Infra-Renal Endovascular Abdominal Aortic Aneurysm Repair Outcomes in Octogenarians - A Systematic Review and Meta-Analysis
Yousef Yousef1,#, Charles Hallett2,#, Kunal Namjoshi3, Albagir Altahir3, Vaux Robertson3, Nina Al-Saadi4, Isabel O'Shea5, Tamer El-Sayed1,* and David Sidloff6
1The Northern Vascular Centre, Freeman Hospital, Newcastle Upon Tyne, United Kingdom
2Lancashire Teaching Hospitals NHS Trust, UK
3University Hospitals of Leicester, UK
4Russell’s Hall Hospital, Black Country Vascular Network, West Midlands, UK
5East Lancashire Hospitals NHS Trust, UK
6Vascular Surgery Department, Nottingham University Hospitals, UK
#Both Yousef Yousef and Charles Hallett are joint 1st authors and have contributed equally to this manuscript.
Received Date: 02/07/2024; Published Date: 10/10/2024
*Corresponding author: Tamer El-Sayed, MD, FRCS, NIHR Clinical Lecturer in Vascular Surgery, The Northern Vascular Centre, Fourth Floor, Freeman Hospital, Freeman Road, High Heaton, Newcastle upon Tyne NE7 7DN
Abstract
Background: The safety and durability of endovascular aortic aneurysm repair (EVAR) in Octogenarians is a topic of debate. The purpose of this review is to assess the post-operative 30-day outcomes as well as mid -term mortality in octogenarians undergoing EVAR.
Methods: We followed the standard PRISMA guidelines and qualitatively evaluated relevant studies. Meta-analysis was conducted using Mantel – Haenszel and weighted summary proportions, and meta-regression was utilised. The primary outcome was identified as 30-day mortality after EVAR, while secondary outcomes included early post-EVAR endoleaks, cardiac, pulmonary, stroke, renal, and access complications as well as mid mortality.
Results: A total of 25 observational studies, comprising 40,641 octogenarians with an average age of 83.5 years, were included in the meta-analysis. Females were more frequent among octogenarians (19.5% vs 11.8%, p<0.0001). Octogenarians suffered from more comorbidities as coronary artery disease (CAD) (50.1% versus 47.5%, OR 1.2, 95% CI 1.04-1.39, p=0.01), renal disease (47.9% versus 25.87%, OR 1.69, 95% CI 1.30-2.21, p<0.0001), and an ASA score ≥3 (85.6% versus 78.3%, OR 1.49, 95% CI 1.35-1.64, p<0.0001).
30-day pooled complication included cardiac complications 5.2%, pulmonary 2.9, renal 3.5%, stroke 1.3%, access complications 8.5%, any complications 27.5%. 19.8% had evidence of endoleak at 30 days, only 3.1% of octogenarians required re-intervention at 30 days. Octogenarians had similar rates of post-operative re-intervention, sac diameter increase and rupture as non-octogenarians.
The pooled perioperative 30-day mortality for octogenarians was 2.5%, increasing to 9.1% and 52.9% at 1 and 5 years, respectively. Meta-regression analysis suggests an all-cause mortality rate of approximately 10.6% per year (10.58, R 0.86).
Conclusions: EVAR in octogenarians carries a 30-day perioperative mortality of 2.5% with annual all-cause mortality of 10.6% With appropriate patient selection and shared decision-making, EVAR provides a safe and effective option for AAA repair in this age group.
Keywords: Infra-renal Aortic Aneurysm; EVAR; Octogenarians
Introduction
Abdominal Aortic Aneurysm (AAA) is diagnosed when the aortic diameter is more 50.0% of its normal diameter [1] AAA Repair is considered when the risk of rupture outweighs the mortality risk associated with the repair for which the current diameter threshold for elective AAA repair is >5.5cm [2] following randomised evidence provided by the UK Small Aneurysm Trial (UKSAT) [3] and the American Aneurysm Detection and Management study (ADAM) [4]. Beyond this, the rupture risk increases and although there is some recent debate regarding precisely how much, the 30-day mortality of ruptured AAA repair remains high, with a rate of 34.5% in 2021 [5,6]. Therefore, it is crucial to identify and repair AAA in a timely and appropriate manner [8].
Since 1990, Endovascular aneurysm repair (EVAR) has provided an additional surgical option for patients undergoing AAA repair with over half of all elective AAA repairs in the UK now being done through an endovascular approach rising to over 80.0% of AAA repair in Octogenarians [6,7]. The number of individuals aged over 80 years and over is expected to triple between 2020 and 2050 globally from 142 million to 426 million [8]. Potentially leading to an increase in the number of elderly patients reaching the treatment threshold for abdominal aortic aneurysms (AAA) [9].
Whilst previous studies have shown that both open surgical repair (OSR) and EVAR in octogenarians are associated with increased mortality, and postoperative complications compared to non-octogenarians, EVAR offers a potential treatment option in those who are either unsuitable or unfit to undergo major OSR for which octogenarians as a more co-morbid subgroup are more likely to fall within [10-13].
In 2017, Han et al systematic review compared EVAR in octogenarians vs non-octogenarians [14], however, there have since been additional studies published in the literature. Therefore, offering an up-to-date assessment of infra-renal EVAR outcomes in octogenarians is essential. This can provide a comprehensive analysis of mid-term EVAR outcomes among octogenarians.
Methods
Protocol and registration: This review followed standard reporting guidelines and was registered with the International Prospective Register of Systematic Reviews (PROSPERO) [15] and adhered to the Preferred Reporting Items for Systematic Review and Meta-Analyses (PRISMA) [16] guidelines.
The eligibility criteria for the studies included in the systematic review were as follows:
- The studies must report on elective non-ruptured infra-renal EVAR
- The studies must compare the outcomes of octogenarians to non-octogenarians.
- The study size must be 30 or greater.
- The studies must report post-procedural outcomes and mortality at any specified point.
The exclusion criteria for the studies were:
- Studies that reported complex EVAR procedures such as branched, fenestrated, or thoracic or did not differentiate between the types of AAA.
- Studies that reported solely on ruptured AAA.
- Studies that did not differentiate between OSR and EVAR.
- Studies that contained unpublished, non-peer-reviewed data, such as abstracts, small case series, reviews, or expert opinions.
- Studies that reported data in a non-comparable fashion, such as single-arm studies.
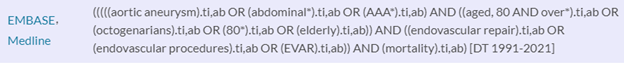
Literature review and search: A comprehensive and systematic literature search was conducted by two independent reviewers, CDH and KN. The search was performed using the Medline and Embase databases, which were accessed through the Healthcare Databases Advanced Search (HDAS) interface. A comprehensive list of keywords and Medical Subject Heading (MeSH) terms were used to retrieve relevant articles from the literature. The search criteria were not limited by language and covered articles published from January 1991 (when the results of the first use of Elective Infra-renal EVAR were reported by Parodi et al [7] to February 2021. In addition, the reference lists of selected articles were screened for any additional studies. The search was initially run over a period of two weeks from 8/02/2021 – 21/02/2021 and updated over a period of one week from 20/02/2023-26/02/2023. The 2023 update used OVID Technologies Inc. due to the closure of the HDAS interface [12]. Details of the search strategy are provided in Appendix 1.
Study selection: Pre-defined eligibility criteria were set as described Titles and abstracts of articles were screened and the full text reviewed of studies that appeared to meet the inclusion criteria. Any discrepancies were resolved by a third review author (YY).
Data Collection: Data collection was carried out by two authors (IMO and KN) and was cross-checked by a third author (CDH). Data collection included details of study design, patient demographics, aneurysm anatomy, procedural details, postoperative outcomes, and follow-up. Data was collected for both octogenarian and non-octogenarian populations to facilitate comparison where required.
Study outcomes: Primary outcome: 30-day mortality after EVAR.
Secondary outcomes: early post-EVAR complications including endoleaks, cardiac, pulmonary, stroke, renal, and endovascular access complications as well as midterm mortality.
Risk of Bias in individual studies and across studies: The quality of the selected studies was evaluated by two authors (KN and IMO) using the Newcastle-Ottawa Scale (NOS) [17]. A score of seven or above out of a maximum of nine was considered to be indicative of a high-quality study. To assess the risk of publication bias, funnel plots were utilised as a visual representation of the distribution of effect sizes in the studies. The asymmetrical inverted V shape in the data points on the funnel plot indicates the absence of publication bias.
Statistical analyses: The primary outcomes were analysed using either Odds Ratio (OR) for dichotomous data or Weighted Mean Difference (WMD) for continuous data, both with a 95% Confidence Interval (CI). Statistical significance was established with a p-value less than 0.05. The Mantel-Haenszel method was employed to compare the odds of outcomes between octogenarians and non-octogenarians, with an OR greater than 1 indicating that the event was more frequent among the octogenarians group. Weighted summary proportions were utilised to assess events within individual study populations. The degree of heterogeneity among studies was calculated using the I-squared (i²) test. In cases where significant heterogeneity was identified, a random-effects model was used. Conversely, a fixed-effects model was applied in the absence of significant heterogeneity.
To assess publication bias, 30-day mortality was selected as this was the most consistently reported outcome across the studies included.
All statistical analysis was conducted using Review Manager (RevMan), Windows 10 Version 5.4, The Cochrane Collaboration 2020, and MedCalc Statistical Software version 19.2.6 (MedCalc Software bv, Ostend, Belgium; https://www.medcalc.org; 2020).
- Literature Search terms for HDAS database and update search through OVID platform.
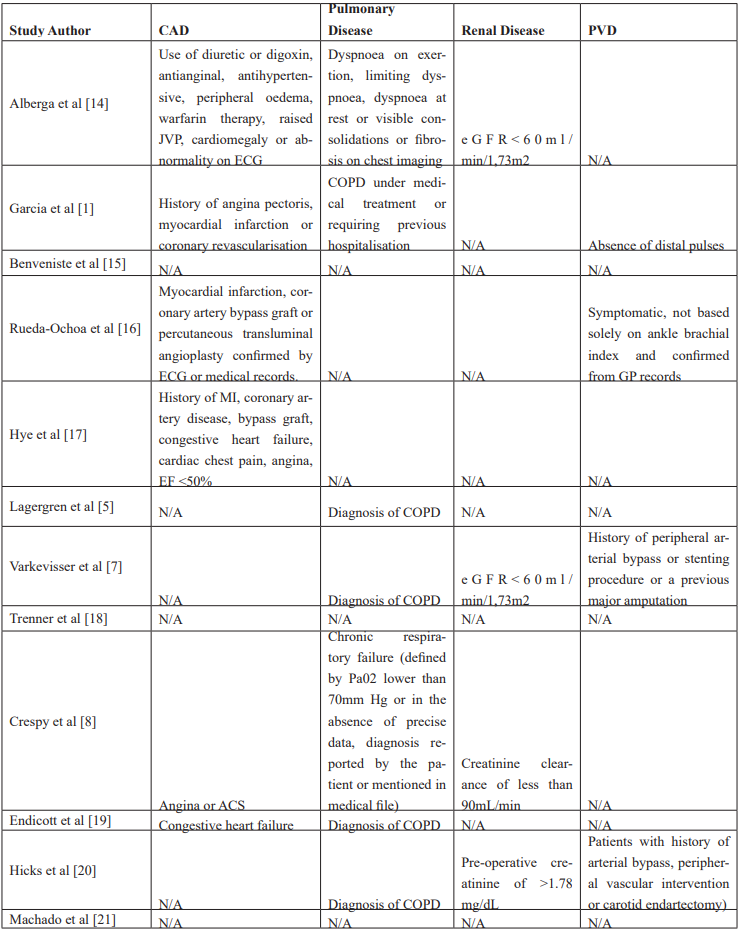
- Supplementary table showing Study definitions were defined for pre-operative characteristics.

Results
Study Selection and Characteristics: After conducting an initial screening to exclude duplicates, 914 articles were initially assessed. Of these, 130 articles were considered for potential inclusion in the review. Of these, 42 were abstracts only, 33 were missing post-procedural outcomes data or had incorrect age comparisons, 13 had no comparison by age, 8 were non-original data (such as review articles or meta-analyses), 5 could not be retrieved, 3 included complex or ruptured AAA repair, 2 had fewer than 30 patients and 2 had duplicate data with no additional parameters reported.
As a result, 21 studies met the pre-defined inclusion criteria, and four further studies were identified from reviewing the references of the included studies. The updated 2023 search identified a further 145 articles of which 15 were considered for potential conclusion but all were eventually excluded. Figure 1 provides a detailed illustration of the study selection, inclusion, and exclusion process is presented in the PRISMA diagram.
The studies included in this review were conducted from 1994 to 2019 and published between 2005 and 2021. The studies originated from the USA (8 studies), Europe (9 studies), 4 international studies (data collected from 2 or more countries) and Australia (1 study). Although there was some overlap in the data sources used between studies, only unique data was extracted for this review. The total number of patients undergoing infra-renal AAA repair was 40,641 octogenarians and 119,858 non-octogenarians. Table 1 provides individual study characteristics. The quality of the studies was evaluated using the NOS, with scores ranging from 5 to 8. Most studies were rated as medium or high quality, as shown in Table 2. All studies were observational and there were no randomised controlled trials.
Bias and quality within studies: Funnel plots for 30-day mortality in Figure 2 showed an even distribution within the accepted limits, indicating a low likelihood of publication bias.
Patient demographics: The total number of patients undergoing infra-renal AAA repair was 40,641 octogenarians and 119,858 non-octogenarians. Patient demographics and comorbidities are summarised in Table 3. Significantly more non-octogenarians were male (88.2%) compared to the octogenarians (80.5%) (OR 0.53, 95% CI 0.56-0.61, p <0.0001).
Octogenarians had more co-morbidities compared to non-octogenarians as coronary artery disease (CAD) (50.1% versus 47.5%, OR 1.2, 95% CI 1.04-1.39, p=0.01), renal disease (47.9% versus 25.9%, OR 1.69, 95% CI 1.30-2.21, p<0.0001), and an ASA score ≥3 (85.6% versus 78.3%, OR 1.49, 95% CI 1.35-1.64, p<0.0001).
Procedural data: The patients’ aneurysm morphology and perioperative data are reported in Table 4. The mean diameter of AAA was significantly larger among octogenarians (58.9mm) compared to non-octogenarians (56.7mm) (mean difference 2.99mm, 95% CI 2.01-3.93mm, p<0.0001). There was no difference in aneurysm neck length (mean difference 1.77mm, 95% CI -1.81-5.35, p 0.33) or neck diameter (mean difference 0.21mm, 95% CI -0.01-0.43, p 0.06) between the two groups.
Operation time (146.2 minutes versus 137.6 minutes, mean difference 3.25 minutes, 95% CI -8.8-15.9, p 0.6) and length of ICU stay (1.03 days versus 1.14 days, mean difference -0.27 days, 95% CI -0.93—0.39, p 0.42) and overall hospital length of stay (mean 7.72 days versus 5.85 days, p 0.12) were comparable between the two groups. Octogenarians had a higher mean blood loss (278.9mL versus 255mL, mean difference 24.64mL, 95% CI 7.26-42.02, p 0.005).
30-Day Outcomes: The thirty-day mortality, endoleak and post-operative complications are summarised in Table 5. Thirty-day mortality was 2.5% among octogenarians with the weighted summary proportion of endoleak 19.8%. Cardiac complications were recorded as 5.2%, pulmonary complications in 2.9 %, renal complications in 3.6%, stroke in 1.3%, endovascular access complications in 8.5% and any complications of 27.5%. Technical success was 96.0% whilst conversion to open was 0.7% and the 30-day reintervention rate was 3.1%.
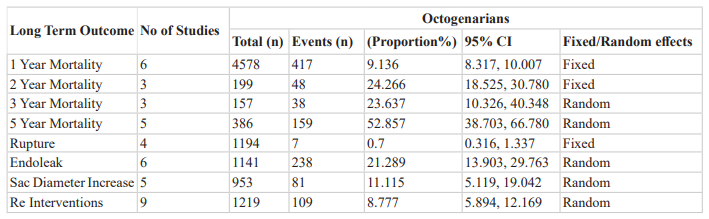
Midterm outcomes: The midterm outcomes are summarised in Table 6, Six studies reported 1-year mortality with a weighted summary proportion of 9.1%. Three studies reported on 2-year and 3-year mortality rates with 24.3% and 23.6% respectively. At 5-years a weighted summary proportion the mortality was 52.9%.
Four studies reported on the incidence of late rupture of 0.7%, six studies on endoleak 21.3%, five studies reported the incidence of sac diameter increase which was 11.1% and nine studies reported on incidence of re-intervention which was 8.8%.
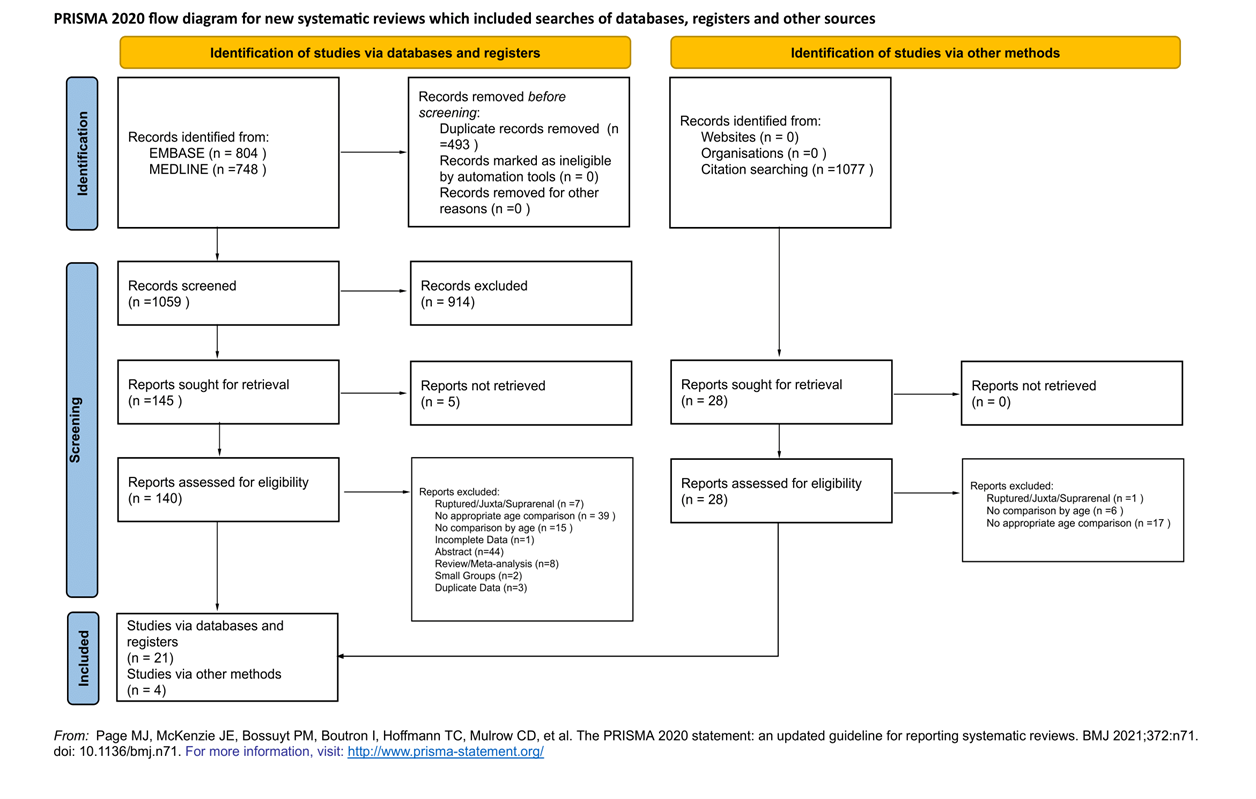
Figure 1: PRISMA flow diagram of study selection process.
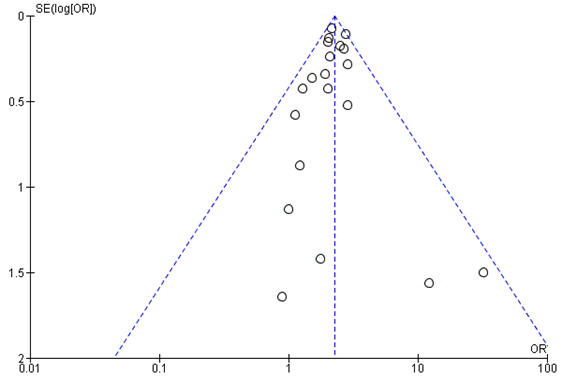
Figure 2: Funnel Plot for 30 Day mortality of Octogenarians compared to non-Octogenarians.
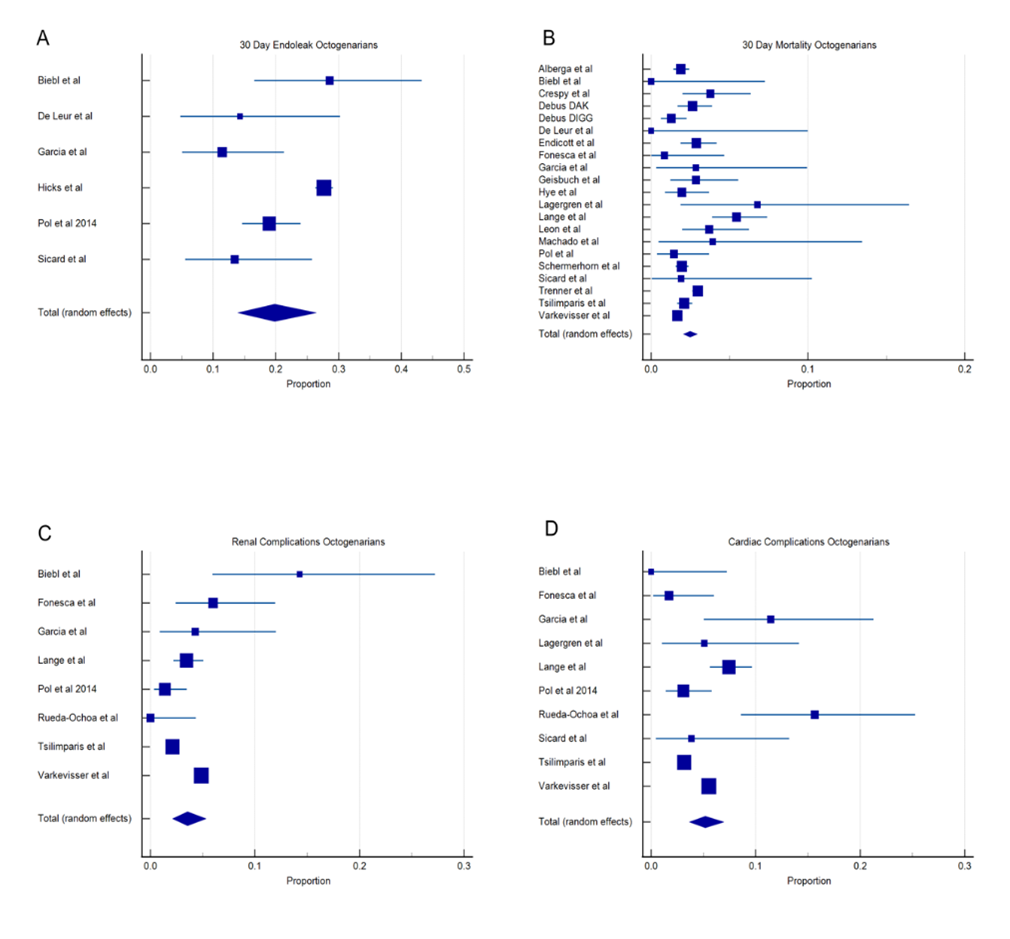
Figure 3: Single arm forest plots to represent the Octogenarian cohort (Single arm forest plots within the Octogenarian cohort showing individual studies proportion and overall total effect. A = 30-day endoleak, B = 30-day mortality, C = cardiac complications and D = renal complications.)
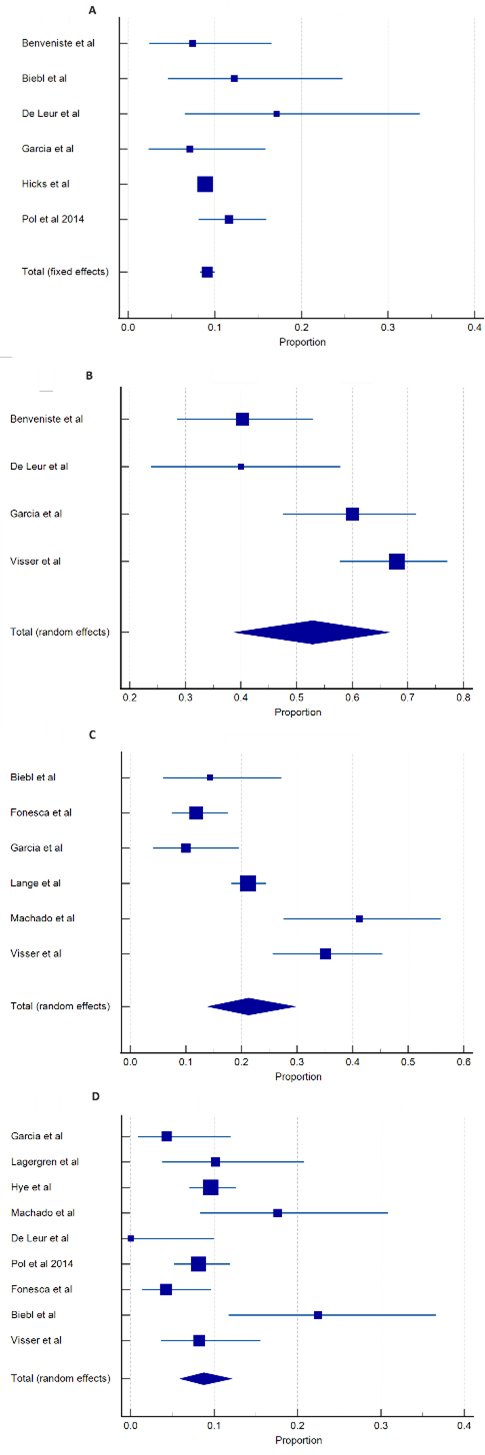
Figure 4: Mid to long-term outcomes (weighted summary proportions) for; A = 1 Year Mortality, B = 5 Year Mortality, C = Endoleak, D = Re-intervention (R3 Minor C3 - Please mention the time for the C & D estimates).
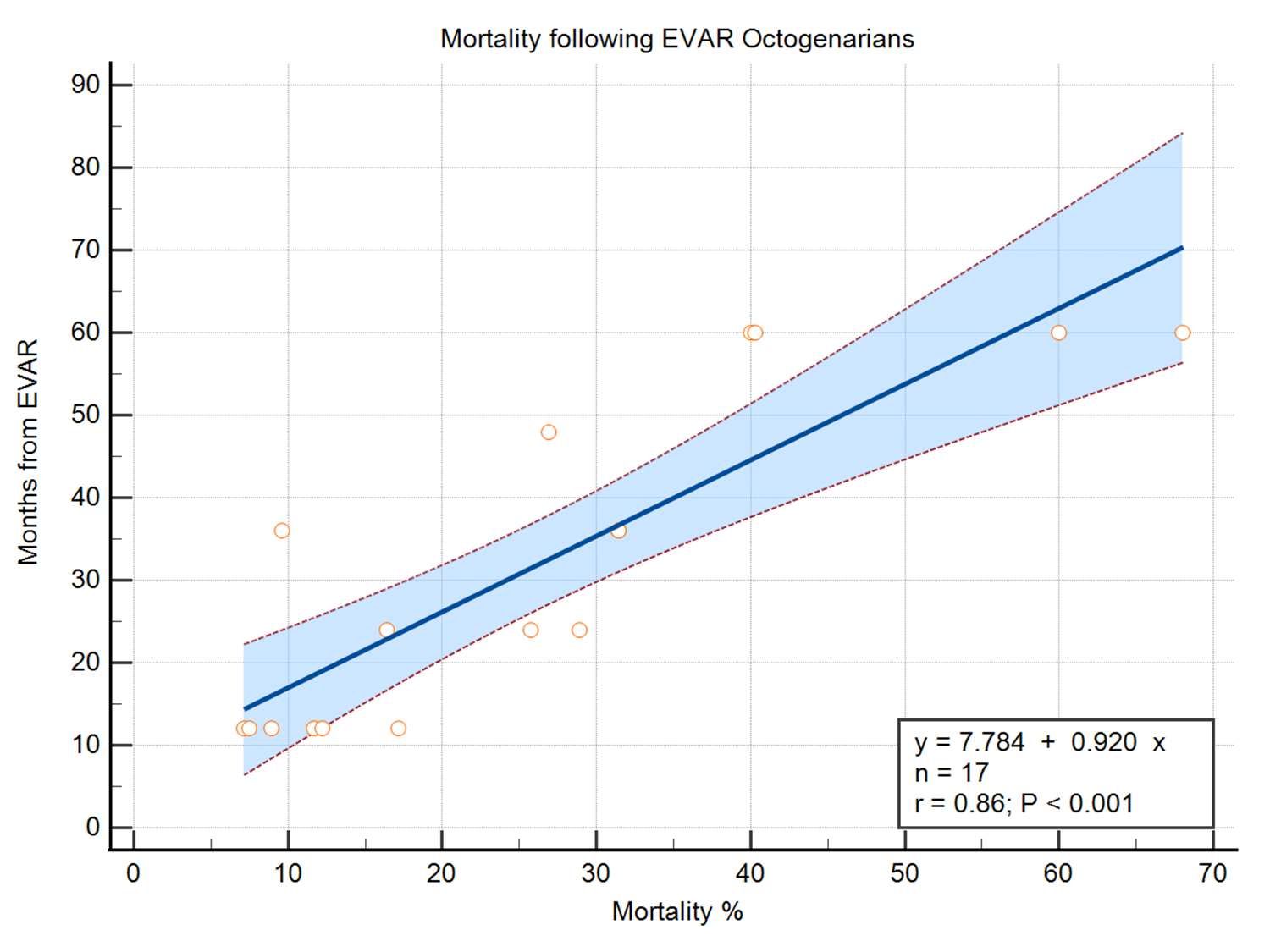
Figure 5: A = Linear meta-regression of mortality for octogenarians following EVAR.
Table 1: Summary of Included Studies.
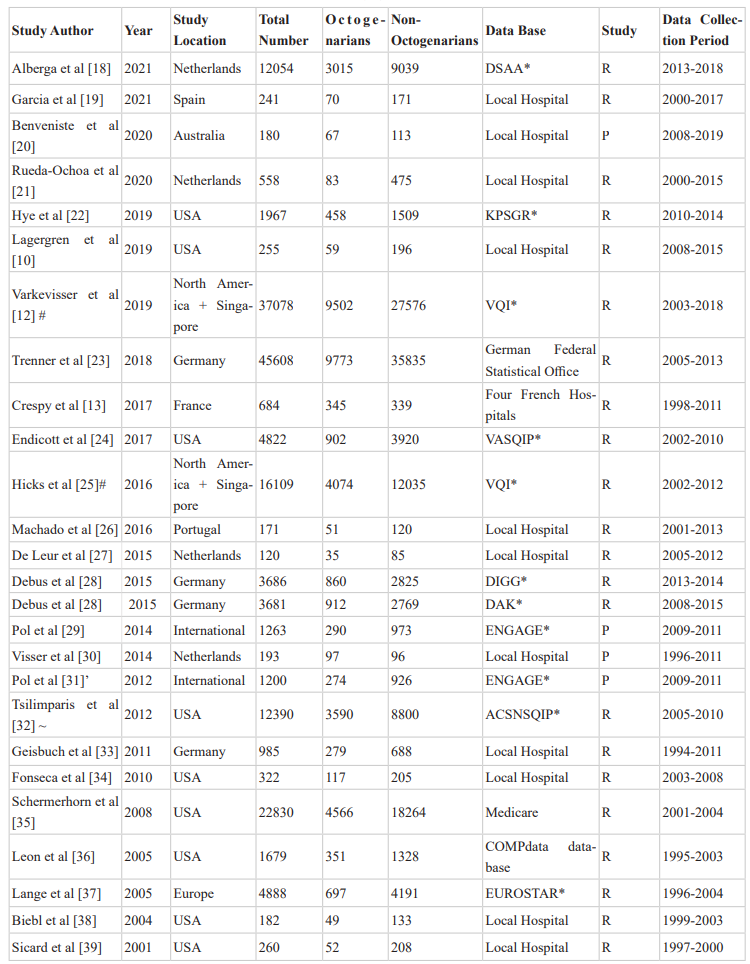
R - Retrospective study, P - Prospective Study, *VQI - Vascular Quality Initiative, ENGAGE - Endurant Stent Graft Natural Selection Global Post-market Registry, KPSGR - Kaiser Permanente Endovascular Stent Graft Registry, DSAA - Dutch Surgical Aneurysm Audit, DAK - German Employees' Health Insurance Fund, DIGG - German Institute for Vascular Health Care Research, EUROSTAR - The EUROpean collaborators on Stent–graft Techniques for abdominal aortic Aneurysm Repair, ACSNSQIP - American College of Surgeons National Surgical Quality Improvement Programme, # Both Studies use the VQI database, ̾ Both studies use ENGAGE registry, ~ Figures for total number, number of octogenarians and non-octogenarians not given and back calculated from mortality percentages, ^ Study includes two different databases DIGG and DAK.
Table 2: Quality of Study Assessment using Newcastle Ottawa Scale.
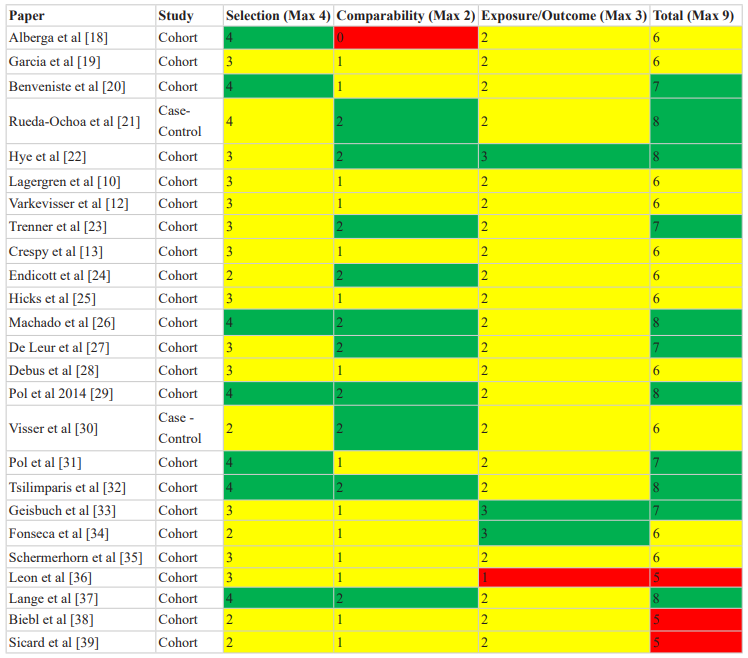
Colour coded by Green/Yellow/Red. Green for high scoring papers and Red for low scoring papers and Yellow for intermediate.
Table 3: Patient characteristics and comorbidities.
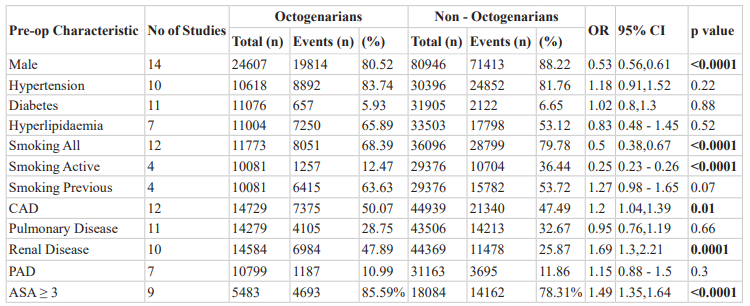
CAD = Coronary artery disease, PAD = Peripheral arterial disease, ASA = American Society of Anaesthesiology. (For further definitions of CAD, Pulmonary disease, renal disease and PVD please see supplementary table 1).
Table 4: Perioperative and Aneurysmal Data.
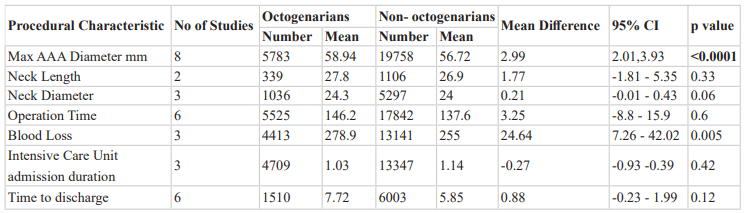
Table 5: 30-day outcomes.
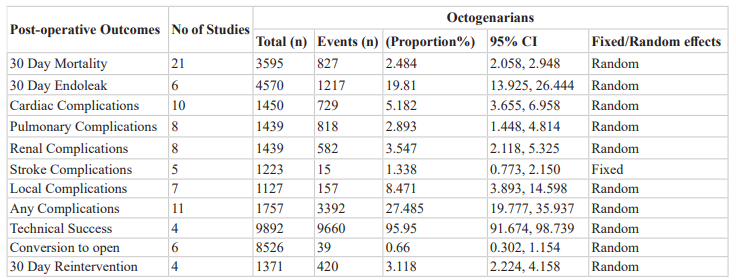
Results from DIGG and DAK registries/databases have been counted as separate for 30 day mortality.
Table 6: Mid to Long-term mortality and outcomes.
Additional Analyses
Sensitivity Analysis: After conducting the initial meta-analysis, we noticed that one of the studies, Fonesca et al, had a substantially lower mortality at 5 years compared to the other studies. We therefore performed a sensitivity analysis on this to determine its impact on the results. The sensitivity analysis included data from five studies with a total 386 octogenarians. We systematically excluded each study in turn examining the resultant weighted mean proportion, and standard deviations. For this outcome Fonesca et al was found to lie more than 2 standard deviations away and as such the removal of this study offers a more representative outcome of the octogenarian population for 5-year mortality.
Meta-Regression: A meta-regression analysis was conducted to examine the all-cause mortality rates between 1- and 5 years post-EVAR.
The results of the analysis revealed that octogenarians had a yearly all-cause mortality rate of 10.6% with an R2 of 0.74. This indicates that the model as seen in Figure 5 explains 74.0% of the variability in the mortality data.
Discussion
Octogenarians who require infra-renal AAA repair, pose a clinically challenging cohort considering their multiple co-morbidities and the yearly risk of rupture and the associated high mortality. With the expected increase in the octogenarian population over the coming years, EVAR is likely to be frequently used particularly within the octogenarian cohort.
Our meta-analysis and systematic review provide a thorough review of the differences in early postoperative outcomes observed in octogenarians undergoing infra-renal AAA repair as well as mid -term mortality. This complements a previous meta-analysis performed by Han et al in 2017 [2] where, following a rigours literature search and strict inclusion/ exclusion criteria 10 studies have been included which have been published since this data and an additional 5 studies identified for inclusion.
Our study primary outcome of 30-day mortality was noted to be 2.5% among octogenarians which appears acceptable when viewed in the context of the annual rupture risk of a AAA >5.5cm.
The increased 30-day mortality is consistent with the findings of increased rates of cardiac, renal, pulmonary, and endovascular access complications within the octogenarian population. Whilst the technical success was significantly higher in non-octogenarians this did not translate into a significant difference in re-intervention rate with Benveniste et al suggesting that re-intervention rates were higher in those with unfavourable anatomy and usage outside of instructions for use. Nor did the higher incidence of endoleak seen in octogenarians both in the early or late follow-up result in a significant difference in re-intervention rate between the age groups.
Biebl et al [38] found that the most common systemic complication in patients over 80 years old was renal dysfunction, whilst Saratzis et al [40] found that the incidence of Acute Kidney Injury (AKI) after EVAR is significant and is independently associated with medium-term mortality and morbidity [41]. Rueda et al [21] suggested that renal dysfunction with preoperative urea levels greater than 50 mg/dl identified a higher likelihood of AKI indicating a need to identify the at-risk population to optimise pre-operative renal functions. Renal dysfunction following EVAR may be caused due to use of contrast and thromboembolism and vigilant monitoring of serum creatinine and urine output is warranted to allow for timely interventions to minimise post-operative complications. Both cardiac and pulmonary complications were observed to be significantly higher in octogenarians post-EVAR in our study. Pre-operatively octogenarians did not have a significantly higher incidence of pulmonary disease within our study population.
Within our study, we noted a lower proportion of males and active smokers in the octogenarian population however a higher proportion of ex-smokers with nicotine and gender well established risk factors for aneurysm formation [38]. The increase in co-morbidity with age was demonstrated with the significantly higher incidence of cardiac, pulmonary, and peripheral vascular disease within the octogenarian population correlating with the higher proportion of octogenarians considered ASA ≥ 3 as evidenced by Pol et al [29]. This increased co-morbidity in the octogenarian population may be one of the factors influencing the higher post-operative mortality and complication rates observed compared to the non-octogenarian population with Garcia et al [19] showing an ASA of 4 being an independent risk factor for lower mid-term survival rates. Lange et al also found an increased risk of systemic complications in octogenarians who underwent EVAR, they proposed that this may be due to octogenarians being more heavily comorbid, which could have led to them being deemed unfit for open repair [37].
Although previous studies suggested a higher likelihood of complex aortic anatomy in octogenarians with increased aneurysm tortuosity and max diameter than in non-octogenarians [29,37]. This study showed no significant difference in neck length or neck diameter. Both groups had comparable EVAR operative time, ICU duration, length of hospital stay, technical success or conversion to open. Whilst blood loss was found to be statistically significant between the two groups the small difference in volume is unlikely to be of clinical significance. This is discussed by Pol et al [29] suggesting the reasons the reason for the increased blood loss in the octogenarian group may be secondary to less favourable aneurysm anatomy although theirs did not reach statistical significance, however, they noted that this remained significantly less that blood loss from open surgical repair. Octogenarians with unrepaired large aortic aneurysms pose an increased risk of rupture as discussed by Lederle et al [41] with a 9.4% rupture risk in 1 year for aneurysms between 5.5-5.9cm. However, Hye et al [22] observed that although age >80 and AAA diameter >5.5cm were independent risk factors for survival post-AAA when combined the risk was not amplified.
Our analysis showed that whilst as expected midterm mortality rates were higher in octogenarians which is congruent with De Leur and Lagergren et al’s findings [10,27]. De Leur's results however suggested this was not the case after open surgical repair and Fonesca et al [34] results showed comparable 5-year mortality between octogenarians and non-octogenarians. One explanation may be selection bias and a higher operative fitness among the octogenarians undergoing OSR as well as those selected for EVAR in the Fonesca study. This highlights the importance of considering patient selection when offering surgical intervention. The all-cause mortality in octogenarians following EVAR of 10.6% is acceptable and worth consideration. De Leur et al reported an even poorer mid-term survival among octogenarians treated conservatively, again perhaps explainable by selection bias. This however contrasts with the findings of the EVAR 2 trial [40] which showed no benefit of EVAR over conservative management in those unsuitable for operative repair, but they reported a 30-day mortality of 7.3% compared to our study's findings of 2.5% at 30 days. Mortality due to rupture was low at 0.7% and is likely to be an underestimation when compared to previous trials such as the EVAR 2 trial.
The above findings support EVAR as a reasonable option for infra-renal aortic aneurysms, particularly in large aneurysms. With an all-cause mortality of 10.6% of which 0.7% was due to rupture this supports the importance of patient selection and the patient-shared decision when considering aneurysm repair.
Limitations
This systematic review has several limitations. Firstly, heterogeneity throughout the studies should be noted including follow-up periods, patient enrolment and patient characteristics, stent graft devices used and post-procedural outcomes. All the studies were observational in nature and only 11 papers considered to be of high quality reducing the quality of evidence available for review and analysis. This systematic review covers a wide period of 1994-2019, as a result the older generation of stent grafts as well as the learning curve previously associated with the delivery of EVAR may have influenced the outcomes of some of the older studies included. Loss to follow-up as well as lack of reporting on cause of death following aneurysm repair impacts the ability to assess the efficacy of EVAR in the octogenarian population as well as introducing potential selection bias.
Conclusion
Our findings support the usage of EVAR as a safe option for AAA repair in the octogenarian population demonstrating acceptable midterm mortality at 5 years as well as mortality within the early peri-operative phase at 30 days. Given the octogenarian's unique risk profile, we emphasize the importance of careful and appropriate patient selection based on a patient-centred multi-disciplinary approach. This must take into consideration the individual co-morbidities, rupture risk and quality of life markers. Careful patient selection may further reduce the peri-operative and mid-term mortality associated with EVAR repair in octogenarians and further studies are required to investigate prognostic indicators pre-EVAR repair.
References
- Johnston KW, Rutherford RB, Tilson MD, Shah DM, Hollier L, Stanley JC. Suggested standards for reporting on arterial aneurysms. J Vasc Surg, 1991; 13(3): 452–458.
- National Institute for Healthcare and Excellence: Abdominal aortic aneurysm: diagnosis and management NICE guideline [NG156], 2020.
- Powell JT. Final 12-year follow-up of Surgery versus Surveillance in the UK Small Aneurysm Trial. British Journal of Surgery, 2007; 94(6): 702–708.
- Lederle FA. The Aneurysm Detection and Management Study Screening Program. Arch Intern Med, 2000; 160(10): 1425.
- Earnshaw JJ. The Indication for Elective Repair of Abdominal Aortic Aneurysm Should Be Reviewed. European Journal of Vascular and Endovascular Surgery, 2021; 61(1): 7–8.
- National Vascular Registry, 2021.
- Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg, 1991; 5(6): 491–499.
- https://www.who.int/news-room/fact-sheets/detail/ageing-and-health.
- Living longer; how our population is changing and why it matters, 2018.
- Lagergren E, Chihade D, Zhan H, Perez S, Brewster L, Arya S, et al. Outcomes and Durability of Endovascular Aneurysm Repair in Octogenarians. Ann Vasc Surg, 2019; 54: 33–39.
- Dang T, Dakour-Aridi H, Rizwan M, Nejim B, Malas MB. Predictors of acute kidney injury after infrarenal abdominal aortic aneurysm repair in octogenarians. J Vasc Surg, 2019; 69(3): 752-762.e1.
- Varkevisser RRB, O’Donnell TFX, Swerdlow NJ, Liang P, Li C, Ultee KHJ, et al. Factors associated with in-hospital complications and long-term implications of these complications in elderly patients undergoing endovascular aneurysm repair. J Vasc Surg, 2020; 71(2): 470-480.e1.
- Crespy V, Salomon du Mont L, Kaladji A, Bartoli M, Gouëffic Y, Abello N, et al. Endovascular Treatment of Asymptomatic Abdominal Aortic Aneurysms in Octogenarians: Factors Influencing Long-term Survival. Ann Vasc Surg, 2017; 45: 199–205.
- Han Y, Zhang S, Zhang J, Ji C, Eckstein HH. Outcomes of Endovascular Abdominal Aortic Aneurysm Repair in Octogenarians: Meta-analysis and Systematic Review. Eur J Vasc Endovasc Surg, 2017; 54(4): 454–463.
- National Institute for Health Research International Prospective Registry of Systematic Reviews (PROSPERO).
- Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol, 2010; 25(9): 603–605.
- Alberga AJ, Karthaus EG, van Zwet EW, de Bruin JL, van Herwaarden JA, Wever JJ, et al. Outcomes in Octogenarians and the Effect of Comorbidities After Intact Abdominal Aortic Aneurysm Repair in the Netherlands: A Nationwide Cohort Study. European Journal of Vascular and Endovascular Surgery, 2021; 61(6): 920–928.
- Marcos Garcia L, Calsina Juscafresa L, Velescu A, Casajuana Urgell E, Galarza Tapia A, Llort Pont C, et al. Outcome of elective endovascular repair of abdominal aortic aneurysms in octogenarians. Geriatr Gerontol Int, 2021; 21(5): 392–397.
- Benveniste GL, Tjahjono R, Chen O, Verhagen HJM, Böckler D, Varcoe RL. Long-term Results of 180 Consecutive Patients with Abdominal Aortic Aneurysm Treated with the Endurant Stent Graft System. Ann Vasc Surg, 2020; 67: 265–273.
- Rueda-Ochoa OL, van Bakel P, Hoeks SE, Verhagen H, Deckers J, Rizopoulos D, et al. Survival After Uncomplicated EVAR in Octogenarians is Similar to the General Population of Octogenarians Without an Abdominal Aortic Aneurysm. European Journal of Vascular and Endovascular Surgery, 2020; 59(5): 740–747.
- Hye RJ, Janarious AU, Chan PH, Cafri G, Chang RW, Rehring TF, et al. Survival and Reintervention Risk by Patient Age and Preoperative Abdominal Aortic Aneurysm Diameter after Endovascular Aneurysm Repair. Ann Vasc Surg, 2019; 54: 215–225.
- Trenner M, Kuehnl A, Reutersberg B, Salvermoser M, Eckstein HH. Nationwide analysis of risk factors for in-hospital mortality in patients undergoing abdominal aortic aneurysm repair. British Journal of Surgery, 2018; 105(4): 379–387.
- Endicott KM, Emerson D, Amdur R, Macsata R. Functional status as a predictor of outcomes in open and endovascular abdominal aortic aneurysm repair. J Vasc Surg, 2017; 65(1): 40–45.
- Hicks CW, Obeid T, Arhuidese I, Qazi U, Malas MB. Abdominal aortic aneurysm repair in octogenarians is associated with higher mortality compared with nonoctogenarians. J Vasc Surg, 2016; 64(4): 956-965.e1.
- Machado R, Teixeira G, Oliveira P, Loureiro L, Pereira C, Almeida R. Is age a determinant factor in EVAR as a predictor of outcomes or at procedure selection? Our experience. Braz J Cardiovasc Surg, 2016.
- de Leur K, Flu HC, Ho GH, de Groot HGW, Veen EJ, van der Laan L. Outcome of elective treatment of abdominal aortic aneurysm in elderly patients. International Journal of Surgery, 2015; 15: 117–123.
- Debus ES, Torsello G, Behrendt CA, Petersen J, Grundmann RT. Perioperative mortality following repair for abdominal aortic aneurysm in Germany: Comparison of administrative data of the DAK health insurance and clinical registry data of the German Vascular Society. Chirurg, 2015; 86(11): 1041–1050.
- Pol RA, Zeebregts CJ, van Sterkenburg SMM, Ferreira LM, Goktay Y, Reijnen MMPJ, et al. Outcome and quality of life after endovascular abdominal aortic aneurysm repair in octogenarians. J Vasc Surg, 2014; 60(2): 308–317.
- Visser L, Pol RA, Tielliu IFJ, van den Dungen JJAM, Zeebregts CJ. A limited and customized follow-up seems justified after endovascular abdominal aneurysm repair in octogenarians. J Vasc Surg, 2014; 59(5): 1232–1240.
- Pol RA, Zeebregts CJ, van Sterkenburg SMM, Reijnen MMPJ, ENGAGE Investigators. Thirty-day outcome and quality of life after endovascular abdominal aortic aneurysm repair in octogenarians based on the Endurant Stent Graft Natural Selection Global Postmarket Registry (ENGAGE). J Vasc Surg, 2012; 56(1): 27–35.
- Tsilimparis N, Perez S, Dayama A, Ricotta JJ. Age-stratified results from 20,095 aortoiliac aneurysm repairs: should we approach octogenarians and nonagenarians differently? J Am Coll Surg, 2012; 215(5): 690–701.
- Geisbüsch P, Katzen BT, Tsoukas AI, Arango D, Peña CS, Benenati JF. Endovascular repair of infrarenal aortic aneurysms in octogenarians and nonagenarians. J Vasc Surg, 2011; 54(6): 1605–1613.
- Fonseca R, Rockman C, Pitti A, Cayne N, Maldonado TS, Lamparello PJ, et al. Intermediate-term EVAR outcomes in octogenarians. J Vasc Surg, 2010; 52(3): 556–560; discussion 560-561.
- Schermerhorn ML, O’Malley AJ, Jhaveri A, Cotterill P, Pomposelli F, Landon BE. Endovascular vs. open repair of abdominal aortic aneurysms in the Medicare population. N Engl J Med, 2008; 358(5): 464–474.
- Leon LR, Labropoulos N, Laredo J, Rodríguez HE, Kalman PG. To what extent has endovascular aneurysm repair influenced abdominal aortic aneurysm management in the state of Illinois? J Vasc Surg, 2005; 41(4): 568–574.
- Lange C, Leurs LJ, Buth J, Myhre HO, EUROSTAR collaborators. Endovascular repair of abdominal aortic aneurysm in octogenarians: an analysis based on EUROSTAR data. J Vasc Surg, 2005; 42(4): 624–630; discussion 630.
- Biebl M, Lau LL, Hakaim AG, Oldenburg WA, Klocker J, Neuhauser B, et al. Midterm outcome of endovascular abdominal aortic aneurysm repair in octogenarians: a single institution’s experience. J Vasc Surg, 2004; 40(3): 435–442.
- Sicard GA, Rubin BG, Sanchez LA, Keller CA, Flye MW, Picus D, et al. Endoluminal graft repair for abdominal aortic aneurysms in high-risk patients and octogenarians: is it better than open repair? Ann Surg, 2001; 234(4): 427–435; discussion 435-437.
- Endovascular Repair of Aortic Aneurysm in Patients Physically Ineligible for Open Repair. New England Journal of Medicine, 2010; 362(20): 1872–1880.
- Lederle FA. Rupture Rate of Large Abdominal Aortic Aneurysms in Patients Refusing or Unfit for Elective Repair. JAMA, 2002; 287(22): 2968.

