Histopathological Profile of Rhabdomyosarcomas in the Congolese Child at the Anatomopathological Laboratories of Kinshasa/ RDCongo
Nsumpi Tshimanga Guylain1,2,3*, Beya Kabongo François2, UICC3, Kisile Mikuo Olive2, Lebwaze Massamba Bienvenu2, Mutombo Kabamba André1 and Kabongo Mpolesha Jean-Marie2
1Official University of Mbuji-Mayi: Mbujimayi University Clinics, République Démocratique du Congo
2University of Kinshasa, Faculty of Medicine: Department of Anatomy and Pathology, République Démocratique du Congo
3Union for International Cancer Control (UICC), République Démocratique du Congo
Received Date: 24/07/2024; Published Date: 17/10/2024
*Corresponding author: Nsumpi Tshimanga Guylain, Official University of Mbuji-Mayi: Mbujimayi University Clinics; University of Kinshasa, Faculty of Medicine: Department of Anatomy and Pathology; Union for International Cancer Control (UICC), République Démocratique du Congo
Abstract
Background: The description of the histopathological aspects of rhabdomyosarcomes dates back to 1900 by Horn and Enterline and has allowed to group the MSR into several types; embryonic with its subtypes (botryoid), alveolar and pleomorphic. In our environment, studies on RMS are rare or non-existent.
Objectives: Determine the prevalence of RMS; their histopathological types, clinical aspects and socio-demographic profile of children affected by RMS.
Methods: The study is descriptive, retrospective, multicenter and documentary. It was carried out over a period of 13 years (from 1 January 2010 to 31 December 2023). Carried out in the main laboratories of the city of Kinshasa. It targeted all children aged 0 to 19 years with confirmed diagnosis of RMS based on analyses made on biopsies and/ or pieces of excisions in the aforementioned laboratories. The sampling was exhaustive and random.
Results: In this study, 56 cases of rhabdomyosarcoma were reported, a prevalence of 30.93%; sex-ratio: 1. In the age group of 6 to 11 years girls were most affected, 39.3% and boys were more affected at 18 and over, 42.9%. Embryonic rhabdomyosarcomes (32.1%) were the most observed histopathological type followed by fusiform cell rhabdomyosarcoma (23.2%). The RMSE botryoids reach more children between 0 to 5 years old or 55.6% and fusiform cells between 6 to 11 years (37.5%) p-value is 0.671. The ERMS Botryoid is the female’s prerogative in 42.9% of cases and versus fusiform cell RMSE which reaches the male in 28.6% of cases.
The preferred location of children’s rhabdomyosarcomas is the head: ocular 15% and extraocular 26.6%. The ERMS botryoide is more extraocular localization 37% and thoracic limbs 33.3%, while fusiform cell RMS are located at pelvic limbs 40%.
Conclusion: Rhabdomyosarcomas is a cancer that exists in the Congolese child, as well highlights its prevalence.
Keywords: Rhabdomyosarcome, histopathology, laboratories, anatomopathological, children, Congolese, Kinshasa
Introduction
The description of the histopathological aspects of rhabdomyosarcomes dates back to 1900 by Horn and Enterline and has allowed to group the RMS into several types; embryonic with its subtypes (botryoid), alveolar and pleomorphic [1]. It was necessary to wait until 2017 to see the work of Saro P and al add to this description entities such as fusiform and anaplastic cell RMS, Also, it provides a better understanding of ARMS [1].
Rhabdomyosarcomas are a group of malignant solid tumors of the mesenchymal child with a strong propensity for myogenesis and in which more than one entity with common neoplastic striped muscles [1-3]. Their preferential location is in the areas where there are normally skeletal striated muscles, but also in sites where these muscles are unimagined [1,3,4]. Their prognosis is poor depending on age, location and histological type similar to alveolar types in adolescents [5]. More than one author reported that in 10 to 33% of cases rhabdomyosarcomas are associated with genetic abnormalities or risk factors sometimes with syndromes of genetic predisposition, the cases of syndromes below are eloquent in this regard: Li-Fraumeni syndrome; Neurofibromatosis type I; Rubénstein Taybi syndrome; Wiedmann-Beckwith syndrome; Costello syndrome; Noonan syndrome; Basic Noevus syndrome of the Gorlin [1]. This suggests that at the molecular level, the child’s rhabdomyosarcoma, have varieties that subdivide them into different groups mainly on both histopathological and genetic aspects which differentiate them from those of the adult [1].
Thus, the mastery of these characteristics should ipso facto, allow the understanding and improvement of the management of this cancer in children, Consequently, their lack of knowledge would impact on the diagnostic approach as well as on their adequate management. Hence the questions below invite our reflection to better understand or grasp the need and relevance of this research; What is the prevalence of RMS in children in Kinshasa? -What is the morphological and sociodemographic profile of children with rhabdomyosarcomas? What are the clinical characteristics of the child with rhabdomyosarcoma? From these pivots, the objectives pursued by this research are summarized as follows: Determine the prevalence of RMS; their histopathological types, clinical aspects and socio-demographic profile of children affected by RMS.
Patients and Method
The study was carried out in the main Pathological Anatomy Laboratories of the City of Kinshasa (Laboratory of the University Clinics of Kinshasa, Laboratory of pathological anatomy of the National Institute for Biomechanical Research INRB in acronym, Department of Anatomy and Pathological Cytology LEBOMA, Laboratory of Pathological Anatomy of the Hospital Center MONKOLE).
It targeted all children aged 0 to 19 years with confirmed diagnosis of RMS based on analyses made on biopsies and/ or pieces of excisions in the aforementioned laboratories. The documentary and/or logistical support consisted of data collection sheets, biopsy pathological analysis request forms, reports of samples, The slides, paraffin blocks and for reading slides, the optical microscope of the brand Olympus and Meitz were used.
The study is retrospective, descriptive, multicenter and documentary. It was carried out over a period of 13 years (from 1 January 2010 to 31 December 2023).
The sample was comprehensive simple random and 56 cases of RMS that met the eligibility criteria for the study were selected from 181 childhood cancers from 2380 cancers the results of the studies were also presented in the US. The study parameters used for the analysis were: the socio-demographic profile of children with RMS; the location of RMS, clinical signs; the anatomopathological data of the RMS. Data was entered into Excel and analyzed using SPSS Software 29.0.10 dated 12/9/2022.
Anonymity and medical confidentiality were strictly observed in accordance with the Helsinki and Taepei declaration.
Results
The prevalence
In this study it was listed 2380 cancers in general, of all these cancers the cancers of the child represented a proportion of 181 cases or 2,35% and 181 childhood cancers 56 cases of rhabdomyosarcoma were isolated, a prevalence of 30.93%. Rhabdomyosarcoma affects both sexes equally, sex-ratio: 1.
Distribution of patients according age and sex
Table I: Distribution of patients according age.
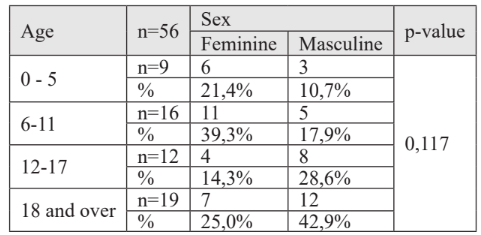
It is clear from this table that girls were most affected in the age group of 6 to 11 years, 39.3%, and boys were more affected in the age group of 18 and over, 42, 9 %. This link is statistically not significant
Distribution of patients according to clinic
In our series 19.6% of cases had pain as a symptom, 73.2% of the cases no symptoms were mentioned in the various documents. 93% of the cases of children suffering from rhabdomyosarcomas had a fleshy mass and this was ulcerated in 3.6% of the cases.
Distribution of patients according localization
Table 2: Breakdown of patients according localization.
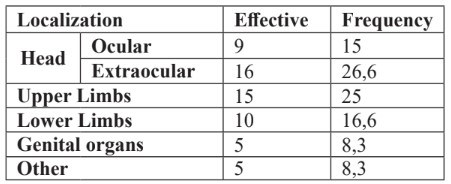
The preferred localization of children’s rhabdomyosarcomas is the head: ocular 15% and extraocular 26.6%.
Patient distribution according histopathological types of rhabdomyosarcomas
Table 3: Distribution of patients according diagnostic types of rhabdomyosarcomas.
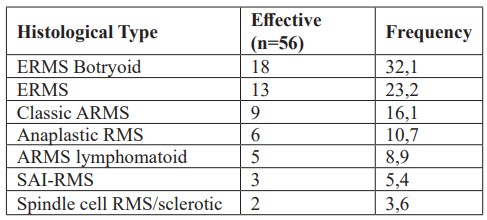
This table shows that embryonic rhabdomyosarcomas (32.1%) were the most observed histopathological type followed by spindle cell rhabdomyosarcoma (23.2%).
Distribution of patients by histological type and age
Table 4: Distribution of patients according histological type and age.
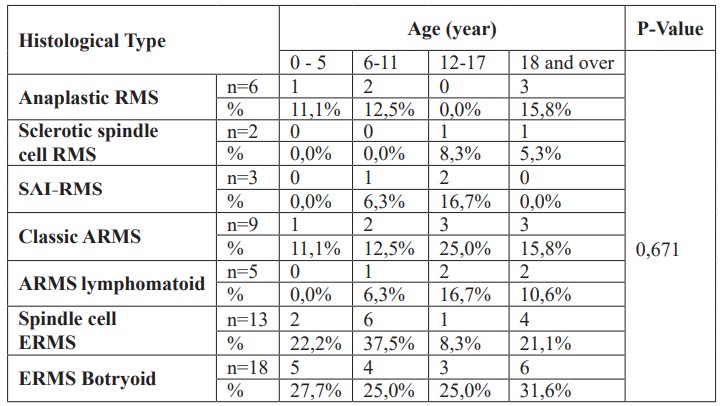
This table shows that the botryoid ERMS reach more children between 0 to 5 years 55.6% and fusiform cells between 6 to 11 years (37.5%) p-value is 0.671.
Distribution of patients according histological type and sex
Table 5: Distribution of patients according histological type and sex.
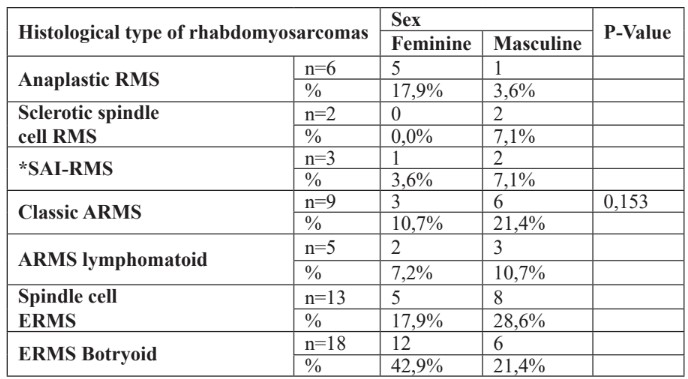
It is clear from this table that the ERMS botryoid is the female’s prerogative in 42.9% of cases and versus fusiform cell RMSE which reaches the male sex in 28.6% of cases.
Distribution of patients according localization and age
Table 6: Distribution of patients according localization and age.
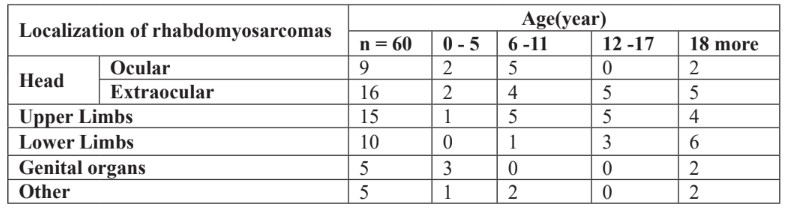
This table shows that ocular localization was observed in children aged 6 to 11 years (5/9 patients), extraocular localization was observed in children aged 12 to 18 years (10/ 16 patients).
Patients according localization and sex
Table 7: Distribution of patients according localization of RMS and sex.
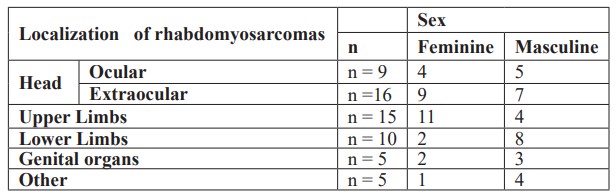
The RMS was more localized to the upper limbs 11/15 and extraocular 9/16 in female children. The ocular localization is even in both sexes.
Distribution of patients according localization and histological type of rms
Table 8: Distribution of patients by location and histological type.
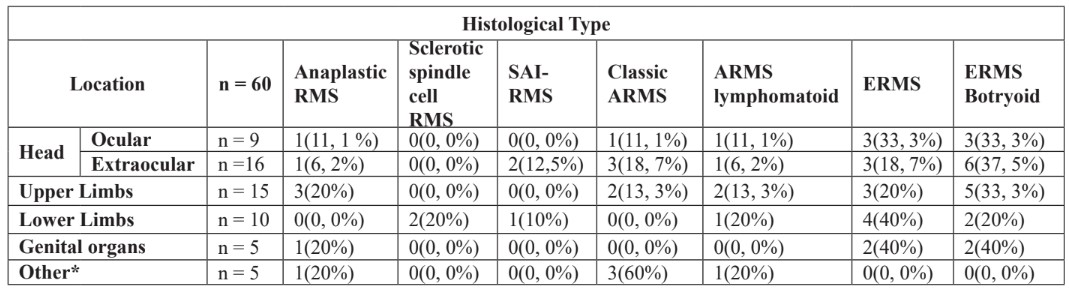
It is clear from this table that the ERMS botryoid are more of extraocular localization 37% and thoracic members 33,3%, while fusiform cell RMS are located at 40% of the lower limbs.
Discussion
Frequency of Rhabdomyosarcomas
The frequency of rhabdomyosarcoma in our series was 30.95% or 56 children out of 181 children with cancer during the study period. This is similar to the findings of Mandeville H.C et al [5] and Ingley K.M et al [6], who noted in their studies that rhabdomyosarcomas accounted for 40-50% of childhood cancers. The literature reports that MSR accounts for 60 to 70% of paediatric solid tumors [2]. The difference found would be explained by the different study scope and sample sizes. Our study was only targeted to children whose samples were taken to the different laboratories where the study was carried out, whereas most studies in the literature are conducted in the general population.
Socio-Demographic Characteristics
RMS affected both sexes equally, with a bimodal peak between 6 and 11 years 28.6% followed by 18-year-olds 33.9%. The median age was 12 10 years. Juan P et al [7] noted that rhabdomyosarcomes was more common in Caucasian boys with a peak of bimodal age between 2 years and 6 years and 10 to 18 years, and additionally over 80% of cases were diagnosed before 14 years. The bimodal peak was also reported by Ingley K.M et al [6] they found that rhabdomyosarcomas were more common in children under 10 and adolescents around 16 to 19. Other authors reported a predominance of males with an average age of 7 1.8 years [10].
Patient Clinic
Pain was the symptom of about 19.6% of children in our series; the physical examination had reported the presence of a mass as a clinical sign in 92.6% of cases. The symptomatology or clinical signs of rhabdomyosarcomas have been discussed by some authors. Indeed, Pradeep B et al [8], also reported that 75% of rhabdomyosarcomas were manifested by a mass, unlike our results, pain was more common in their study in 75% of cases. Then Smaranda D et al [9] reported that in a proportion of 60%, rhabdomyosarcomas were revealed as masses and pain was the symptom observed in 28% of cases. The general symptomatology of rhabdomyosarcomas depends on the location of the primary tumor. Sometimes the secondary symptoms come from the compressive effect of the mass, this is how one can have: exophthalmia for the RMSE of the head, scrotal swelling for the paratesticular RMS [7].
Localization of Rhabdomyosarcomas
Rhabdomyosarcomas were located in the head, with a 26, 6% extraocular predominance in girls aged 12 to 18 years. The upper limbs were the second most common site, accounting for 25 % of girls in the same age group. In 16, 6 % of cases, rhabdomyosarcomas located in the pelvic limbs in the boys aged over 18 years. Pradeep B et al [7; 8], in their study also reported that rhabdomyosarcomas were more likely to be located in the head but more likely to be ocular (50 % per eye). On the other hand, Smaranda D et al [7; 9], stated that 48 % of rhabdomyosarcomas were located in the urinary tract, 32% in the trunk and extremities, and only 8 % in head.
Histological Types of Rhabdomyosarcoma
Embryonal rhabdomyosarcoma was the most common histological type reported in our study, including 32,1% botryoid and 23,2 % spindle cell cell/sclerotic subtype accounted for only 3,6 % of cases. Classical alveolar rhabdomyosarcoma represented 16, 1 % and the lymphomatoid subtype 8, 9 %. Our results are similar to those found by Smaranda et al, Juan P et al [2; 7; 10] who reported in their studies respectively 80 %, 75 % and 6, 75 % of embryonal rhabdomyosarcomas, 32 %, 4 % and 2 % of alveolar rhabdomyosarcoma. The incidence of spindle cell/sclerotic rhabdomyosarcoma in our series in close to that reported in their literature, which is 5 to 10 % according to the WHO [5].
Histological types according age and sex
The types of rhabdomyosarcoma most frequently in children in Kinshasa were embryonal rhabdomyosarcoma of the botryoid type (42.9 %) in girls, spindle cell rhabdomyosarcoma (28,6 %) in the boys (sclerotic subtype predominating in girls) and classic ARMS (21,4 %). The statistical relationship between histological type and sex was no-significant (p-value= 0,153). In contrast to our study, the 2013 WHO classification states that spindle cell/sclerotic RMS affects children and adults indiscriminately in both sexes with a mal predominance [5].
ERMS subtype botryoid was observed in children aged 18 years and over (31, 6 % and in the 0 – 5 age group (27, 7 %°. Spindle cell rhabdomyosarcoma affected more children in the 6 to 11 age group, while classic ARMS was seen in the 12 to 17 age group. The statistical association between histological type and age was no-significant (p-value 0, 671). Ingley K.M et al [11] in his series, reported that rhabdomyosarcoma is more common in children under 10 years of age and adolescents age 16 to 19 years. In contrast to our series, they also specified that ERMS predominated in children aged 0 to 5 years and was rare in adolescents. Juan P et al [7] state that over 80 % of cases are diagnosed before the age of 14 and that age peaks are related to histological type. Thus, ERMS are observed in early childhood and ARMS reaches children in late childhood and adolescence.
Histological types and localization
Embryonal rhabdomyosarcomas were located in the head, (37, 5 %) extraocular (33, 3 %) ocular, upper limbs (33, 3%), lower limbs (20 %) and genitals (40 %). The spindle cell rhabdomyosarcomas were located almost everywhere in the body: (40 %) in the pelvic limbs, (20 %) in the thoracic limbs, (40 %) in the genitals, (33, 3 %) in the eyes and 18, 7 % in the extraocular. The spindle cell/sclerotic subtype was localised to the lower limbs (20 %). Classic alveolar rhabdomyosarcomas were found in the head (11, 1% ocular, 18, 7 % extraocular), upper limbs (13, 3 %) and other locations (60 %). The lymphomatoid type of ARMS was most frequently observed in the thoracic limbs (13, 3 %). Anaplastic rhabdomyosarcoma (20 %) and SAI (8 %) were located in the thoracic limbs and head respectively. Our results corroborate those reported by Juan P et al [7; 11] who said that, ERMS were located in the head, genitals and urinary tract and that ARMS were located in the extremities and trunk. For Juan et al [7; 11] in his study, ESMR included the botryoid and spindle cell subtypes, whereas in our series we have separated them for didactic reasons. While they speak of the trunk as a separate location, in our study the trunk is included in other locations. On the other hand, Smaranda D et al [9] note that (48 % of rhabdomyosarcomas were located in the urinary tract, trunk and extremities in 32% of cases, head and neck 8 % in the peritoneum.
Appendices: Breakdown of patients by sex; age and clinic
Breakdown of Patients by Gender
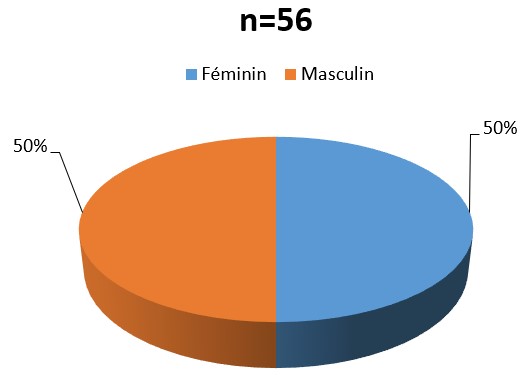
Figure 1: This figure shows that RMS reaches both sexes equally.
Distribution of patients according clinic
1. Breakdown of patients by symptomatology
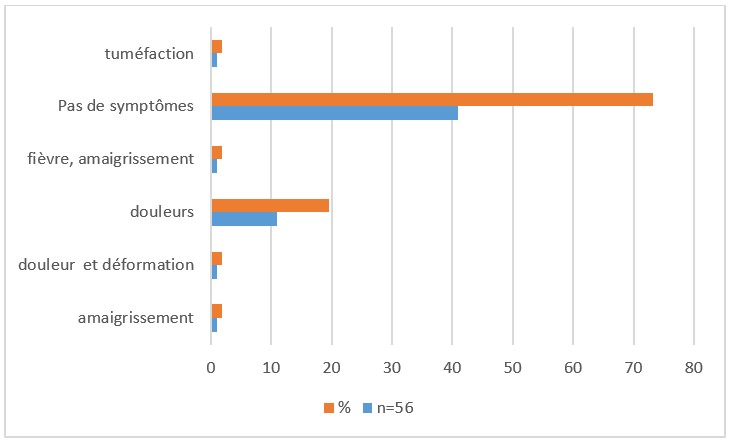
Figure 2: Shows that 73, 2 % of symptoms were not reported with pain the most frequently reported symptom at 19, 6 %.
2. Breakdown of patients by clinical signs
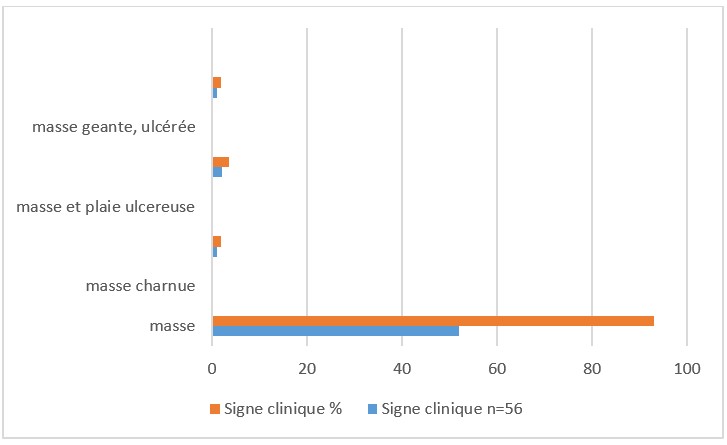
Figure3: shows that 93 % appear as a fleshy mass and 3, 6 % are ulcerated.
Distribution of patients by age
Breakdown of patients by age
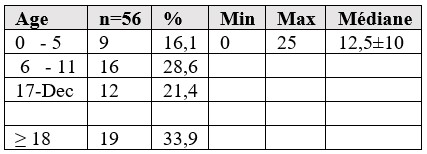
This table shows that children aged 18 years are the most affected by rhabdomyosarcoma 34 % followed by the 6 to 10 age group 29%, standard deviation 12,5±10 years.
References
- Panda SP, et al. Diagnosis and Management of rhabdomyosarcome in children and adolescent: ICMR Consensus Document, Idian J. Pediatr, 2017; 84(5): 393-402.
- Leila H. Etude du rhabdomyosarcome chez l’enfant dans le service d’oncologie et hématologie pédiatrique (Thèse N° 171) Université Cadi Ayyad, Maroc, 2017; 11-49.
- Micael CH. Fact sheet on Childhood Rhabdomyosarcoma [The cancer association of South Africa, 2022
- Adil A, Mohammed K, Abibou N, Karim EL, Abdal JA. Rhabdomyosarcome Cranio-facial de l’adulte: Un cas de mauvais Pronostic, PAMJ, 2018; 30: 3.
- Mandeville HC. Radiotherapy in the Management of Childhood Rhabdomyosarcoma. Elsevier, Clinical Oncology, 2019; 31: 46-470.
- Ingley KM, Cohen SG, Gupta AA. Systemic Therapy in Paediatric type soft tissue Sarcoma. Curr Oncol, 2020; 27(61): 6-16.
- Juan P Guurria, Roshni D. Rhabdomyosarcoma and Extraosseous Ewing Sarcoma. Children, 2018; 5: 165.
- Pradeep B. Orbital rhabdomyosarcoma in the Paediatric Population: A perspective, observational Study from Mid-West Nepal. Academic Journal of Health, 2022; 37(3): 108-112.
- Smarada D, Burlea M, Igrid M, Aprodu SG, Doina M, Claudia O. Childhood rhamyosarcoma : Anatomo-clinical and therapeutic study on cases Surgical Implications. RJME, 2013; 54(3): 531-537.
- Chidi F, Rouas L, Lamalin N. Spindle cell/ screrosing Rhabdomyosarcoma in Childhood: About a case and review of the Literature. Saoudi Journal of Pathology and Microbiology, 2021; 6(4): 125-127.
- Erin RR, James RA, Douglas SH, Stephen X. Skapek et al. The World Health Organization Classification of Skeletal Muscle Tumors in Pediatric Rhabdomyosarcoma: A Report from the children’s Oncology Group. Arch Pathol Lab Med, 2015; 139(10): 1281–1287.
- Sila D, Jay GR, Tushar D, Santamu P. Embryonal rhabdomyosarcoma: A rare oral tumor. Journal of Oral and Maxillofacial Pathology, 2016; 20: 527-531.
- Juri F, Anastasia ML, Markus K, Patrick G, Alexender F, Jean P, et al. Biliary Rhabdomyosarcoma in Paediatric Patient data. Frontiers in Oncology, 2021; 11: 701400.
- Evi S, Matias JS, JIN Y, Sabin S, Sabina H, et al. Serum and Glucocorticoide Inducible Kinase1-Sensitive Survival, Proliferation and Migration of Rhabdomyosarcoma cells. Cell Physiol Biochem, 2017; 43: 1308.
- Makimoto A. Optimising Rhabdomyosarcoma Treatement in Adolescents and Young Adults. Cancers, 2022; 14: 2270.
- Loi WH, Wen-Feng Wu, Jin-Yang, Young-Hui, Jie-Hui L, Jun-Xin. Alveolar Paratesticular Rhabdomyosarcoma Mimicking Epididymitis. Medecine, 2018; 97: 25.
- Jack S, Marielle FY, Javed K. Paediatric Rhabdomyosarcoma. Crit Rev Oncog, 2015; 20(3-4): 227-243.
- Cora AR, Andriew DW, William S, Melvin L, Ganapati S, Erin RR. Refractory Alveolar Rhabdomyosarcoma in 11-years-old male. Cold Sprind hard Mol Case Stud, 2021; 7: 0005983.
- Ashlesha J, Sajitha K, Padmaraj H, Vikram S. Spindle cell Rhabdomyosarcoma in Adult: A rare case report.J.Oral Maxillo Fa Pathol, 2022; 26: S103-6.
- Sabire NJ, Melone M. Myogenin and Myo D1 expression in paediatric rhabdomyosarcoma. J.clin Pathol, 2003; 56: 41-146.

