Outcomes of Sensitizer-Induced Occupational Asthma: Clinical and Functional Features in Regard to Occupational Exposure After Diagnosis
Minov J1,*, Stoleski S1, Kocovska Kamcevska N2, Buklioska Ilievska D2 and Mijakoski D1, Atanasovska A1, Panajotovic Radevska M1, Bislimovska D1 and Zdraveski D1
1PHI Institute for Occupational Health of R. North Macedonia - Skopje, R. North Macedonia; Faculty of Medicine, Ss Cyril and Methodius University in Skopje, R. North Macedonia
2PHI City General Hospital “8th September” - Skopje, R. North Macedonia; Faculty of Medical Sciences – University “Goce Delchev” – Shtip, R. North Macedonia
Received Date: 04/12/2024; Published Date: 08/01/2025
*Corresponding author: Minov J, PHI Institute for Occupational Health of R. North Macedonia - Skopje, R. North Macedonia; Faculty of Medicine, Ss Cyril and Methodius University in Skopje, R. North Macedonia
Abstract
Introduction: Outcomes of sensitizer-induced Occupational Asthma (OA) and effectiveness of workplace interventions in regard to occupational exposure after diagnosis still are a matter of discussion.
Aim of the study: To evaluate clinical and functional outcomes of sensitizer-induced OA in regard to causative occupational exposure after the diagnosis was established.
Methods: We performed a cross-sectional study including 84 patients with sensitizer-induced OA diagnosed in the period 2015-2022. Regarding the workplace intervention after the diagnosis was established, study population was classified as subjects with continued exposure, subjects with reduced exposure and subjects with ended exposure to occupational agent associated with their disease, i.e. subjects removed to another workplace and unemployed subjects. All study subjects completed a questionnaire on asthma symptoms and underwent spirometric measurements.
Results: Frequency of symptomatic subjects was significantly higher in the group with continued exposure than in the groups with reduced and ceased causative exposure (79.1% vs. 28.6%; P = 0.0001 and 79.1% vs. 38.9%; P = 0.0214, respectively). Frequency of symptomatic subjects in the group of subjects with reduced exposure was non-significantly higher than its frequency in the group of subjects with ceased exposure (38.9% vs. 28.6%; P = 0.4311). Mean value of FEV1 was significantly lower in the groups of subjects with continued and reduced exposure than in the group of subjects with ceased causative exposure (78.4% vs. 85.7%; P = 0.0000 and 80.9% vs. 85.7%; P = 0.0009, respectively). Significant difference was also registered between mean FEV1 value in the group of subjects with continued exposure as compared to its mean value in the group of subjects with reduced exposure (78.4% vs. 80.9%; P = 0.0437).
Conclusion: Our findings indicated that cessation and reduction of exposure had better clinical and functional outcomes compared with study subjects with continued exposure. Study subjects with ended exposure had better functional outcomes compared to study subjects with reduced causative occupational exposure.
Keywords: Asthma symptoms; Causative occupational exposure; Continued exposure; Ended exposure; Reduced exposure; Spirometry
Introduction
According to the recent evidence, chronic respiratory diseases, excluding lung cancer and respiratory infections, are the third leading cause of death, being responsible for 4 million deaths and 103.5 million Disability-Adjusted Life Years (DALYs) worldwide in 2019 at global level. Workplace exposures are considered as one of the main risk factors for chronic respiratory diseases, i.e., they are in third place after smoking and particulate matter globally and rank second in some regions [1].
Occupational asthma, i.e., a new-onset asthma incited by causes and conditions only found at the workplace, is considered as the most frequent occupational ling disease in developed countries in the last decades. OA is not unique and homogenous entity, but includes two main subtypes, sensitizer-induced OA and irritant-induced OA, with significant difference in their frequency, pathogenesis and management. Sensitizer-induced OA, also referred to as immunologic OA or allergic OA, is more frequent OA subtype accounting more than 80% of all OA cases. It develops after a sensitization to certain high or low molecular weight occupational agent that leads to chronic allergic inflammation of the airways. Diagnosis of sensitizer-induced OA may negatively impact careers, incomes and quality of life of affected workers, but, so far, there is still insufficient evidence of outcomes of sensitizer-induced OA in regard to occupational exposure after its diagnosis with somewhat inconsistent findings from several studies in this field [2-7].
In the present study we evaluated clinical and functional outcomes of sensitizer-induced OA in a group of patients in regard to occupational exposure to agent associated with their disease 2 to 8 years after the diagnosis was established.
Methods
Study design and setting
A monocentric cross-sectional study was performed at the Institute for Occupational Health (IOH) of RN Macedonia, Skopje, in the period Fevruary – June 2024.
Study population
Study population included 84 patients (47 males and 37 females, aged 34 to 57 years) with sensitizer-induced OA diagnosed at the IOH (referral center for occupational diseases in RN Macedonia) in the period 2015-2022. In the mentioned period, sensitizer-induced OA was diagnosed in 102 workers but with 18 of them we had no contact after diagnosis was established so they were not included in the study. Diagnosis of immunologic OA was established in patients with diagnosed asthma and work-related asthma symptoms by positive results from serial measurements of peak expiratory flow rate (PEFR) at and away from work and combination of serial PEFR measurements and metacholine challenge at and away from work [8]. All study subjects used their regular treatment according to the recommendations of recent guidelines. In addition, all study subjects were informed about study and their written consent was obtained.
Study protocol
Study protocol included completion of an interview-led questionnaire and lung function measurements.
The questionnaire was consisted of three parts.
The first part of the questionnaire included questions on demographic and other characteristics of the study subjects (sex, age, education level, occupation, smoking status, and presence of other chronic diseases). Smoking status (active smoker, ex-smoker, and non-smoker) was defined by the World Health Organization (WHO) criteria [9]. In addition, this part of the questionnaire also included questions about duration of the certain occupational exposure before the diagnosis of OA was established, as well as duration of the period from onset of the symptoms and diagnosis of the disease.
The second part included questions on employment status (employed, unemployed and retired) of the study subjects. Regarding the causative occupational exposure after the diagnosis was established, study subjects were classified as subjects with continued exposure at the same workplace, subjects with reduced exposure at the same workplace, and subjects with ended causative occupational exposure. In addition, the study subjects were asked for the duration of the certain occupational exposure and respiratory symptoms before the diagnosis was established.
In the third part symptoms of the study subjects (cough, wheezing, shortness of breath, and chest tightness) were assessed by the European Community Respiratory Health Survey (ECRHS) questionnaire. As symptomatic were considered those who reported one or more respiratory symptoms in the previous 12 months [10].
Lung function measurements included spirometry which was performed in all study subjects following the actual recommendations [11,12]. The baseline spirometry, i.e., measures of forced vital capacity (FVC), forced expiratory volume in the first second (FEV1, FEV1/FVC, and maximal expiratory flow at 50%, 25%, and 25-75% of FVC (MEF50, MEF25, and MEF25-75, respectively), as well as bronchodilator test by indication, was performed using spirometer Ganshorn SanoScope LF8 (Ganshorn Medizin Electronic GmbH, Germany) with recording the best result from three measurements the values of FEV1 of which were within 5% of each other.
Statistical analysis
All analyses were carried out using the Statistical Package for the Social Sciences (SPSS) version 26.0. Continuous variables were expressed as mean values with Standard Deviation (SD), and the nominal variables as numbers and percentages. Data analysis was done using univariate statistical models for testing the differences in prevalence and comparison of the means, i.e., Chi-square test (or Fisher’s exact test where appropriate) and independent-samples T-test. The level of significance was set at P value less than 0.05.
Results
Demographic and other characteristics of the study subjects are shown on Table 1.
Table 1: Characteristics of the study subjects.
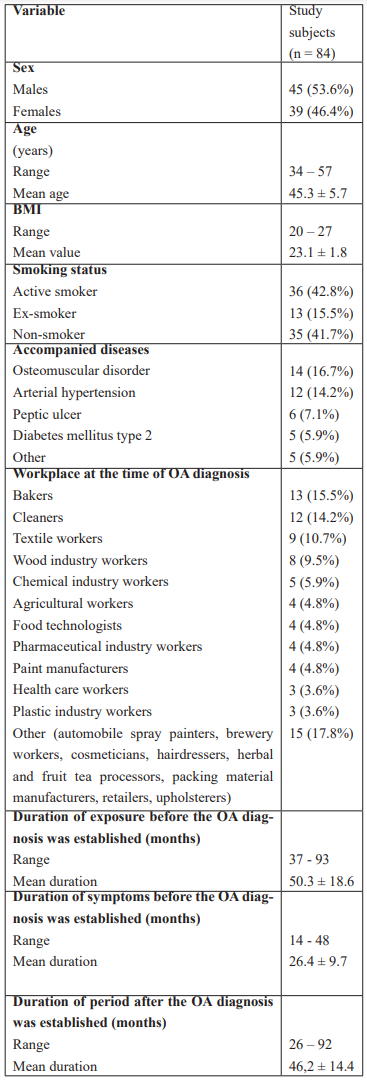
BMI: body mass index; OA: occupational asthma.
Of 84 study subjects with diagnosed OA, 24 (28.6%) continued work at the same workplace, 18 (21.4%) continued to work at the same workplace with workplace interventions aimed at reduction of exposure, 32 (38.1%) were removed to another workplace with different exposure, 10 (11.9%) were unemployed, and no one (0%) was retired (Figure 1).
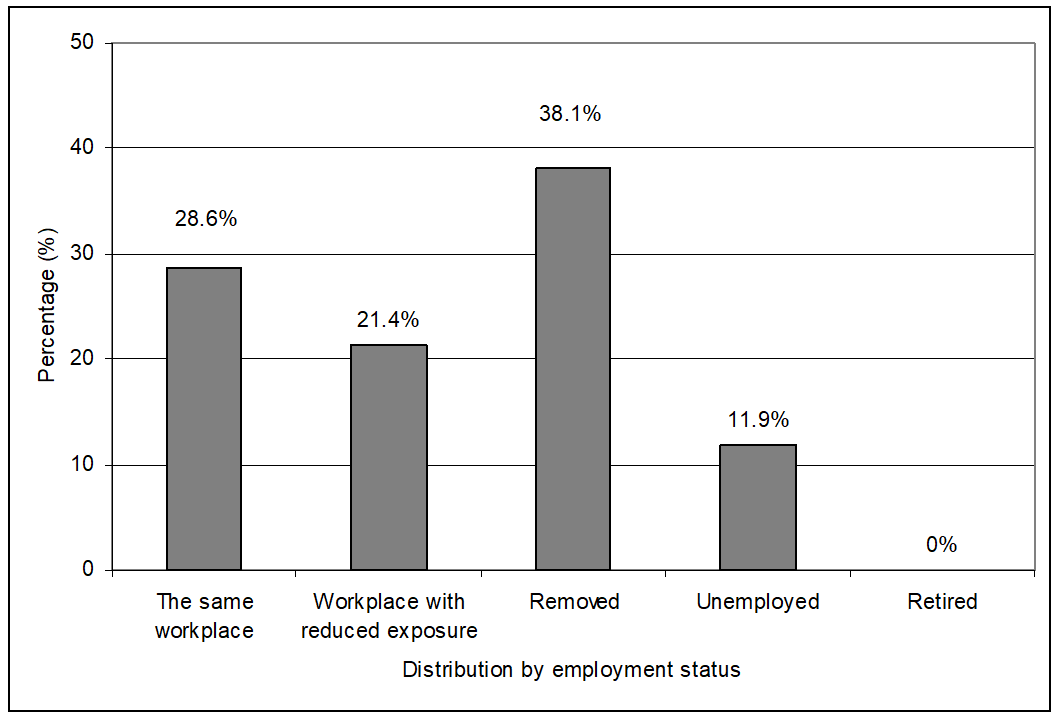
Figure 1: Distribution of study subjects by their employment status.
In regard to occupational exposure after the OA diagnosis, study subjects were classified as subjects with continued exposure, subjects with reduced exposure, and subjects with ended exposure to occupational agent associated with their disease, i.e., subjects removed to another workplace and unemployed subjects (Figure 2).
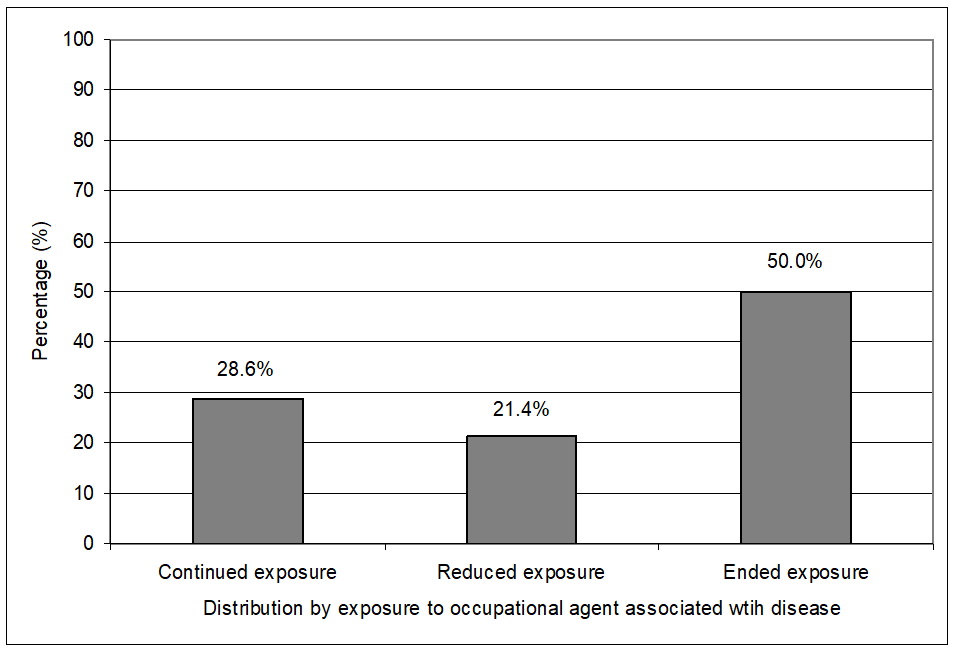
Figure 2: Distribution of study subjects by causative occupational exposure after the OA diagnosis was established.
Frequency of symptomatic subjects, i.e., study subjects who reported one or more respiratory symptoms in the previous 12 months, was significantly higher in the group of subjects with continued exposure than in the groups of subjects with reduced and ended exposure to occupational agent associated with their disease (79.1% vs. 28.6%; P = 0.0001 and 79.1% vs. 38.9%; P = 0.0214, respectively). In addition, frequency of symptomatic subjects in the group of subjects with reduced exposure was non-significantly higher than its frequency in the group of subjects with ended exposure (38.9% vs. 28.6%; P = 0.4311) (Figure 3).
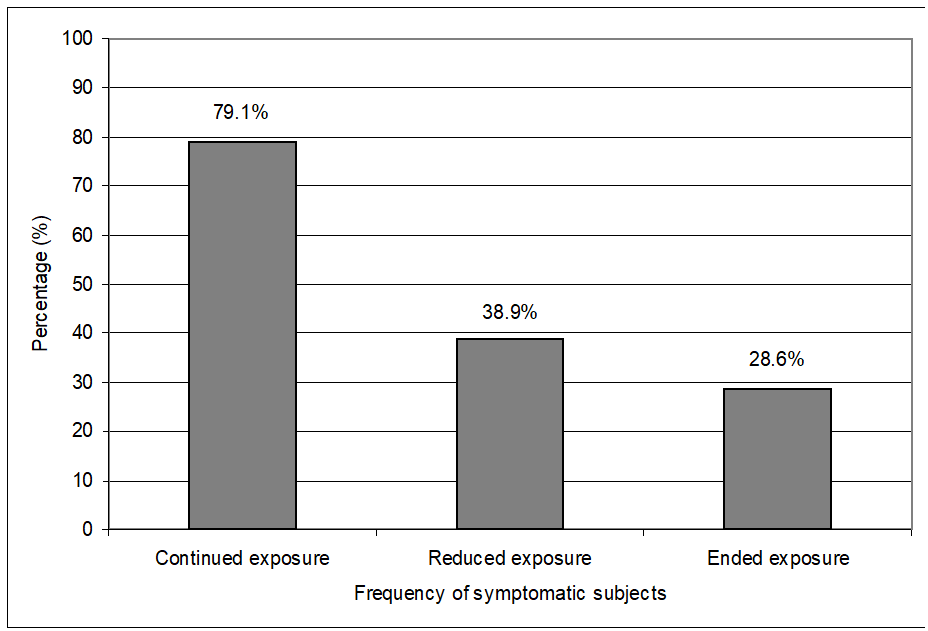
Figure 3: Frequency of symptomatic subjects in the groups with continued, reduced and ended exposure to occupational agent associated with their disease.
Mean value of FVC was significantly lower in the groups of subjects with continued and reduced exposure than in the group of subjects with ended exposure to occupational agent associated with their disease (91.2% vs. 96.3%; P = 0.0035 and 92.4% vs. 96.3%; P = 0.0409, respectively). Difference between mean FVC value in the group of subjects with continued exposure and reduced exposure was statistically non-significant (91.2% vs. 92.4%; P = 0.3251). Mean value of FEV1 was significantly lower in the groups of subjects with continued and reduced exposure than in the group of subjects with ceased causative exposure (78.4% vs. 85.7%; P = 0.0000 and 80.9% vs. 85.7%; P = 0.0009, respectively). Significant difference was also registered between mean FEV1 value in the group of subjects with continued exposure as compared to its mean value in the group of subjects with reduced exposure (78.4% vs. 80.9%; P = 0.0437). Finally, significant difference was registered between mean value of FEV1/FVC between the groups of subjects with continued and reduced exposure and the group of subjects with ceased exposure (85.4% vs. 88.8%; P = 0.0000 and 86.1% vs. 88.8%; P = 0.0036, respectively), while difference between mean FEV1/FVC value between groups with continued and reduced exposure was at border of statistical significance (85.4% vs. 86.1%; P = 0.094) (Figure 4).
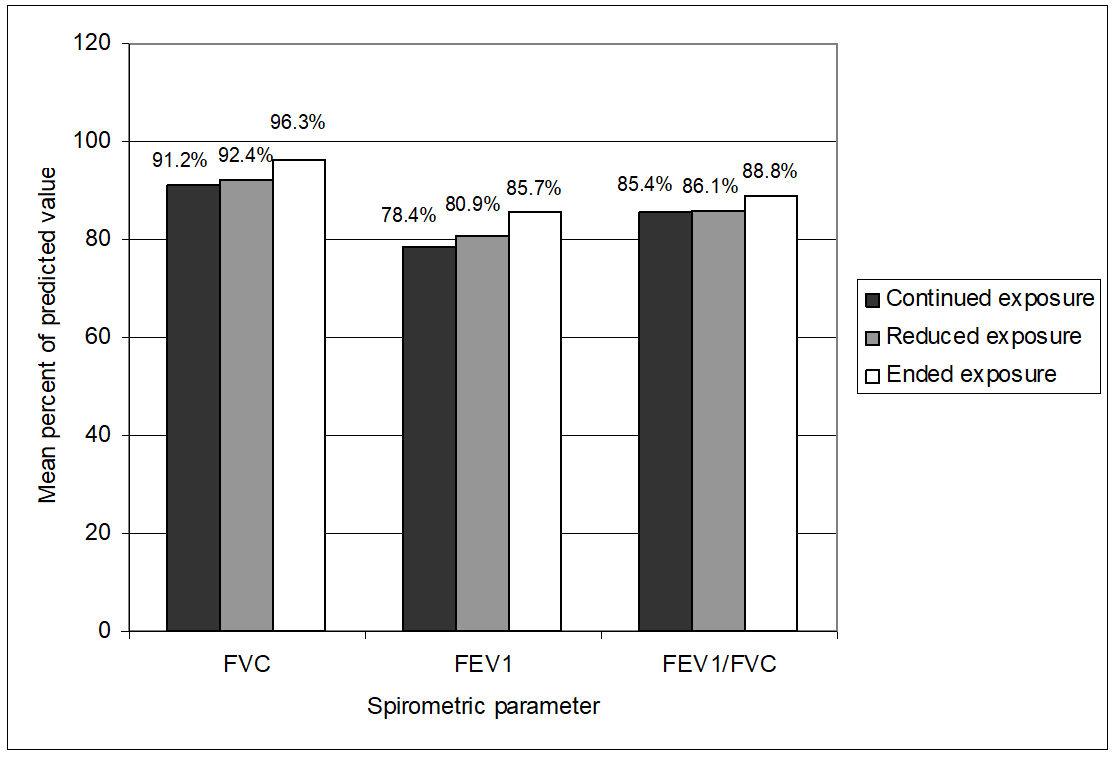
Figure 4: Mean value of FVC, FEV1 and FEV1/FVC in the groups with continued, reduced and ended causative occupational exposure.
Discussion
As it is mentioned earlier, OA became the most prevalent occupational lung disease in the developed countries in the last few decades, i.e., it is estimated that in one of five to ten adult asthma patients the disease is occupational by its origin. While OA remains under-recognized, especially in developing countries, it remains poorly diagnosed and managed and inadequately compensated worldwide [13,14]. On the other side, despite intensive efforts towards prevention, there is no compelling evidence for a decline in its frequency that may be partly explained by the introduction of new, potentially allergenic substances in production and processing that undo the effect of preventive measures taken previously [15-17].
According to the results from the literature, reported mean annual incidence of OA in developing countries varied from less than 2 per 100,000 working population, 4.2 per 100,000 working population in West Midlands, UK, up to 18/100,000 in Scandinavian countries [18-20]. According to the results of our studies, mean annual incidence of OA in the period 2005-2022 varied from 2.2 per 100.000 working population in 2005, 2.7 per 100.000 working population in 2011 to 2.6 per 100.000 working population in 2012, being at the range of its annual incidence in developing countries [8,21].
In the present study we evaluated clinical and functional outcomes of sensitizer-induced OA in a group of patients two to eight years after the diagnosis was established in regard to occupational exposure to agent associated with their disease. Study population included 84 workers with diagnosed sensitizer-induced OA at the IOH in the period 2015-2022. Majority of the subjects enrolled in the study were bakers, cleaners, textile workers and wood industry workers OA in which was caused by different high and low molecular occupational allergens (1B). Mean duration of occupational exposure and mean duration of symptoms before the OA diagnosis was established were four and two years, respectively. Similarly, to the findings of our previous studies, a large proportion of the study subjects, i.e., more than 40%, were active smokers that indicated still poor results of implemented anti-smoking strategies and activities [22].
According to analyze of Vandenplas et al., almost one third of workers with sensitizer-induced OA remained exposed to the causative agent of the disease after its diagnosis [23]. Regarding the employment status at the time when the present study was carried out, nearly 30% of the study subjects continued to work at the same workplace without any workplace intervention, around 20% worked at the same workplace with reduced exposure achieved by limiting period of exposure, improved ventilation and use of adequate respiratory protective equipment, around 40% were removed from causal occupational exposure by relocation or by a change in job position within the company, and around 10% were unemployed as they left their workplaces with continued or reduced exposure because of worsening of their disease. Similarly, to the results of the study cited above, around one third of the study subjects continued causal occupational exposure after the OA diagnosis. One fifth of the study subjects worked at the same workplace with reduced exposure to agent associated with their disease and a half of the study subjects ended causal occupational exposure due to removal to another workplace or unemployment.
Respiratory symptoms in the previous 12 months were reported by nearly 80% of the study subjects with continued exposure, nearly 40% of the study subjects with reduced exposure and nearly 30% of the study subjects with ended causative occupational exposure. In our previous study on clinical and functional outcomes of sensitizer induced OA including 16 bakers and cotton workers in a shorter period after cessation of exposure to the offending workplace agent (3 to 5 years) respiratory symptoms in the previous 12 months were reported by nearly 70% of the study subjects [24]. Regarding the results from spirometric measurements, we found significantly lower mean FVC values in the study subjects with continued and reduced exposure than in the study subjects with ended exposure, while the difference of mean FVC value between study subjects with reduced and ended exposure was not statistically significant. In addition, mean FEV1 value was significantly lower in the study subjects with continued and reduced exposure than in the study subjects with ended exposure. Significantly lower mean FEV1 value was also registered in the study subjects with reduced exposure compared to the study subjects with ended exposure. In a systematic review including 26 studies, Henneberger et al. found that removal and reduction of exposure as compared to continued exposure increased the likelihood of absence of asthma symptoms. Removal from exposure, but not reduction of exposure, may improve lung function when compared to continued exposure. In addition, results from some of reviewed studies indicated that removal from exposure compared to reduction of exposure had better functional outcome in sensitizer-induced OA patients exposed to low molecular weight agents [25-28]. On the other hand, in a systematic review of studies on effects of reduction of causal exposure compared to its complete avoidance in subject with sensitizer-induced OA, Vandenplas indicated that reduction of exposure to the causal agent is associated with a lower likelihood of improvement in asthma symptoms and a higher risk of worsening of symptoms and nonspecific bronchial hyper-responsiveness [29].
Findings of the present study should be interpreted in the context of its limitations. Relatively small size of study population, as well as a cross-sectional analysis, could have implication on the results obtained and their interpretation. In addition, study population was heterogenous regarding the causal occupational exposure, as well as regarding the duration of exposure to offending occupational agent, that could also have implication on the results obtained and their interpretation. On the other side, findings resulted from this real-life study could help in understanding of the course of sensitizer-induced OA, as well as in decision for further working activities and working environment of these patients.
Conclusion
In a cross-sectional study investigating clinical and functional outcomes in a group of workers with sensitizer-induced OA caused by different high and low molecular agents in regard to their occupational exposure after diagnosis we found that both cessation and reduction of exposure had better clinical and functional outcomes compared with study subjects with continued occupational exposure to agent associated with their disease. Study subjects with ended exposure had better functional outcomes compared to study subjects with reduced exposure to agent associated with their disease. Our findings indicated a need of further studies on evaluation of workplace interventions in order to choose optimal management option for workers with sensitizer-induced OA.
Competing Interests: All authors hereby have declared that no competing interests exist.
Authors Participation: MJ, SS, KKN, and BID participated in data collection, data analysis, and writing all versions of the manuscript. MD, AA, PRM, BD, and ZD participated in data collection. All authors read and approved the final version of the manuscript.
References
- GBD 2019 Chronic respiratory Disease Collaborators. Global burden of chronic respiratory diseases and risk factors, 1990-2019: an update from the Global Burden of Disease Study 2019. EClinicalMedicine, 2023; 59: 101936.
- Maestrelli P, Schlunssen V, Mason P, Sigsgaard T. Contribution of host factors and workplace exposure to the outcome of occupational asthma. Eur Respir Rev, 2012; 21: 88-96.
- TiotIu AI, Novakova S, Labor M, et al. Progress in Occupational Asthma. Int J Environ Res Public Health, 2020; 17: 4553.
- Minov J. Occupational chronic obstructive pulmonary disorder: prevalence and prevention. Expert Review of Respiratory Medicine, 2021. DOI 10.1080/17476348.2021.2011722.
- Mason P, Liviero F, Paccagnella ER, et al. Impact of occupational asthma on health and employment status: a long-term follow-up study. Occup Environ Med, 2023; 80(2): 70-76.
- Suojalehto H, Lindstrom I. Long-term outcome of occupational asthma with different etiology. Curr Opin Allergy Clin Immunol, 2024; 24(2): 64-68.
- Murgia N, Akgun M, Blanc PD, et al. Issue 3-The occupational burden of respiratory diseases, an update. Pulmonology, 2024. https://doi.org/10.1016/jpulmoe.2024.2304.
- Minov J, Stoleski S, Mijakoski D, et al. Incidence of Immunological Occupational Asthma in 2015-2022 by Occupation: Macedonian Experience. SEE J Immunol, 2023; 6(1): 7-11.
- WHO Report on the Global Tobacco Epidemic, 2019, Geneva: World Health Organization, 2019.
- European Community Respiratory Health Survey. Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European Respiratory Health Survey (ECRHS). Eur Respir J, 1996; 9: 687-695.
- Culver BH, Graham BL, Coates AL, et al. Recommendations for Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement. Am J Respir Crit Care Med, 2017; 196 (11): 1463-1472.
- Townsend MC. The American Thoracic Society / European Respiratory Society 2019 Spirometry Statement and Occupational Spirometry Testing in the United States. Am J Respir Crit Care Med, 2020; 201(8): 1010-1011.
- Sigsgaard T, Nowak D, Annesi-Maesani I, Nemery B, Toren K, et al. and the ERS EOH group 6.2. ERS position paper: work-related respiratory diseases in the EU. ERS Respir J, 2010; 35: 234-238.
- Tarlo SM, Balmes J, Balkissoon R, Beach J, Beckett W, et al. Diagnosis and Management of Work-Related Asthma. American College of Chest Physiciand Statement. Chest, 2008; 134: 1-41.
- McDonald JC, Chen Y, Zekveld C, Cherry NM. Incidence by occupation and industry of acute work-related respiratory diseases in the UK, 1992–2001. Occup Environ Med, 2005; 62: 836–842.
- Brant A. Baker’s asthma. Curr Opin Allergy Clin Immunol, 2007; 7: 152–155.
- Broding HC, Frank P, Hoffmeyer F, Bunger J. Course of occupational asthma depending on the duration of workplace exposure to allergens – a retrospective cohort study in bakers and farmers. Ann Agric Environ Med, 2011; 18: 35-40.
- Jeebhay MF, Quirce S. Occupational asthma in the developing and industrialized world: a review. Int J Tuberc Lung Dis, 2007; 11(2): 122-133.
- Hnizdo E, Esterhuizen TM, Rees D, Lalloo UG. Occupational asthma as identified by the Surveillance of Work-related and Occupational Respiratory Diseases in South Africa. Clin Exp Allergy, 2001; 31(1): 32-39.
- Diar Bakerly S, Moore VC, Vellore AD, et al. Fifteen-year trend in occupational asthma: data from the Shield surveillance scheme. Occup Med, 2008; 58: 169-174.
- Minov J, Karadzinska-Bislimovska J, Vasilevska K, et al. Distribution of sensitizer-induced occupational asthma in R. Macedonia in the period 2005-2014 by occupation. Glob J Allergy, 2015; 1(1): 104.
- Minov J, Stoleski S, Stikova E, et al. COPD in a sample of general adult population from the Skopje region. Acad Med J, 2022; 2(1): 47-58.
- Vandenplas O, Toren K, Blanc PD. Health and socioeconomic impact of work-related asthma. Eur Respir J, 2003; 22: 689-697.
- Minov J, Karadzinska-Bislimovska J, Tutkun E, et al. Clinical and Functional Outcomes of Sensitizer-Induced Asthma in Bakers and Cotton Workers after Removal from Exposure. Arch Pulmonol Resp Care, 2016; 2(1): 001-006.
- Henneberger PK, Patel JR, de Groene GJ, et al. Workplace interventions for treatment of occupational asthma. Cochrane Database of Systematic Reviews, 2019; 10: Art. No.: CD006308. doi: 10.1002/14651858 CD006308.pub4.
- Henneberger PK, Patel JR, de Groene GJ, et al. The effectiveness of removal from exposure and reduction of exposure for managing occupational asthma: Summary of an updated Cochrane systematic review. Am J Ind Med, 2021; 64(3): 165-169.
- Talini D, Novelli F, Melosini L, et al. May the reduction of exposure to specific sensitizers be an alternative to work cessation in occupational asthma? Results from a follow-up study. Int Arch Allergy Immunol, 2012; 157(2): 186–193.
- Talini D, Novelli F, Bacci E, et al. Mild improvement in symptoms and pulmonary function in a long-term follow-up of patients with toluene diisocyanate-induced asthma. Int Arch Allergy Immunol, 2013; 161(2): 189–194.
- Vandenplas O. Reduction of exposure in the management of occupational asthma. Curr Opin Allergy Clin Immunol, 2011; 11: 75-79.

