Knowledge, Attitude, and Practice (KAP) of Health Care Professionals (HCPs) about Probiotics Use in Division Gujranwala, Punjab, Pakistan
Amna Shafqat1, Aqna Malik2,*, Dr. Muhammad Abbas Sadiq3, Muhammad Zafar Siddiq4, Dr. Shumaila Fatima5 and Amna Bashir6
1Department of Pharmacy, University of Chenab, Gujrat, Pakistan
2Department of Pharmacy, University of Chenab, Gujrat; Department of Pharmacy, The University of Lahore, Pakistan
3Relizon Pharmaceutics, Department of Pharmacy, The University of Lahore, Pakistan
4M Phil Pharmaceutics, Department of Pharmacy, The University of Lahore, Lahore, Pakistan
5Khawaja Muhammad Safdar medical college Sialkot
6Department of Pharmacy, The University of Lahore, Pakistan
Received Date: 09/12/2024; Published Date: 13/01/2025
*Corresponding author: Dr. Aqna Malik, Department of Pharmacy, University of Chenab, Gujrat; Department of Pharmacy, University of Lahore, Lahore, Pakistan
https://orcid.org/0000-0003-3875-9621
Abstract
Background: The phrase 'probiotic' is derived from the Latin word 'pro,' meaning 'for,' and the Greek word 'bios,' meaning 'life.' It is considered contrary to “antibiotic” which was first used back in the 1960s.
Objectives: The study sought to evaluate the knowledge, attitudes, and practices (KAP) of HCPs concerning the application of probiotics in various health situations and to identify the hurdles associated with their utilization.
Methods: A cross-sectional study was conducted on 206 HCPs (Pharmacists, Pediatricians, GPs, and Gastroenterologists) via a validated self-administered closed-ended questionnaire to evaluate their KAP towards probiotic use. The study data were analyzed using descriptive statistics, the Friedman test, and one sample t-test.
Results: Among the 206 participants, 48±31 were familiar with probiotics and their potential health benefits, 49 ± 31 considered yogurt, and butter, milk as probiotic-rich food. 20±17 have excellent Levels of confidence in accurate probiotic prescribing however 23±13 were confident about the efficacy of probiotics. 42±27 thought that Probiotics should be a part of routine healthcare 37±21thought that Probiotics are valuable for maintaining good health. 6.3 ± 4.3 liked to prescribe gut care sachet for GIT-related issues.
Conclusion: In the present study, overall good knowledge and practices regarding the use of probiotics among HCPs were seen While the participants showed mixed attitude towards the utilization of probiotics. To convert HCP's positive attitude to their practices and to create responsiveness regarding probiotic use focused training programs should be initiated by professional health organizations.
Keywords: HCPs; KAP; Probiotics; Gutcare
Background
The human GIT has millions of microorganisms collectively known as gut microbiota. The human body derives significant advantages from these bacteria in multiple aspects, including energy production, immune system regulation, pathogen defense, and lipid metabolism. The bacteria present in various food products or nutritional supplements might alter the composition of the microorganisms that flourish in the gastrointestinal system [1,2]. The term "probiotic," originating in the 1960s, derives from the Latin "pro," meaning "for," and the Greek "bios," signifying "life." It is considered the antonym of the phrase "antibiotic." [3].
According to The Food and Agriculture Organization/World Health Organization (FAO/WHO), probiotics are live microorganisms that boost the immunity of the host when administered as medicine. The efficacy of probiotics in preventing and managing various ailments has led to a marked surge in interest regarding their application recently. Probiotics are beneficial for GIT in, medical conditions like lactose intolerance, acute infectious diarrhea, antibiotic-associated diarrhea, Clostridium difficile-induced diarrhea, and travel-related diarrhea. The Food and Drug Administration (FDA) does not classify probiotics as pharmaceuticals, as they are considered part of a balanced diet. However, generally, individuals across various age groups consider them to be safe and acceptable [4].
Probiotics may be derived from bacteria including E coli, Leuconostoc, Enterococcus, Streptococcus, and Pediococcus species. Yeasts like Saccharomyces boulardii may also be utilized. However, a variety of novel possible probiotic taxa are expected in the future. system, and facilitate digestion [5,6]. The predominant bacteria present in several probiotic products belong to the Bifidobacterium and Lactobacillus genera. Research indicates that probiotics enhance the gastrointestinal tract's defenses against potential infections, and augment the functionality of the mucosal immune [7]. A probiotic product may be classified by the US Food and Drug Administration (FDA) as a pharmaceutical, food additive, or dietary supplement, contingent upon its intended usage. Probiotics, as nutritional supplements that can be marketed without FDA approval, are sold in substantial quantities. Probiotic products are typically recognized to possess a minimum concentration of 106 CFU/ml; however, the minimum effective quantities remain undetermined. Selecting the optimal probiotic can be a daunting endeavor. Nonetheless, a prior study identified that the primary characteristics affecting the efficacy of probiotics are disease specificity, strain specificity, and mode specificity [8].
HCPs play a crucial role in the integration of probiotics into clinical practice. The prescribing habits, knowledge, and attitudes of healthcare providers significantly influence patient care approaches and the utilization of probiotics as adjunct or supplementary therapy. Understanding the attitudes and behaviors of physicians toward probiotics is essential for enhancing patient care pathways and promoting evidence-based healthcare practices [9].
Several clinical trials have shown that probiotics can be used safely and successfully. However, less information is available about knowledge and perception of probiotics and HCPs [10]. The majority of previously published studies on probiotics were primarily concerned with figuring out how they worked and whether they had any health advantages. Regretfully, there isn't much-published research on the variables affecting probiotic usage. It is well established that HCPs’ (HCPs) attitudes and expertise on probiotics may influence how they prescribe and that the information they provide has a direct impact on patients' use of probiotics [11].
The current Survey aimed to look at the present attitudes and prescribing practices of physicians regarding probiotics in various treatments. With main objective was to assess the knowledge, Perception, Follow-up, driving force, and prescribing trends of HCPs regarding the use of probiotics in different health conditions and identify various barriers associated with their use.
Methodology
In this cross-sectional study, a random sample of HCPs participated in a face-to-face survey, also known as a personal interview was conducted from November 2023 to February 2024. The study adhered to ethical standards for using human subjects in research, making sure that each participant gave their informed consent and that their privacy was safeguarded at all times. After written approval from the IRB committee of the educational institute and concerned hospitals from district Gujranwala. A printed copy of the generated questionnaire, along with instructions for completing it was sent to HCPs who qualified. HCPs are included like General Physicians, Pediatrics, Gastroenterology and Pharmacist in current study. General population and patients were excluded as the study was focused only on HCPs. Out of the 250 surveys that were delivered, 206 HCPs responded. Since the study participants in this instance were HCPs exclusively, there were no patients involved. The following survey questions were directed toward HCPs who wrote prescriptions on an ongoing basis, whether supplements or foods containing probiotics were routinely prescribed; what the indications were for the recommendations or prescriptions; how to choose a probiotic supplement based on its indication; and how to use probiotics when taking antibiotics like AAD. The survey was divided into four sections: probiotic knowledge, perception, driving force, follow-up, and probiotic prescribing trends. The final collected data was analyzed using Microsoft Excel and GraphPad Prism 10.4.1
Results
Among 206 participants 61% of the HCPs were from 29-39 years old, 23% 39-49 years and 16% were from 49-59 years including 46.12% GPs, 8.74% Pharmacists, 25.73% Pediatrics, and only 19.42%. Gastroenterologists. As far as the experience was concerned 31% of among 206 had professional medical experience of ≤4 years (Most of them were GPs), 45% were in the medical field of 5–10 years (Pharmacists and Peads) and 24% had practiced from ≥11 years (Gastro specialists). Among 206 participants the HCPs prescribed to the patient population were Adult 54.85%, pediatric 27.18%, Geriatric 9.23%, and Adult/Pediatrics 7.28%. To analyze KAP following elements were assessed.
I. Knowledge about Probiotics
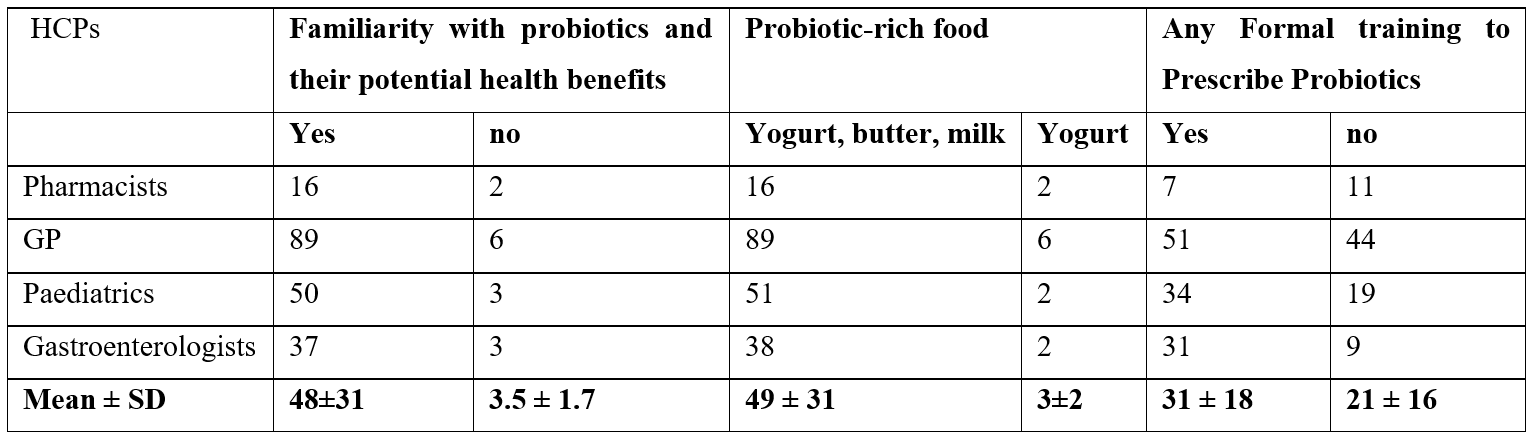
Among 206 participants 96% of HCPs were familiar with probiotics and 4% are those who were not familiar with probiotics. 90% of HCPs recommended yogurt as a probiotic-rich food, 5% recommended butter and milk, and 5% recommended cheese and yogurt. 60% of HCPs obtained formal training in probiotics. Overall, a comparison among HCPs regarding knowledge about probiotics is tabulated and analyzed on GraphPad Prism 10.4.1 in Table 1.
Table 1: Knowledge about Probiotics among HCPs.
II. Perception of Probiotics
Perception about Probiotics was assessed by Information regarding pharmaceutical specifications about product HCPs and, the role of probiotics in maintaining good health as a part of routine healthcare. All this was tabulated and analyzed. The information level of 61% of HCPs about pharmaceutical specifications of probiotics was good, fair in 24%, and poor in 7%. 6% had excellent Information regarding pharmaceutical specifications about product probiotics. Among 206 participants 82% of HCPs considered probiotics valuable for maintaining good health, 14% were neutral and 4% disagreed. 72% of HCPs considered probiotics as a part of routine healthcare, 24% were neutral and 4% were not considering probiotics as a part of routine healthcare. 46% of HCPs were very confident regarding the efficacy of probiotics, 37% were neutral and 17% were poor confident. Comaprison among HCPs regarding Confidentiality levels about accurate probiotic prescribing and efficacy of probiotics was tabulated in Table 2.
Table 2: Confidentiality levels about accurate probiotic prescribing and efficacy of probiotics.
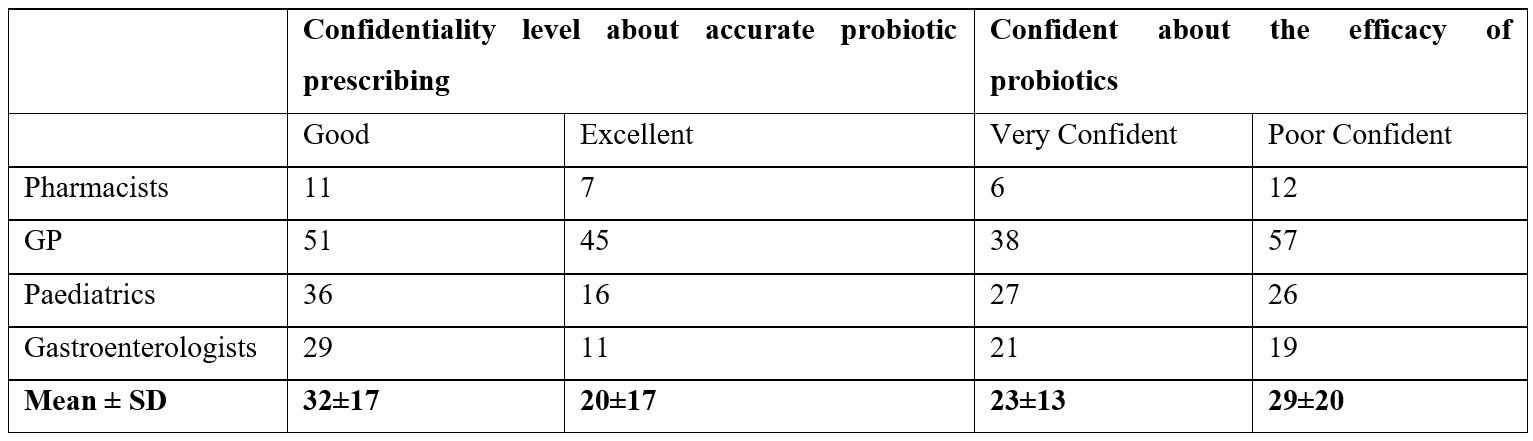
There is a significant difference observed between a good level of confidentiality in accurate probiotic prescribing and confidence about the efficacy of probiotics (p=0.0390). It means all HCPs who have good levels of confidentiality in accurate probiotic prescribing are confident about its efficacy.
III. Driving force to prescribe probiotics
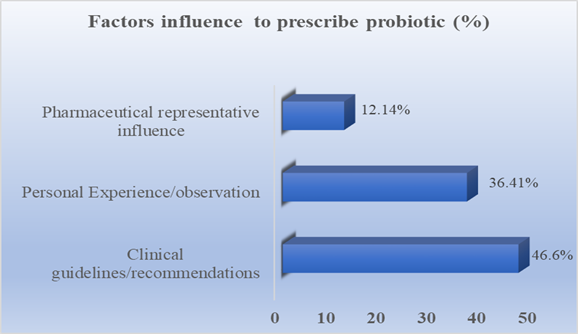
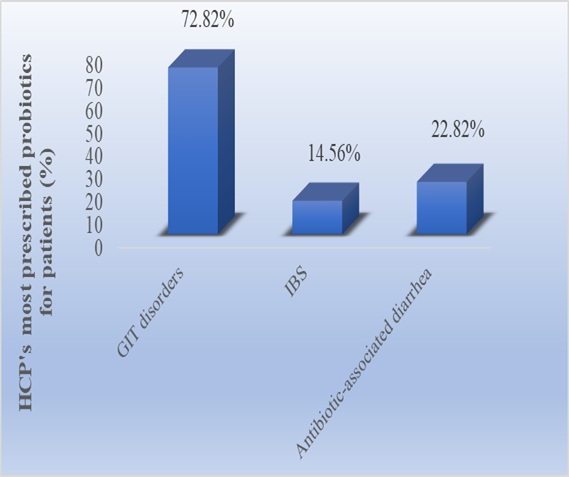
The driving force to prescribe probiotics was firstly assessed by questions about factors influencing prescription probiotics Figure 1. Secondly, which ailment was targeted most ly to prescribe probiotics by HCPs, Figure 2.
IV. Follow-up clinical data management
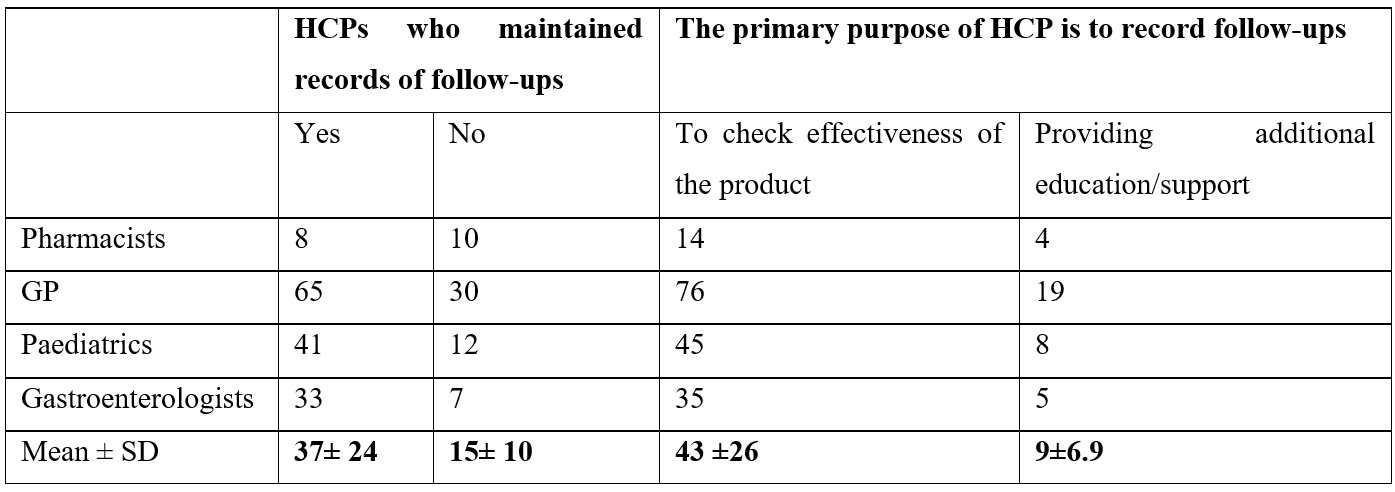
Follow-up clinical data management was assessed via questions regarding the record of follow-ups and the Primary purpose of HCPs to record follow-ups. GPs maintained records of patients who visited clinics for follow-ups mostly with the Primary purpose to assess the effectiveness of treatment.
Table 3: Clinical data management of probiotics among HCPs.
V. Prescribing Trends of Probiotic-brands)
Prescribing Trends were judged from questions regarding willingness to recommend and prescribe probiotics. Although 93% HCPs were prescribing probiotics routinely to their patients in their concerned health facilities but only 74% were willing to recommend probiotics to their patients and 26% remained neutral.
VI. Influence of Marketing on Probiotics Prescribing Trends
Influence of Marketing on Probiotics Prescribing Trends was checked via the frequency of prescribing probiotic brands in prescriptions of OPD patients. Among 206 participants 29.61% of HCPs were prescribed Gutcare Sachet, 18.45% prescribed Biflor sachet, 16.5%, prescribed Enflor Sachet, 15.05% prescribed Ecotec Sachet and 26.21% prescribed Enterogermina. Comparison among HCPs regarding different dosage forms and brands of probiotics was tabulated and analyzed.
Table 4: Perception of HCPs regarding Dosage forms and brands of probiotic.
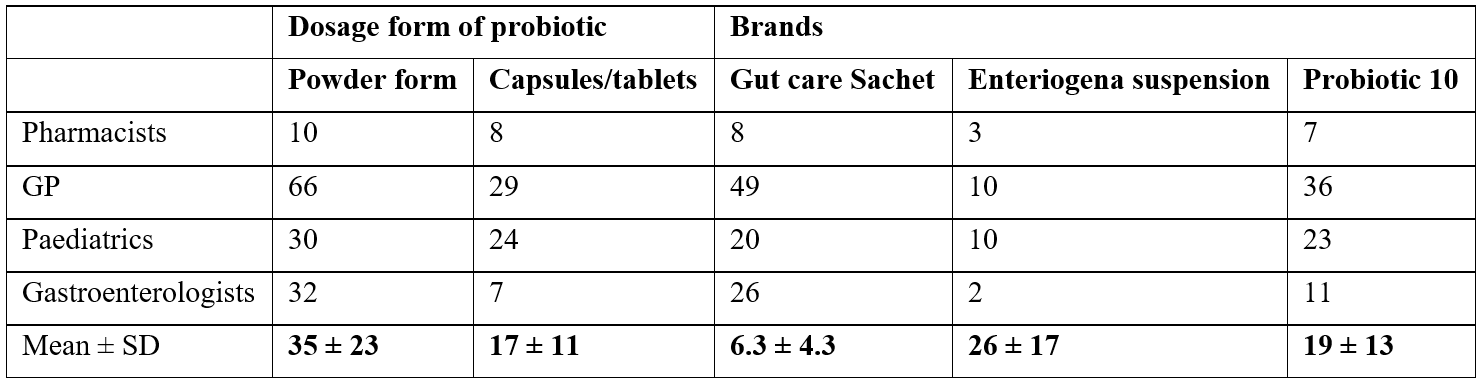
Friedman test was applied on Dosage form of probiotics vs Brands available in the market with different dosage forms. Promising results were observed between groups of Dosage forms of probiotics vs Brands with significant exact (p=0.0007). All HCPs were confident to prescribe powder for reconstitution as probiotics with the brand name Gut Care Sachet easily available in the market (p=0.0035).
Discussion
This cross-sectional study assessed the knowledge, attitudes, and practices (KAP) of probiotics use among HCPs in Division Gujranwala. Among 206 participants, 46.12% were GPs ,19.42% were (Gut specialists) Gastroenterologists. Remaining were Pharmacists 8.74% and Pediatricians 25.73%.
It was found that all GPs have professional medical experience of ≤4 years of as compared to pharmacist and peads (5–10 years) and Gastroenteriologists ≥11 years of experience, however, GPs were prescribing mostly. Probiotics were mostly prescribed to adults 54.85%, as compared to Pediatrics (27.18%), Geriatrics (9.23%) which indicated low immunity in young population. GPs and pediatricians predominantly administered probiotics for GIT in both adult and pediatric patients.
HCPs have a good level of knowledge which was judged by Familiarity with probiotics and their potential health benefits. GPs have more familiarity of probiotics as compared to others. HCPs preferred yogurt, butter, and milk (49 ± 31) as probiotic-rich food as compared to yogurt only (3±2). 31 ± 18 HCPs have obtained formal training and among those (51%) were GPs. 96% of respondents were knowledgeable about probiotics.
The survey indicated that most HCPs expressed a desire to acquire further knowledge about probiotics, with over half holding a favorable view of them. Moreover, it was established that the principal impediment to probiotic utilization was insufficient awareness regarding the various products accessible.
61% of HCPs possess a good understanding of probiotics, 24% have a fair understanding, 7% have a poor understanding, and 6% have an excellent understanding. Most HCPs regard probiotics as beneficial to maintaining good health, while 14% remain neutral, and 4% do not consider probiotics valuable for health maintenance. 72.82% of HCPs prescribed probiotics to GIT patients, 22.82% to patients with antibiotic-associated diarrhea, and 14.56% to patients with irritable bowel syndrome. Moreover, it was found that GPs and pharmacists had the least awareness of gastrointestinal issues, whilst pediatricians and gastroenterologists demonstrated the highest level of expertise. This may be attributed to the prevalent utilization of probiotics in the treatment of pediatric diseases such as irritable bowel syndrome and diarrhea. 46% of HCPs exhibited great trust in the efficacy of probiotics, 37% maintained a neutral stance, and 17% expressed low confidence. 74% of HCPs were inclined to offer probiotics to their patients, while 26% remained neutral. 46% of HCPs express strong confidence in the efficacy of probiotics, 37% remain indifferent, and 17% exhibit low confidence.
These findings, however, align with a Pakistani study indicating that healthcare practitioners' attitudes and comprehension of probiotics affect their current practice. Furthermore, one of the criteria assessed in this study was the respondents' inclination to recommend probiotics to future patients, primarily evaluated among HCPs. 93% of HCPs consistently administer probiotics to their patients, while 7% do not prescribe them regularly. 74% HCPs preserve follow-up records, 21% didn’t reply to questions, and 5% did not maintain follow-up records of patients. Among those 80.1% of healthcare providers document follow-up records to evaluate treatment efficacy, while 12.14% do so to offer supplementary information and support to their patients. 46.6% of HCPs prescribed probiotics by clinical recommendations, 36.41% based on personal experience and observations, and 12.14% influenced by pharmaceutical representatives. 29.61% of HCPs prescribed Gutcare Sachet, 18.45% prescribed Biflor Sachet, 16.5% prescribed Enflor Sachet, 15.05% prescribed Ecotec Sachet, and 26.21% prescribed Enterogermina. >80% of HCPs agreed that probiotics should be consumed regularly for an extended duration. 87.8% of respondents strongly concurred that oral probiotic use can positively influence health [12].
The overall classification of knowledge, attitude, and practice was deemed excellent if the total score ranged from 60 to 79%, moderate if it spanned from 60 to 100%, and poor if it fell below 60% [13]. HCPs had a commendable degree of understanding and training about probiotics, with 72.82% recommending them for gastrointestinal issues such as diarrhea and irritable bowel syndrome.
Global understanding of probiotics significantly surpasses that of Pakistan. The limited awareness of probiotics among HCPs may account for the reduced utilization of probiotic products in Pakistan. Moreover, the HCPs claimed that insufficient information was the primary barrier to refraining from providing probiotics, corroborating findings from another published research. Enhanced probiotic understanding among HCPs will elevate their capacity to treat patients safely and efficiently.
This study suggests that the utilization of probiotics is predominantly limited. Despite the favourable outcomes of numerous prior researches indicating progress on this topic, HCPs still have misgivings and encounter challenges in providing probiotics [12].
If the whole score fell between 60 and 79%, moderate if it fell between 60 and 100%, and poor if it fell below 60%, the knowledge, attitude, and practice were classified as good overall [13].
Probiotic knowledge is far more advanced worldwide than it is in Pakistan. The low probiotic awareness among HCPs may be the reason for Pakistan's lower usage of probiotic products. Furthermore, the HCPs claimed that a lack of information was the largest obstacle to not prescribing probiotics, which is in line with another research that have been published. Higher probiotic knowledge among HCPs will boost their energy levels to treat patients safely and effectively [14].
Conclusion
The findings highlight how crucial it is that medical practitioners have up-to-date and appropriate knowledge about probiotics. Prescriptive confidence rose as information about probiotics improved. HCPs seek out relevant and scientifically validated educational platforms to gather information, investigate issues and obstacles, and seek out constructive methods for probiotic recommendation in order to distribute accurate information about probiotics.
Recommendations
- Current Cross-sectional study has uncovered insufficient knowledge and practices regarding the use of probiotics. The subjects demonstrated a positive attitude towards the use of probiotics. Through training initiatives, professional health organizations should take the lead in changing the positive attitudes that HCPs have toward their work and increasing public knowledge of the use of probiotics.
- Probiotics should also be included in various healthcare programs.
- Future health professionals’ curricula and the targeted learning programs for working HCPs could benefit from including this topic in their curriculums, since health practitioners have expressed interest in learning more about probiotics and are the ones who have to prepare various guidelines for probiotic use based on evidence-based research.
Strengths and limitations of this study
Strengths:
- The current study was cross-sectional, so the contributing relationship cannot be established.
- We have reported for the very first time (HCPs) knowledge, attitude, and practices (KAP) towards probiotic use in Division Gujranwala. Punjab, Pakistan. The sample size was inflated by 10% to minimize the errors in completing the questionnaire and to identify significant influencing factors of KAP among the HCPs.
- The response bias may be present in the present study due to the use of self-reporting data, which may affect the accuracy of the findings.
Limitations:
- The present study was conducted only in the HCPs of Division Gujranwala. Punjab, Pakistan, and the results cannot be generalized to the HCPs working in the whole country.
- This study is limited to only HCPs who are practicing in their professions i.e. pharmacists, general practitioners, gastroenterologists, and pediatrics.
References
- Rodríguez JM, Murphy K, Stanton C, Ross RP, Kober OI, Juge N, et al. The composition of the gut microbiota throughout life, with an emphasis on early life. Microbial ecology in health and disease, 2015; 26(1): 26050.
- Thursby E, Juge N. Introduction to the human gut microbiota. Biochemical Journal, 2017; 474(11): 1823-1836.
- Morelli L, Capurso L. "FAO/WHO guidelines on probiotics: 10 years later." Journal of Clinical Gastroenterology, 2012; 46: S1-S2.
- Ababneh M, Elrashed N, Al-Azayzih A. Evaluation of Jordanian healthcareproviders’ knowledge, attitudes, and practice patterns towards probiotics. Expert review of pharmacoeconomics & outcomes research, 2020; 20(1): 93-97.
- Chugh B, Kamal-Eldin A. Bioactive compounds produced by probiotics in food products. Current Opinion in Food Science, 2020; 32: 76-82.
- Gorreja F, Walker WA. The potential role of adherence factors in probiotic function in the gastrointestinal tract of adults and pediatrics: a narrative review of experimental and human studies. Gut Microbes, 2022; 14(1): 2149214.
- Fei YY, Steen J, Tutt E, Ng JY, Dobbins M. The impact of knowledge and attitudes on physicians', nurses' and pharmacists' recommendation of probiotics: A systematic review. European Journal of Integrative Medicine, 2023; 102272.
- O’la Ahmad A-F, Rayyan WA, Fararjeh AFS, Seder N. Probiotic therapy: A survey of Middle Eastern healthcare providers’ attitudes, beliefs, and practice patterns. Journal of Applied Pharmaceutical Science, 2023; 13(10): 172-180.
- Hempel S, Newberry SJ, Maher AR, Wang Z, Miles JN, Shanman R, et al. Probiotics for the prevention and treatment of antibiotic-associated diarrhea: a systematic review and meta-analysis. Jama, 2012; 307(18): 1959-1969.
- van der Geest AM. Probiotics in perspective: A closer look into practices and adoption in the current primary healthcare system, 2023.
- Liu RT, Walsh RF, Sheehan AE. Prebiotics and probiotics for depression and anxiety: A systematic review and meta-analysis of controlled clinical trials. Neuroscience & Biobehavioral Reviews, 2019; 102: 13-23.
- Ong TS. Assessment of knowledge, attitude and practice towards probiotics for gut-skin axis among health science undergraduates in Malaysia UTAR, 2022.
- Akalu Y, Ayelign B, Molla MD. Knowledge, attitude and practice towards COVID-19 among chronic disease patients at Addis Zemen Hospital, Northwest Ethiopia. Infection and drug resistance, 2020; 1949-1960.
- Wilson Z, Whitehead K. A cross sectional survey to assess HCPs' attitudes to and understanding of probiotics. Clinical nutrition ESPEN, 2019; 34: 104-109.
- Morelli L, Capurso L. FAO/WHO guidelines on probiotics: 10 years later. Journal of clinical gastroenterology, 2012; 46: S1-S2.
- Tuohy K, et al. "Survivability of a probiotic Lactobacillus casei in the gastrointestinal tract of healthy human volunteers and its impact on the faecal microflora." Journal of applied microbiology, 2007; 102(4): 1026-1032.

