size Calculator with a CI of 95% and a margin of error of 5%. Initially, 100 patients were recruited for the study, however later on 17 out of the total 100 didn’t give consent. Finally, 83 cardiac patients were selected for the study. Non-probability convenience sampling technique was applied. Prescription data of patients was noted for analysis including demographics, medical records, and medication prescribed and administered from departments like Emergency, Critical care units, and General ward. Lab reports were also collected from the respective patients to check cardiac enzyme levels of troponin I. Lab records of diagnostic tests like ECG and ECHO were noted. echocardiogram. Stringent measures were followed to ensure the secure handling and anonymization of all collected information. Patients diagnosed with ACS, confirmed by clinical symptoms, ECG changes, and/or cardiac enzyme elevation and admitted to the cardiac ward of Chaudhary Pervaiz Elahi Institute of Cardiology, Wazirabad were included in the study, and patients with conditions other than cardiac disease or incomplete medical records were excluded.
Results
Among 83 patients, 36 females and 47 males were selected for the study. 36 females were classified as HFrEF patients as per guidelines of heart failure classifications established by the European Society. HFrEF was categorized according to The European Society of Cardiology. The risk of HF with preserved and reduced LvEF and HvEF among participants was assessed from MR file data. Data was tabulated according to the age group of both males and females. Among 83 patients most were suffering from HFpEF (males 5±3.03 and females 4.2±4.5) (Tables 1,2).
LVEF is a strong predictor of CVS outcomes in HF patients. However, when EF reaches the range of 55%, it stops adding to the evaluation of CVS risk for HF [6]. HF patients with midrange and reduced LVEF are at great risk of mortality. It is the most widely used clinical measure of left ventricular systolic function.
Mostly (males 3±1.63) who had a past medical history of heart damage from heart attack or cardiomyopathy were diagnosed with (HFrEF).
MR data showed that all selected patients with HFmrEF were prescribed cardiac drugs. Among the total participants, 21(25.3012%) males & 13(15.6%) females were accurately prescribed ACEi, and ARBs. Moreover, indicated rational prescribing while 23 (11.5±0.5%) including 12 (14.5%) males and 11 (13.3) females were not prescribed any cardiac drug despite worsening conditions highlighted by irrational prescribing. (Table 3). Overall rational practice was observed in 60±5 participants patients and irrational practise was observed in 23±0.5 patients.
Increased troponin level is a significant indicator of mortality in patients with acute coronary syndrome, particularly when accompanied by a dynamic change. In the current study, ACS Patients with increased troponin I levels than baseline were more susceptible to acute Myocardial Infarction (MI), early mortality, and adverse discharge outcomes in comparison to those with low or normal troponin I levels [7].
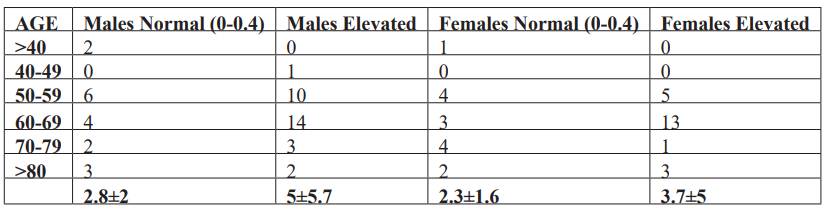
Results depicted that male (5±5.7) have greater troponin levels than females (3.7±5). Troponin testing is mandatory in AIC Patients with a history of pulmonary embolism. Moreover, increased troponin I levels may indicate hemodynamic instability and aortic dissection. Myocardial damage chronic atherosclerotic CVD, chronic coronary syndrome, chronic ischemia of the lower extremities, or CVD. In the present study, MR file records showed patients with increased troponin levels suffered from different cardiac ailments, though not mentioned individually.
Increased cardiac troponin concentration correlates with certain parameters suggesting subclinical dysfunction of the CVS including the IMT, ABI, CAC, PWV, and FMDc [8]. Survey results showed that all patients with high troponin I were administered cardiac drugs primarily comprising Dual Antiplatelet Therapy (DAPT). Some patients were treated with enoxaparin in the CCU. Moreover, patients with heart failure, whether post-myocardial infarction or not, were prescribed ACEIs or ARBs. Only patients with Heart failure either after a heart attack or without it were prescribed ACEi or ARBs.
Table 1: Cardiology classification of HF wrt to LVEF.
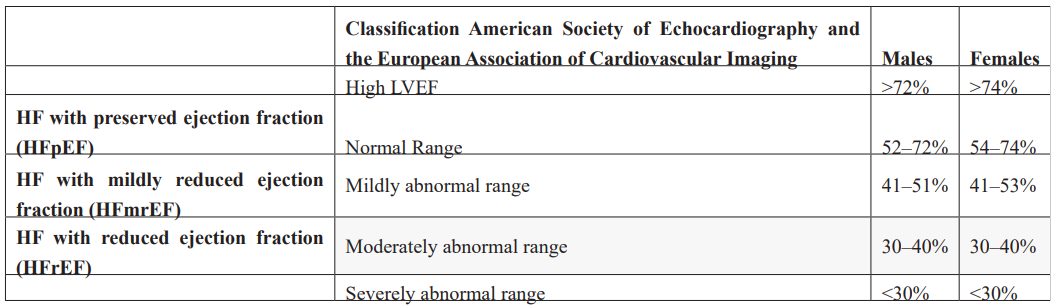
Table 2: Risk of HF with LVEF among Female and male patients.
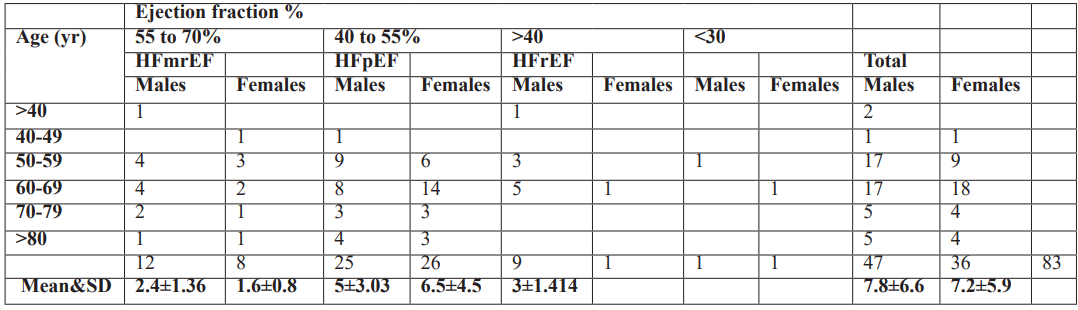
Table 3: Prescribing pattern among HF patients with LVEF.
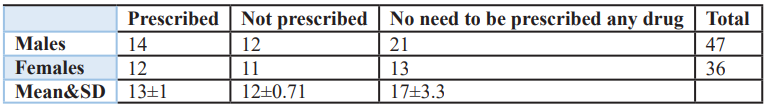
Table 4: Rational VS Irrational Prescribing.
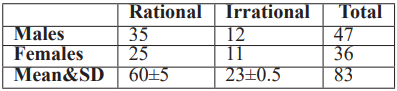
Table 5: Troponin levels among patients.
Discussion
Male patients are more prone to MI than women while women have a high chance of developing HF. All the patients with MI were treated according to the guidelines established indicating complete rational prescribing in Chaudhry Pervaiz Elahi Institute of Cardiology but the study indicates significant disparity in adherence to established guidelines in case of HF as only half of patients are being treated according to recommended protocols.
Limitations
Some of the main limitations of this study are
- Small sample size (n=83) due to a shortage of time
- Lack of resources like a small number of equipment and shortage of medicines
- Overflow of patients with other Conditions like CHB etc
Recommendations
- Availability of all the necessary equipment in sufficient quantity and a full supply of medicines must be ensured.
- Large-scale studies must be conducted to check adherence to the guidelines to provide optimum healthcare.
References
- Thygesen K, Alpert JS, White HD, Jaffe AS, Apple FS, Galvani M, et al. Universal definition of myocardial infarction. Circulation, 2007; 116(22): 2634-2653. https://doi.org/10.1161/circulationaha.107.187397
- Man JP, Tymchak WJ, Jugdutt BI. Therapies Adjunctive 13. Cardiac Intensive Care E-Book, 2010; 145.
- Sinha SS, Rosner CM, Tehrani BN, Maini A, Truesdell AG, Lee SB, et al. Cardiogenic shock from heart failure versus acute myocardial infarction: clinical characteristics, hospital course, and 1-year outcomes. Circulation: Heart Failure, 2022; 15(6): e009279.
- Sindone AP, De Pasquale C, Amerena J, Burdeniuk C, Chan A, Coats A, et al. Consensus statement on the current pharmacological prevention and management of heart failure. Med J Aust, 2022; 217(4): 212-217. https://doi.org/10.5694/mja2.51656
- Greenberg B. Angiotensin receptor-neprilysin inhibition (ARNI) in heart failure. International Journal of Heart Failure, 2020; 2(2): 73.
- Ceriello A, Catrinoiu D, Chandramouli C, Cosentino F, Dombrowsky AC, Itzhak B, et al. Heart failure in type 2 diabetes: current perspectives on screening, diagnosis and management. Cardiovascular diabetology, 2021; 20(1): 218.
- Akbas T. Elevated Cardiac Troponin Levels as a Predictor of Increased Mortality Risk in Non-Cardiac Critically Ill Patients Admitted to a Medical Intensive Care Unit. J Clin Med, 2024; 13(20). https://doi.org/10.3390/jcm13206025.
- Jakubiak GK. Cardiac Troponin Serum Concentration Measurement Is Useful Not Only in the Diagnosis of Acute Cardiovascular Events. J Pers Med, 2024; 14(3). https://doi.org/10.3390/jpm14030230.

