Covid-19 Outbreak Investigation among Healthcare Workers in a Low-Risk Medical Area of a Tertiary Care Hospital
Saad Bin Zafar Mahmood1, Aysha Almas1, Zaib un Nisa1, Aisha Jamal1, Sana Hirani2 and Syed Faisal Mahmood1,*
1Department of Medicine, Aga Khan University Hospital, Pakistan
2School of Nursing, Aga Khan University Hospital, Pakistan
Received Date: 22/07/2024; Published Date: 14/10/2024
*Corresponding author: Dr. Saad Bin Zafar Mahmood, Senior Instructor, Department of Medicine, Diplomate American Board of Infectious Diseases and Internal Medicine, Aga Khan University Hospital, Stadium Road, Karachi, Pakistana
Abstract
Background: Healthcare Workers (HCWs) have been assumed to be a cause of nosocomial outbreaks themselves as they are at the interface between healthcare setting and the community and not limited to a single area. Covid-19 nosocomial infections are more likely to occur in areas where prevalence of infection is high, and hypothetically the spread of infection is low among HCWs in non-isolation ward areas where such patients are not admitted. We present an outbreak investigation report from a low-risk medical ward and the factors associated with the outbreak.
Methods: A formal outbreak investigation was initiated in a low-risk medical zone of a tertiary care hospital when two HCWs from the low-risk area turned positive for Covid-19. All HCWs including nurses and physicians who are involved in direct patient care were included from these two areas for investigation except those who were on leave. The report included participants working in the low-risk zone from 16th April 2020 to 30th April 2020. The total number of HCWs in the two wards was determined from the ward heads and the monthly roster. A predesigned pro forma was filled after acquiring the data and serial coding was employed to maintain anonymity and confidentiality. The basic steps of epidemiologic field investigations as set by the Center for Disease Control and Prevention (CDC) were adapted for investigation. SPSS V22.0 was used for analysis. An epidemiological curve and a swimmer chart were plotted to illustrate the course of the epidemic to identify the index case. The attack rate was also calculated and other risk factors for a hospital outbreak were also investigated.
Results: Twenty HCWs tested positive for Covid-19 out of 166 giving an attack rate of 12%. The Majority were registered nurses (n=15) with a preponderance for male gender (n=12). Myalgias (n=11) and fever (n=10) were the common presenting symptoms. Three HCWs had a history of high-risk contact with a Covid-19 positive case. The origin of the outbreak was presumed to be from the secondary ward where two HCWs reported infection while three patients tested positive around the same time in both wards. The common physical risk-defining activity associated with high-risk contact was either not wearing a gown (n=18) or prolonged contact with a patient who was not wearing a facemask (n=18). Lack of physical distancing and taking meals together were the major behavioral risk factors increasing the risk of Covid-19 transmission (n=18).
Conclusion: This Covid-19 outbreak investigation reports an attack rate of 12% from a low-risk medical unit. The outbreak’s likely origin was from patients who were admitted with other medical or surgical conditions and further triggered by suboptimal personal protective equipment practice and lack of physical distancing in HCWs.
Keywords: Covid-19, outbreak investigation report, low-risk hospital area, healthcare workers.
List of abbreviations: AGPs - Aerosol-Generating Procedures; CDC - Center for Disease Control and Prevention; Covid-19 - Coronavirus disease 2019; ER - Emergency Room; HCWs - Healthcare Workers; RT-PCR - Reverse Transcription – Polymerase Chain Reaction; PPE - Personal Protective Equipment; SPSS : Statistical Package for Social Sciences
Introduction
Healthcare Workers (HCWs) have been postulated to be causing large nosocomial outbreaks themselves since they are not confined to a single area and are at the interface between healthcare setting and the community [1,2]. Nosocomial outbreak investigations help to identify the source of infection, prevent additional cases, and increase our knowledge of disease control to face future outbreaks [3,4]. Covid-19 pandemic, that initially began as pneumonia of unknown origin in December 2019 in Wuhan, China has similar symptoms and transmission risks to that of influenza [5]. Hence, it is important to identify outbreaks early, contain them, and prevent person-to-person spread until identification of the cause of the outbreak can be determined [4].
Covid-19 nosocomial infections are more likely to occur in areas where prevalence of infection is high, for example the wards housing most of the Covid-19 patients, and hypothetically the spread of infection is low among HCWs in ward areas where such patients are not admitted. We recently had an outbreak of Covid-19 infections in a low-risk vicinity of the hospital. Here we present the outbreak investigation report from a low-risk medical ward and look at the risk factors linked to the outbreak of Covid-19 in our low-risk area.
Methods
Study design, setting and participants
A formal outbreak investigation was initiated in a low-risk medical zone of a tertiary care hospital when 2 HCWs from the low-risk area turned positive for Covid-19. A low-risk area (GREEN ZONE) was defined as the area of the hospital reserved for patients who were either not suspected for Covid-19 and were screened negative based on symptoms from the Emergency Room (ER) or included those patients who were initially suspected of Covid-19 from ER but later tested negative for Covid-19 using reverse transcription - polymerase chain reaction (RT-PCR) test. In our hospital all patients who were Covid-19 positive or who were suspected of Covid-19 were housed in the Covid-19 diagnostic and testing Zone (Red Zone) (on separate floors). Our study looked at two low-risk areas: primary internal medicine ward and the adjacent secondary medicine ward. All HCWs including registered nurses, health care assistants, physicians (residents, faculty, or interns) who are involved in direct patient care were included from these two areas for investigation except those who were on leave. The report included participants working in the low-risk green zone from 16th April 2020 to 30th April 2020.
Data was acquired from the Covid protector, persons designated by the hospital administration from every department to assess all HCWs for possible exposures with SARS-CoV-2 either from other patients, from co-workers, or even community in some cases. The total number of HCWs in the two wards was determined from the ward heads and the monthly roster. A predesigned pro forma was filled after acquiring the data and serial coding was employed to maintain anonymity and confidentiality.
Outbreak investigation method
The basic steps of epidemiologic field investigations as set by the United States Center for Disease Control and Prevention (CDC) were adapted for investigation [6]. The diagnosis of Covid-19 was based on a confirmed nasopharyngeal swab RT-PCR test for SARS-CoV-2. HCWs with a positive test were screened for any positive contacts outside the hospital and if they had worked in the red zone in the last 15 days. The contacts within the hospital were also screened and their interactions with patients and other HCWs were noted to determine the risk of infection. Nosocomial Covid-19 infection for HCWs was defined as having an onset of symptom or positive test after having a history of contact in hospital with either a positive HCW or a patient [7].
An epidemiological curve and a swimmer chart were plotted to illustrate the course of the epidemic to identify the index case. Apart from this, other risk factors for a hospital outbreak were also investigated; like risk of exposure, details of Personal Protective Equipment (PPE) worn at the time of exposure, the proximity of contact (a close contact being defined as a contact within 2 meters of the index case for a cumulative time of >15 min or had performed Aerosol-Generating Procedures (AGPs) without ‘appropriate’ PPE), lack of physical distancing, non-availability of changing rooms, and eating together without masks and physical distancing. Exposure was defined high-risk exposure when the HCW was not wearing the appropriate PPE for a long duration (> 15 minutes) encounter at less than 2 meters. Any other exposure was defined as low exposure.
Statistical analysis
Statistical Package for Social Sciences (SPSS) V22.0 was used for analysis. Mean (SD) was reported for quantitative variables while frequency and percentage were used for qualitative variables. Chi-square test was used as appropriate and a P value of < 0.05 was significant. The attack rate (Number of HCWs at risk who developed the disease/total number of HCWs at risk) was calculated.
Results
A total of 166 (121 from the primary medicine ward and 45 from the secondary medicine ward) HCWs underwent testing for Covid-19. Twenty HCWs tested positive during the outbreak period of 2 weeks, giving an attack rate of 12.05 %. The mean (SD) age was 27.5 (4.2) years. As soon as the outbreak was confirmed the infection control department and the chief medical officer were informed. It was decided to test all patients admitted in the low-risk area along with all HCWs working in that area for Covid-19 infection. Majority (n=12) were males. Registered nurses (n=15) were affected more frequently. Myalgias (n=11) and fever (n=10) were the common presenting symptoms while 3 HCWs were asymptomatic. Three HCWs had a history of high-risk contact with a Covid-19 positive case. Table 1 shows a detailed description of baseline characteristics.
An epidemiological curve was plotted (Figure 1) with number of cases against the date of symptom onset to see the progression of the illness over time. It showed that the maximum number of HCWs having symptoms on any given day was 4 and that the symptoms started initially in the patient and HCWs of secondary medicine ward and then propagated over to the primary medicine ward. A swimmer chart (Figure 2) was designed to identify the index case based on the history of symptoms and exposures in different HCWs and patients. Two HCWs started having symptoms at the same time on 17th April 2020, one of them was from the secondary ward the other was looking after patients both in secondary and primary low-risk green zone. Additionally, one patient from the secondary ward developed symptoms prior to the development of symptom in the two HCWs while another patient in the primary ward developed symptoms four days later. Another patient from the primary ward was later identified as having Covid-19 on routine testing prior to a surgical procedure (see Appendix). Hence, it can be hypothesized that the index case was either one of the HCW mentioned above or the patient in the secondary ward.
Factors associated with the outbreak in health care professionals
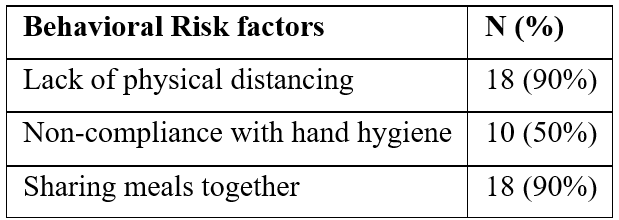
Further exploration was conducted of the reasons for the outbreak of Covid-19 in the low-risk green zone. The common physical risk-defining activity associated with high-risk contact was either not wearing a gown (n=18) or prolonged contact with a patient who was not wearing a facemask (n=18) (Table 2). Lack of physical distancing and taking meals together were the major behavioral risk factors increasing the risk of Covid-19 transmission (n=18) (Table 3). Analyzing differences in practices and activities between both genders, it appeared that both males and females had similar infection control practices when dealing with patients or performing various procedures except when performing AGPs where five males did not follow proper protocol when doing procedure while all females were wearing adequate PPE (p=0.05).
Based on these findings it was hypothesized that lack of practice with the correct PPE and lack of physical distancing, and possibly suboptimal screening of patients for Covid-19 in ER contributed to this outbreak of Covid-19 in a low-risk green zone of the hospital.
Table 1: Baseline characteristics and presenting features of Covid-19 positive healthcare workers.
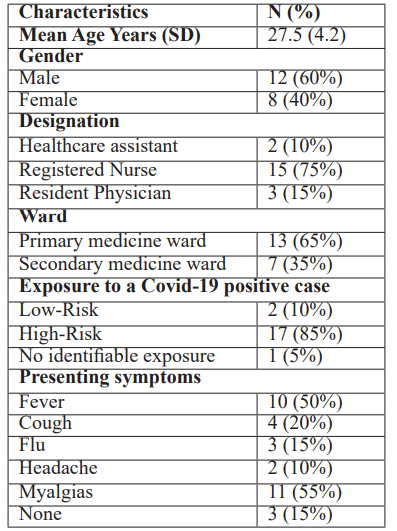
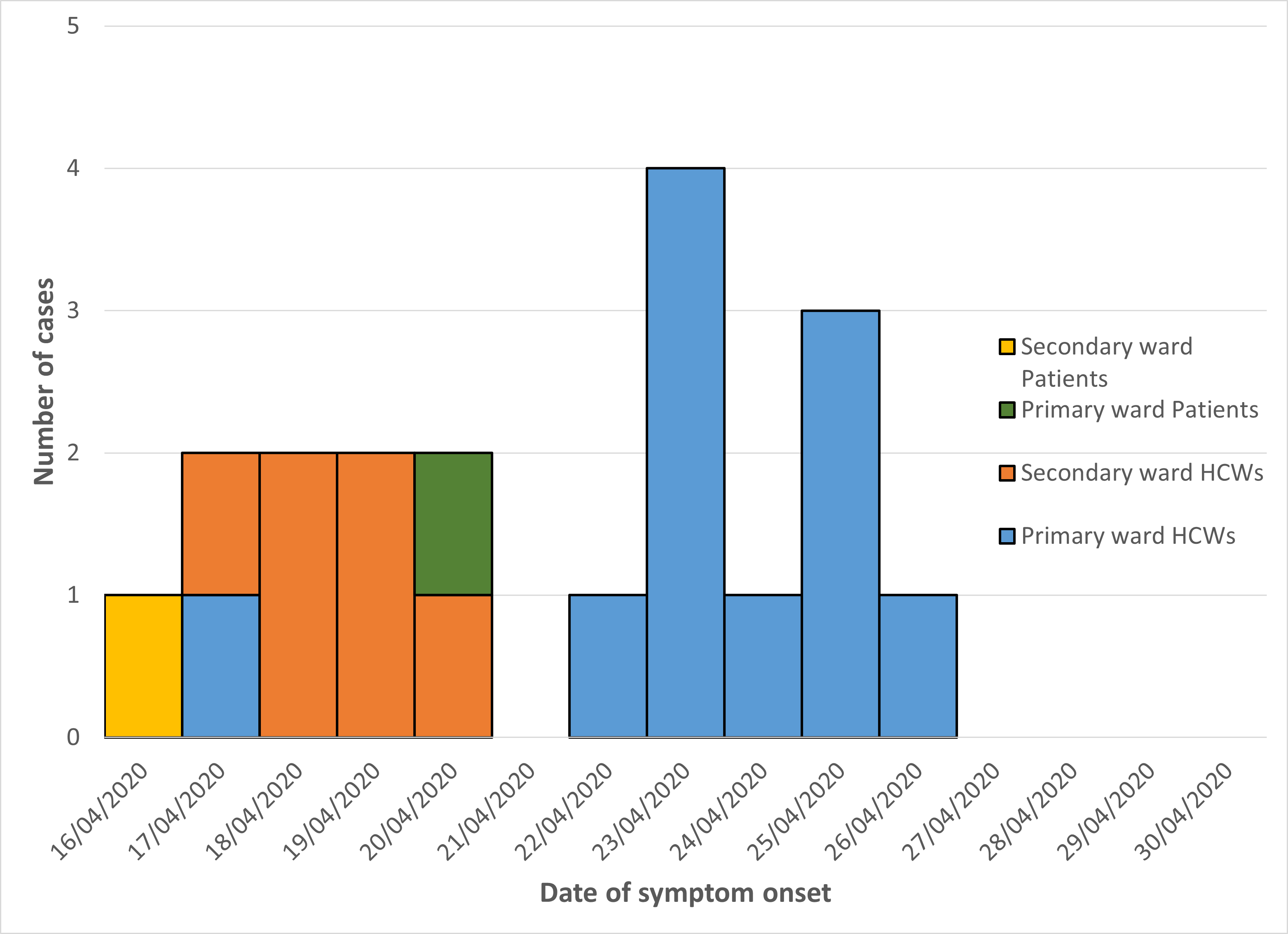
Figure 1: Epidemiological curve with number of cases against the date of symptom onset to see the progression of the illness over time.
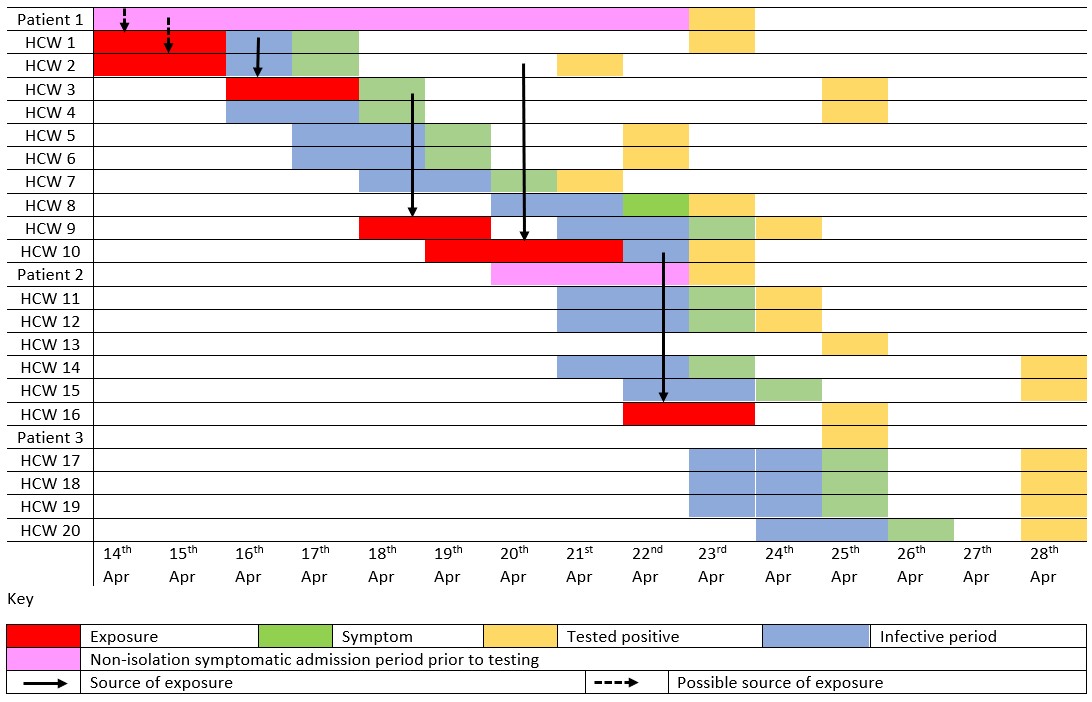
Figure 2: Swimmer chart to identify the index case based on the history of symptoms and exposures in different HCWs and patients.
Table 2: Physical risk-defining activities of healthcare workers in the low-risk ward.

Table 3: Behavioral risk-defining activities among healthcare workers in the low-risk ward.
Discussion
We report from this Covid-19 outbreak investigation in HCWs from a low-risk area of the hospital that the outbreak resulted from possible suboptimal screening of asymptomatic patients with Covid-19. The outbreak was further triggered due to lack of physical distancing and sharing meals together among HCWs. We also noticed that both the physical and behavioral risk factors mentioned above were more prevalent among nurses as compared to resident physicians.
A large meta-analysis on nosocomial Covid-19 confirmed and near-outbreaks consisting of 22 studies from United States, Europe, and Asia [1], focused more on nursing homes rather than HCWs. The attack rate from this meta-analysis concerning HCWs ranged from 2.5% to 17%. However, there are only few reports of Covid-19 outbreak in a low-risk area of the hospital [8-10] with attack rate being reported as low as 2.5% in the study from the United States [8] and 5.2% from Germany [9].
An Italian study showed that with proper following of the infection protocols, the prevalence of SARS-CoV-2 is just 0.43% among all HCWs working at a healthcare institution [11]. Our study showed an attack rate of 12.05% which falls within the figures reported in the studies mentioned above. However, our findings are specifically from a low-risk area in a hospital. This might imply that these numbers are slightly higher because they are from a low-risk area. The reasons behind this relatively high attack rate are inappropriate use of PPE in the early days of the pandemic due to lack of awareness thus leading to variation in practice. Secondly, HCWs working in low-risk areas might have been illusioned that they might not contract Covid-19 as they are in low-risk areas. Thirdly, the standard infection control practices in the low-risk area were of course less stringent compared to the high-risk red zone. Furthermore, some patients with minimal suspicion of Covid-19 or those who were either asymptomatic or screened preoperatively can be the source of outbreak in low-risk green zone. Finally, patients may have tested negative for the SARS-CoV-2 PCR initially as they might have been in the incubation period. This was also seen in a study from Korea where the index case behind the outbreak initially tested negative on admission but later developed symptoms and turned out to be positive for Covid-19 [12].
The chain of transmission of Covid-19 in our ward likely started from a patient who turned out to be positive for Covid-19 and was probably missed in the initial screening. Once HCWs were infected from the patients, further propagation of Covid-19 in the ward was more likely due to transmission between HCWs rather than due to interaction between HCWs and patients. However, during this period a similar high infectivity rate was not seen in the patients admitted in the low-risk ward. Literature review shows that the healthcare community has also been pondering on the fact that the risk of Covid-19 transmission to HCWs is more during peer-to-peer interaction rather than during direct patient care [1,13]. Unfortunately, like our study, most of the other studies were also unable to establish the sequence of infection in patients and hence were unable to identify the index case [14].
Our study showed that most of the individuals affected by this outbreak were nurses. This may be because the total number of nurses working in the medicine ward was far greater than that of physicians. Moreover, limited eating areas for nurses could be the reason for nurses’ inability to maintain physical distancing while taking meals. Studies done globally show a similar trend [9,14], except a study from Wuhan which was dominated by physicians as the source of infection was a multidisciplinary meeting in that study [15]. No significant differences were observed in the practices of the infected male and female HCWs. Performing AGPs was the only activity where the male population did not properly follow the PPE protocols. However, since the number of patients turning out positive for Covid-19 was small, the significance of this difference remains unclear.
The reasons behind nosocomial outbreaks in low-risk areas can be complex. Contributing factors can include suboptimal hand hygiene or other infection control practices by HCWs; inadequate laboratory results or inappropriate triaging; incorrectly engineered heating, ventilation, and air-conditioning systems; or even misinterpretation of existing infection control guidelines [16]. The common factor in our study which predisposed our HCWs to be classified as a high-risk contact was lack of wearing a gown while interacting with either patients or other HCWs and lack of wearing a face mask by those patients and HCWs who were symptomatic for Covid-19. Whether it involves facemask compliance of patients or the compliance of PPE by the HCWs, the overall compliance of PPE and other infection control practices in a healthcare setup has remained an issue globally [17]. Literature also shows that major risk factors for other nosocomial outbreaks are lack of compliance to PPE especially masks, and proper hand hygiene [18]. Studies from Massachusetts and North Carolina showed that chances of Covid-19 transmission among HCWs were greater from an unmasked exposure to another HCWs rather than an exposure to a known infected patient [18,19].
Even with the advent of vaccines, the primary prevention technique for the Covid-19 pandemic still revolves around physical distancing [20]. There is no doubt that physical distancing also has an important part to play in a healthcare setup [21] It is ideal to have six feet between HCWs when rounding on patients or performing tasks on computers. Our investigation showed that lack of physical distancing was one of the major behavioral risk-defining activities among HCWs, with the other being sharing meals. Mealtimes are regarded as a restful and stress-relieving period and sharing of meals is often practiced all around the world. Though sharing of meals and eating out in restaurants has been seen to cause an increase in Covid-19 transmission [22], only one study has commented on the lack of physical distancing while eating unmasked as a risk factor for Covid-19 transmission among HCWs [18].
Studies from around the world have also shown that universal masking policy results in a significant decrease in nosocomial transmission of Covid-19 [18]. Apart from this, there should be an arrangement of a dedicated, well-ventilated area where HCWs can take a break from daily work activities and can have their meals [18]. This restructuring should be extended to reorganization in the ward structure to help in the implementation of physical distancing [21]. Early identification of potential patients using diversified testing criteria and having a low threshold for testing to avoid missing less suspicious cases may also avoid invariable exposures to HCWs [1] While studies have shown that serial testing of patients and HCWs every 7-10 days may identify outbreaks early [23], this may be difficult and costly in a resource-constrained setting.
Once the outbreak investigation concluded, a set of sweeping reforms were introduced to minimize the occurrences of such outbreaks in the future: (i) PPE protocols were revised in low-risk medicine wards and it was made mandatory to wear gown and face shield/goggles in addition to gloves and face mask in all interactions with patients, while face mask and face shield/goggles were made mandatory to be worn all over the hospital; (ii) Use of an N95 mask was made mandatory whenever an HCW went into a high-dependency unit; (iii) Number of HCWs in the unit at a certain time was reduced by restructuring the roster and keeping the minimum number on duty as needed to maintain quality care. This was also done to minimize the number of exposures in case any HCW became symptomatic and tested positive for Covid-19; (iv) HCWs were advised to strategically plan their rounds and reduce unnecessary physical examinations. Computers were placed six feet apart and HCWs were discouraged from taking long breaks together. In addition, taking meals within the vicinity of the ward or in larger groups anywhere in hospital was disallowed to maximize the compliance to physical distancing; (v) Universal testing for SARS Covid antigen was done on all patients being admitted form ER and better screening mechanisms for symptoms at entry points of all hospital wards was mandated; (vi) Educational and awareness sessions were conducted for HCWs for correct practice of PPE and on importance of physical distancing.
Our study is one of the first to address a nosocomial Covid-19 outbreak from Asia / developing countries. The study also helped in initiating specific reforms and policies for the safety of the HCWs working in a developing country in a resource-constrained setting. It reports both physical and behavioral risk factors for contracting infections. However, despite these strengths, the study does have some limitations. Firstly, data is lacking on the number of patients who were Covid-19 infected during this period from the two wards and were discharged prior to testing. Secondly, the data regarding the symptoms of the HCWs and their activities is limited by recall bias and the fear of being caught out due to not following the hospital infection control policies in place. Finally, there may be a few HCWs and administrative staff from other wards who may have had close contacts with HCWs of our ward leading to missed exposures.
Conclusion
This Covid-19 outbreak investigation reports an attack rate of 12.05 % from a low-risk medical unit. The likely origin of the outbreak was from a patient who was admitted with other medical or surgical conditions. The outbreak was further triggered by suboptimal PPE practice and lack of physical distancing in HCWs. It also allowed to evaluate the current surveillance system of infection control and modify it to improve PPE awareness and implementation and to introduce protocols to maintain physical distancing and mass screening using antigen testing for Covid-19 in ER.
Declarations
Ethical approval and consent to participate: The study was conducted after approval from the institutional ethical review committee (ERC # 2020-5078-11372). All data collection was in line with the policies of the employee health department of the hospital, so no separate informed consent was required. Those health care workers who were found positive during this outbreak investigation were notified, properly isolated, monitored for any worsening of symptoms, and advised to get their families tested.
Consent for publication: Not applicable
Availability of data and material: All data generated or analyzed during this study are included in this published article.
Competing interests: The authors declare that they have no competing interests.
Funding: None reported
Author’s contribution: SBZM – Conceptualization, Methodology, Data analysis, Manuscript Writing; AA – Conceptualization, Methodology, Manuscript editing, Supervision; ZN – Methodology, Data collection; AJ – Manuscript writing and formatting; SH – Methodology and Data collection; SFM – Manuscript editing, Supervision.
Acknowledgements: None
References
- Abbas M, Robalo Nunes T, Martischang R, Zingg W, Iten A, Pittet D, et al. Nosocomial transmission and outbreaks of coronavirus disease 2019: the need to protect both patients and healthcare workers. Antimicrob Resist Infect Control, 2021; 10(1): 7.
- Danzmann L, Gastmeier P, Schwab F, Vonberg RP. Health care workers causing large nosocomial outbreaks: a systematic review. BMC Infect Dis, 2013; 13: 98.
- Reingold AL. Outbreak investigations--a perspective. Emerg Infect Dis, 1998; 4(1): 21-27.
- Cespedes MDS, Souza J. Coronavirus: a clinical update of Covid-19. Rev Assoc Med Bras (1992), 2020; 66(2): 116-123.
- Abid K, Bari YA, Younas M, Tahir Javaid S, Imran A. Progress of COVID-19 Epidemic in Pakistan. Asia Pac J Public Health, 2020; 32(4): 154-156.
- CDC. Lesson 6: Investigating an Outbreak - Section 2: Steps of an Outbreak Investigation: CDC Web Archive, 2016.
- Harada S, Uno S, Ando T, Iida M, Takano Y, Ishibashi Y, et al. Control of a Nosocomial Outbreak of COVID-19 in a University Hospital. Open Forum Infect Dis, 2020; 7(12): ofaa512.
- Heinzerling A, Stuckey MJ, Scheuer T, Xu K, Perkins KM, Resseger H, et al. Transmission of COVID-19 to Health Care Personnel During Exposures to a Hospitalized Patient - Solano County, California, February 2020. MMWR Morb Mortal Wkly Rep, 2020; 69(15): 472-476.
- Kabesch M, Roth S, Brandstetter S, Häusler S, Juraschko E, Weigl M, et al. Successful containment of Covid-19 outbreak in a large maternity and perinatal center while continuing clinical service. Pediatr Allergy Immunol, 2020; 31(5): 560-564.
- Schwierzeck V, König JC, Kühn J, Mellmann A, Correa-Martínez CL, Omran H, et al. First Reported Nosocomial Outbreak of Severe Acute Respiratory Syndrome Coronavirus 2 in a Pediatric Dialysis Unit. Clin Infect Dis, 2021; 72(2): 265-270.
- Vimercati L, De Maria L, Quarato M, Caputi A, Stefanizzi P, Gesualdo L, et al. COVID-19 hospital outbreaks: Protecting healthcare workers to protect frail patients. An Italian observational cohort study. Int J Infect Dis, 2021; 102: 532-537.
- Jung J, Hong MJ, Kim EO, Lee J, Kim MN, Kim SH. Investigation of a nosocomial outbreak of coronavirus disease 2019 in a paediatric ward in South Korea: successful control by early detection and extensive contact tracing with testing. Clin Microbiol Infect, 2020; 26(11): 1574-1575.
- Schneider S, Piening B, Nouri-Pasovsky PA, Krüger AC, Gastmeier P, Aghdassi SJS. SARS-Coronavirus-2 cases in healthcare workers may not regularly originate from patient care: lessons from a university hospital on the underestimated risk of healthcare worker to healthcare worker transmission. Antimicrobial Resistance & Infection Control, 2020; 9(1): 192.
- Wang X, Zhou Q, He Y, Liu L, Ma X, Wei X, et al. Nosocomial outbreak of COVID-19 pneumonia in Wuhan, China. Eur Respir J, 2020; 55(6).
- Gao S, Yuan Y, Xiong Y, Zhang Y, Deng L, Chen T, et al. Two outbreaks of SARS-CoV-2 in department of surgery in a Wuhan hospital. Infect Prev Pract, 2020; 2(3): 100065.
- Archibald LK, Jarvis WR. Health care-associated infection outbreak investigations by the Centers for Disease Control and Prevention, 1946-2005. Am J Epidemiol, 2011; 174(11 Suppl): S47-64.
- Oliver D. David Oliver: Could we do better on hospital acquired covid-19 in a future wave? Bmj, 2021; 372: n70.
- Richterman A, Meyerowitz EA, Cevik M. Hospital-Acquired SARS-CoV-2 Infection: Lessons for Public Health. Jama, 2020; 324(21): 2155-2156.
- Advani SD, Yarrington ME, Smith BA, Anderson DJ, Sexton DJ. Are we forgetting the "universal" in universal masking? Current challenges and future solutions. Infect Control Hosp Epidemiol, 2021; 42(6): 784-785.
- Yan Y, Pang Y, Lyu Z, Wang R, Wu X, You C, et al. The COVID-19 Vaccines: Recent Development, Challenges and Prospects. Vaccines (Basel), 2021; 9(4).
- Arora VM, Chivu M, Schram A, Meltzer D. Implementing Physical Distancing in the Hospital: A Key Strategy to Prevent Nosocomial Transmission of COVID-19. J Hosp Med, 2020; 15(5): 290-291.
- Fisher KA, Tenforde MW, Feldstein LR, Lindsell CJ, Shapiro NI, Files DC, et al. Community and Close Contact Exposures Associated with COVID-19 Among Symptomatic Adults ≥18 Years in 11 Outpatient Health Care Facilities - United States, July 2020. MMWR Morb Mortal Wkly Rep, 2020; 69(36): 1258-1264.
- Sastry SR, Pryor R, Raybould JE, Reznicek J, Cooper K, Patrick A, et al. Universal screening for the SARS-CoV-2 virus on hospital admission in an area with low COVID-19 prevalence. Infect Control Hosp Epidemiol, 2020; 41(10): 1231-1233.

