Simplified Technique for Localizing the Fossa Ovalis in Transseptal Puncture using Right Atrial Septogram
Sadanand Reddy Tummala, Paladugu Srinivas Gautam, Uma Devi Karuru*, Naveen T, Sai Kumar Mysore, Ashirbad Parhi and Kiran Kumar Kanjerla
Department of Cardiology, ESIC Medical college and Super Speciality Hospital, Hyderabad, Telangana, India
Received Date: 27/02/2025; Published Date: 02/04/2025
*Corresponding author: Dr. Uma Devi Karuru, Assistant Professor, Department of Cardiology, ESIC Medical college and Super Speciality Hospital, Hyderabad, Telangana, India
Abstract
Background: Transseptal catheterization is an essential procedure for left-sided heart interventions, commonly used in percutaneous transluminal mitral commissurotomy, electrophysiology studies, catheter ablations, and device placements. The key to successful transeptal puncture is the accurate identification of the fossa ovalis on the Interatrial Septum (IAS), which serves as the optimal access point. While traditional imaging methods like Transoesophageal Echocardiography (TEE) and three-dimensional fluoroscopy offer accurate anatomical visualization, these techniques can be costly and require specialized equipment. Therefore, a simplified, cost-effective method to accurately localize the IAS is highly beneficial for improving procedural outcomes and making the technique accessible in various clinical settings.
Method: We describe a novel technique for locating the IAS using a combination of 2-dimensional echocardiography and fluoroscopy. First, the operator performs a 2D echocardiogram to estimate the cardiac axis and rotation, with specific focus on the position of the cardiac apex. This allows for an initial evaluation of IAS anatomy and fluoroscopic projection. A Right Atrial (RA) septogram is then obtained by performing a fluoroscopic procedure using a 20°-25° RAO view and a 10°-15° caudal tilt. The septogram is used to identify the rectangular shape of the IAS, and imaginary lines are drawn to divide it into four quadrants. The optimal puncture site is located at the posterior quadrant, slightly closer to the right atrial posterior margin. The sheath and needle orientation are confirmed in a 30° LAO fluoroscopic view. After confirming the puncture site, a Brocken Brough needle is advanced to access the left atrium, with blood aspiration confirming correct placement.
Conclusion: This simplified, cost-effective technique for identifying the optimal puncture site on the IAS improves the safety and precision of transseptal catheterization. By using accessible imaging techniques, the method is suitable for a wide range of clinical settings and provides an alternative to expensive imaging technologies, enhancing both procedural success and safety for patients.
Keywords: Fossa Ovalis, Transseptal puncture, Right Atrial Septogram
Introduction
Transseptal catheterization is a critical procedure in various cardiac interventions, including left-sided heart access, electrophysiological studies, and the placement of left atrial devices, such as in patients undergoing catheter ablation for atrial fibrillation [1,2]. The procedure was first performed by Braun Wald, Ross and Morrow and later refined by Brocken Brough and Mullins, whose names have been intricately linked with this procedure [1-3]. The safety and success of this procedure rely heavily on accurately identifying the optimal puncture site on the Interatrial Septum (IAS), specifically targeting the fossa ovalis, a natural opening in the septum. However, achieving precise localization remains challenging due to individual anatomical variations and the technical complexity of the procedure.
In traditional techniques, advanced imaging modalities, such as Transoesophageal Echocardiography (TEE), Intracardiac Echocardiography (ICE) or three-dimensional fluoroscopy, are often employed to guide the transeptal puncture [4-13]. While these methods can provide accurate anatomical views, they often require specialized equipment and expertise, which can lead to increased procedural costs and complexity. Furthermore, they may not always be readily available in all clinical settings, particularly in emergency or resource-limited environments.
The objective of this manuscript is to present a simplified, cost-effective technique for determining the appropriate site for transeptal puncture on the IAS, leveraging 2-dimensional echocardiography and fluoroscopic guidance. This method aims to reduce the dependence on expensive imaging technologies, while maintaining high levels of accuracy in identifying the puncture site. The technique described here allows for systematic localization of the IAS, with clear demarcation of key anatomical landmarks, ensuring precise access to the left atrium while minimizing the risk of complications.
By utilizing routine imaging modalities and clear procedural steps, this method offers an accessible and efficient alternative for both novice and experienced operators. The simplicity of this technique makes it particularly relevant for a broad spectrum of clinical environments, improving safety and success rates in transeptal catheterization, especially where advanced resources are limited or unavailable.
Methodology
The technique described below outlines a systematic and precise approach for performing a transeptal puncture using echocardiography and fluoroscopy for accurate localisation of the puncture site on the inter atrial septum (IAS). The key steps of the methodology, focusing on the rationale, instruments, and detailed procedure are summarised below.
- Initial Echocardiographic Assessment
- Objective: Ensure there is no significant cardiac rotation that could affect IAS alignment.
- Process: The patient undergoes a routine 2D echocardiogram. This assessment checks for the correct orientation of the heart within the thoracic cavity, ensuring the apex is between 20° and 60° to the left of the midline. This orientation helps the IAS appear which is usually in the sagittal plane, with anterior border rotated to the left along the vertical axis, with posterior border closer to the spine, and the anterior border to the left of and behind the sternum anteriorly.
- Fluoroscopic Positioning and Septogram Acquisition
- Objective: Obtain a detailed view of the IAS to visualize its borders and the fossa ovalis.
- Process: Following the echocardiogram, the operator uses fluoroscopy with a C-arm setup. The goal is to obtain an atrial septogram. By injecting radiocontrast into the right atrial cavity, the septum is visualized in an en face view from the right side, showing all four borders and all four corners of the IAS clearly.
- Fluoroscopic Angulation: A 20°-25° right anterior oblique (RAO) view, with a 10°-15° caudal tilt, is used to obtain the optimal septogram view. This orientation ensures visualization of the septum in the en face view with all key borders (tricuspid annulus, aortic root, right atrial appendage, SVC, IVC, and posterior IAS).
- Defining the Quadrants of the IAS
- Objective: Divide the IAS into quadrants to accurately locate the fossa ovalis and define the puncture site.
- Process:
- The fossa part of interatrial septum (true septum) is located approximately equi-distant from all the borders although slightly closer to the anterior border.
- Draw a horizontal line from the posterior to the anterior margin of the right atrial septum.
- A vertical line is then drawn at the midpoint of the horizontal line.
- This divides the IAS into four quadrants: anterosuperior, anteroinferior, posteroinferior, and posterosuperior (Figure 1).
- The fossa ovalis, the target for the transeptal puncture, is typically located near the center of the IAS but slightly closer to the posterior part of the septum.
- Fluoroscopic Left Anterior Oblique (LAO) Projection
- Objective: Confirm the exact orientation of the puncture device and the location of the puncture site.
- Process:
- The tip of Mullins sheath is positioned at the anterosuperior corner of the posteroinferior quadrant in contact with septum (Figure 2).
- The position of Mullins sheath loaded with transeptal needle pointing to the septum is verified in fluoroscopic LAO view (Figure 3).
- In this view, the Mullins sheath loaded with transeptal needle pointing towards the spine confirms the appropriate position of the transeptal needle.
- The Mullins sheath is tugged against the septum and puncture needle advanced across the septum into the left atrium.
- In this view, the sheath tip should be directed toward the IAS, with the puncture site positioned approximately 3-4 mm inside the anterosuperior corner of the posteroinferior quadrant.
- This fluoroscopic projection ensures proper alignment of the sheath and needle, allowing precise placement for puncture.
- Wire Positioning and Confirmation
- Objective: Confirm that the transeptal needle has entered the left atrium (LA) and ensure safety before advancing further.
- Process:
- After advancing the Brocken Brough needle through the septum, the operator aspirates blood to confirm entry into the LA which yields bright red oxygenated blood.
- The Brocken Brough needle is then exchanged for a soft-tipped LA coil wire (Figure 4).
- The position of the wire is confirmed using either transthoracic echocardiography or fluoroscopic LAO projection, ensuring it is properly positioned in the LA.
- Sheath Advancement
- Objective: Facilitate smooth catheterization and final placement of the transeptal sheath.
- Process:
- After confirming proper wire placement, the sheath is advanced over the wire into the left atrium.
- The transeptal puncture is performed with the sheath, allowing for subsequent catheterization and procedure progression.
Rationale for the Approach:
- Echocardiography helps identify and confirm the heart's rotation and positioning, ensuring that the IAS is visualized correctly.
- Fluoroscopy, combined with contrast injection, provides a clear en face view of the septum, ensuring that all key borders are identified for accurate targeting of the fossa ovalis.
- Quadrant Division aids in pinpointing the ideal puncture site, reducing the risk of complications.
- The use of both fluoroscopy and echocardiography for wire positioning and confirmation ensures precise navigation and safety during the procedure.
- Sheath advancement with a wire in place ensures smooth and safe passage into the left atrium, reducing procedural risks.
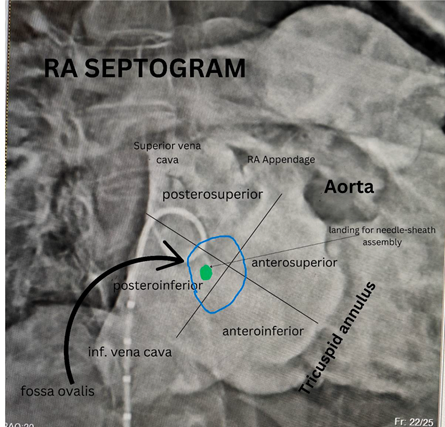
Figure 1: Fluoroscopic image of right atrium with division of the interatrial septum into quadrants.

Figure 2: Fluoroscopic image showing the direction of Brocken Brough needle for septal puncture in right anterior oblique view.
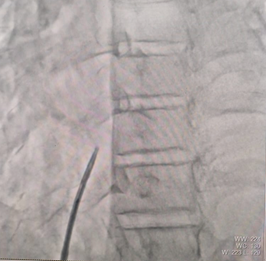
Figure 3: Fluoroscopic image showing the direction of Brocken Brough needle for septal puncture in left anterior oblique view.

Figure 4: Fluoroscopic image showing the passage of left atrial coil wire through Mullins Sheath into the left atrium.
Discussion
This simplified technique for localizing the puncture site on the interatrial septum (IAS) during transseptal catheterization offers a valuable alternative to traditional, resource-intensive methods. By combining standard 2D echocardiography with fluoroscopy, the procedure not only improves accessibility and reduces costs but also maintains the accuracy required for a safe and successful puncture. Below, we explore the key advantages and clinical implications of this approach in detail:
- Reduced Complexity and Cost
One of the most significant benefits of this technique is its simplicity and cost-effectiveness. Traditional methods often rely on advanced imaging technologies such as transoesophageal echocardiography (TEE), Intracardiac Echocardiography (ICE), or 3D fluoroscopy, which can be prohibitively expensive and require specialized equipment and expertise. These imaging modalities, while effective, may not always be readily available, particularly in resource-limited settings or emergency situations.
By utilizing routine 2D echocardiography and fluoroscopy, this approach significantly lowers the financial burden while ensuring high procedural accuracy. Furthermore, the reliance on widely available and easily interpretable imaging techniques enhances its utility in various clinical environments, making it accessible to a broader range of healthcare providers. This is particularly important in developing regions or hospitals with limited access to high-end imaging systems, where the availability of safe and cost-effective methods is essential for improving patient outcomes.
- Anatomical Precision and Improved Safety
Achieving precise localization of the fossa ovalis is critical for the safe performance of transseptal catheterization. An inaccurate puncture site can lead to severe complications, such as perforation of adjacent structures, including the aortic root, superior vena cava (SVC), inferior vena cava (IVC), or right atrial appendage. The technique outlined here provides a systematic approach to accurately identifying the optimal puncture site, significantly minimizing the risks associated with misplaced punctures.
By dividing the IAS into four quadrants, this technique ensures that the puncture site is chosen with high precision, reducing the chances of inadvertent damage to neighbouring structures. The posterior quadrant, where the fossa ovalis is typically located, serves as the target, and the systematization of this process allows for reliable outcomes across different patient anatomies. The division of the septum into quadrants also provides an added layer of clarity, improving the operator’s confidence and reducing the potential for errors.
- Fluoroscopic Guidance and Device Alignment
The use of fluoroscopic guidance in both Right Anterior Oblique (RAO) and Left Anterior Oblique (LAO) projections ensures the precise alignment of the puncture device with the target site. The RAO view provides an enface view of the IAS, facilitating accurate identification of the anatomical borders, such as the tricuspid annulus and the aortic root. The LAO view is particularly useful for confirming the optimal orientation of the puncture device and sheath, ensuring that the needle is correctly aligned with the IAS before advancement. This dual-projection approach is key to enhancing both the safety and accuracy of the procedure.
Real-time feedback provided by fluoroscopy during the procedure is invaluable in minimizing the risk of device misalignment, which can otherwise lead to complications such as inadvertent puncture of the atrial wall or damage to other structures. With both RAO and LAO projections working in tandem, the operator can confidently navigate the catheter or needle toward the desired puncture point, ensuring a more predictable and successful outcome.
- Minimization of Complications
Proper identification of the puncture site and correct needle placement are critical in minimizing complications, which can include perforation of the atrial wall, pericardial tamponade, or thromboembolic events. The inclusion of aspiration after the needle insertion further strengthens the safety of this technique. By aspirating blood, the operator can confirm the needle's correct placement within the Left Atrium (LA), offering an additional layer of verification before advancing the sheath and performing the catheterization.
The use of heparin following wire placement also contributes to the reduction of thromboembolic complications, ensuring that the risk of clot formation is minimized throughout the procedure. These precautionary measures add an extra layer of safety, promoting better patient outcomes and increasing the overall reliability of the method.
- Clinical Applicability in Resource-Limited Settings
Another key advantage of this technique is its suitability for use in diverse clinical environments, including those with limited access to advanced imaging equipment. The approach requires only basic echocardiography and fluoroscopy, both of which are standard in most interventional cardiology settings. This is particularly beneficial in emergency or resource-constrained situations, where access to high-end imaging modalities may be limited or unavailable.
The simplicity and low cost of the method make it an attractive option for institutions with budget constraints or for clinicians in developing regions who may not have access to more expensive equipment. Furthermore, because the technique relies on imaging modalities that are both widely available and relatively easy to perform, it allows for broader implementation and adoption, making transseptal catheterization safer and more feasible for a greater number of patients globally.
- Reproducibility and Operator Learning Curve
This technique’s reliance on basic 2D echocardiography and fluoroscopy ensures that it can be easily learned and performed by operators at various levels of experience. In comparison to more complex techniques requiring advanced imaging systems, this method can be adopted by both novice and experienced operators, providing a standardized approach that can lead to consistent procedural outcomes.
The simplicity of the approach ensures that it is reproducible, even in centers with less experienced staff or limited resources. By establishing clear procedural steps and utilizing widely available imaging techniques, operators can build confidence in performing transseptal puncture with a reduced risk of complications. The reduced complexity of the method also makes it easier to teach, ensuring that procedural safety is maintained even in training environments.
- Alignment with Current Literature
The advantages of using simple imaging techniques for transseptal puncture are well supported by current literature. Previous studies have emphasized the safety and efficacy of utilizing basic echocardiography and fluoroscopy for guiding transseptal puncture, with improved outcomes in both the accuracy of puncture site localization and the reduction of procedural complications [14-18]. Our findings align with these studies, further validating the approach’s effectiveness.
Additionally, research has shown that minimizing the use of complex imaging techniques not only reduces costs but also enhances procedural success rates by improving accessibility and making the procedure more widely applicable. This method, with its straightforward approach, ensures that patients benefit from accurate and safe transseptal puncture while minimizing the financial and logistical barriers that can exist with advanced imaging technologies.
Conclusion
In conclusion, the simplified technique for identifying the optimal puncture site on the interatrial septum during transseptal catheterization provides a reliable, cost-effective, and clinically applicable alternative to more complex imaging methods. By combining 2D echocardiography and fluoroscopy, the method ensures accurate localization, minimizes complications, and improves procedural safety. Furthermore, it enhances accessibility, making transseptal catheterization feasible and safe even in resource-limited settings. This approach has the potential to improve patient outcomes across a wide variety of clinical environments, particularly in cases where advanced imaging systems may not be available.
This method offers several key advantages over traditional techniques for transeptal puncture site localization, providing a balance of simplicity, cost-effectiveness, and high precision. The following points provide a detailed discussion of the rationale behind the steps, the advantages of this approach, and its clinical implications:
Limitations and Future Considerations
While this method provides a reliable and cost-effective means of localizing the puncture site, there are some limitations. The technique relies heavily on the operator's ability to interpret echocardiographic and fluoroscopic images accurately. Additionally, the approach may not be suitable for all patients, particularly those with significant anatomical variations that may require more advanced imaging techniques for precise localization.
Future studies should focus on evaluating the long-term outcomes of this technique compared to more traditional methods, particularly in terms of complication rates, procedural times, and patient safety. Further refinement of the method, potentially incorporating advanced imaging modalities like 3D echocardiography or CT imaging, could improve its precision and broaden its applicability in challenging cases.
Declarations:
Ethical approval and consent to participate: Approved by the institute ethical committee.
Consent to publish: Not applicable.
Availability of data and material: Not applicable
Competing interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author contribution:
SRT: Conceptualization; Methodology; Supervision; Writing—original draft; Writing—review and editing
PSG: Conceptualization; Methodology; Supervision; Writing—original draft; Writing—review and editing
UDK: Conceptualization; Methodology, Validation; Writing—original draft
NT: Writing—review and editing
SKM: Writing—review and editing
AP: Validation; Writing—review and editing
KKK: Valitation; Writing—review and editing
All authors reviewed the paper and approved the final version of the manuscript.
Acknowledgements: None
References
- Ross J Jr, Braunwald E, Morrow AG. Left heart catheterization by the transeptal route: a description of the technique and its applications. Circulation, 1960; 22: 927–934.
- Brockenbrough EC, Braunwald E, Ross J Jr. Transseptal left heart catheterization. A review of 450 studies and description of an improved technic. Circulation, 1962; 25: 15–21. doi: 10.1161/01.cir.25.1.15.
- Mullins CE. Transseptal left heart catheterization: experience with a new technique in 520 pediatric and adult patients. Pediatr Cardiol, 1983; 4: 239–245. doi: 10.1007/BF02242264.
- Matoshvili Z, Bastani H, Bourke T, et al. Safety of fluoroscopy‐guided transseptal approach for ablation of left‐sided arrhythmias. EP Europace, 2017; 19(12): 2023‐2026.
- Ballal RS, Mahan EF, Nanda NC, Dean LS. Utility of transesophageal echocardiography in interatrial septal puncture during percutaneous mitral balloon commissurotomy. Am J Cardiol, 1990; 66(2): 230‐232.
- Kronzon I, Glassman E, Cohen M, Winer H. Use of two‐dimensional echocardiography during transseptal cardiac catheterization. J Am Coll Cardiol, 1984; 4(2): 425‐428.
- Epstein LM, Smith T, HOFF HT. Nonfluoroscopic transseptal catheterization: safety and efficacy of intracardiac echocardiographic guidance. J Cardiovasc Electrophysiol, 1998; 9(6): 625‐630.
- Bulava A, Hanis J, Eisenberger M. Catheter ablation of atrial fibrillation using zero‐fluoroscopy technique: a randomized trial. Pacing Clin Electrophysiol, 2015; 38(7): 797‐806.
- Ferguson JD, Helms A, Mangrum JM, et al. Catheter ablation of atrial fibrillation without fluoroscopy using intracardiac echocardiography and electroanatomic mapping. Circ Arrhythm Electrophysiol, 2009; 2(6): 611‐619.
- Sawhney V, Breitenstein A, Watts T, et al. A novel technique for performing transseptal puncture guided by a non‐fluoroscopic 3D mapping system. Pacing Clin Electrophysiol, 2019; 42(1): 4‐12.
- Chierchia GB, Capulzini L, de Asmundis C, et al. First experience with real‐time three‐dimensional transoesophageal echocardiography‐guided transseptal in patients undergoing atrial fibrillation ablation. Europace, 2008; 10(11): 1325‐1328.
- Scaglione M, Ebrille E, Clemente FD, Gaita F, Bradfield JS. Catheter ablation of atrial fibrillation without radiation exposure using A 3D mapping system. J Atr Fibrillation, 2015; 7(5): 1167.
- Clark BC, Sumihara K, Berul CI, Moak JP. Off the pedal: fluoroless transseptal puncture in pediatric supraventricular tachycardia ablation. Pacing Clin Electrophysiol, 2017; 40(11): 1254‐1259.
- Di Biase L, et al. Understanding the anatomy of the interatrial septum: Implications for transseptal puncture. Circulation: Arrhythmia and Electrophysiology, 2017; 10(2), e004624. https://doi.org/10.1161/CIRCEP.116.004624.
- Knauth AL, Saxon LA. Minimizing complications in transseptal catheterization: Advances and practical tips. Journal of Interventional Cardiology, 2021; 34(1): 62-70. https://doi.org/10.1111/jic.12921.
- Gill JS, Li G. Fluoroscopy-guided transseptal puncture: Technique and considerations. Journal of the American College of Cardiology, 2018; 72(12): 1484-1492. https://doi.org/10.1016/j.jacc.2018.07.077.
- Lee KH, Park JY. Transseptal puncture: Techniques and complications. Korean Circulation Journal, 2020; 50(2): 151-158. https://doi.org/10.4070/kcj.2020.0305.
- Calkins H, Kuck KH. Catheter ablation of atrial fibrillation: A comprehensive guide. Cardiac Electrophysiology Clinics, 2019; 11(3): 291-302. https://doi.org/10.1016/j.ccep.2019.03.002.

