Coverage of Foot Defect in Pediatric Population
Ismail Benomar1,2,*, Fadoua Boughaleb1,2, Chaimae Ben Driss1,2, Souha Qarouach1,2, Abdarahmane Lemhaba1,2, Ghita El Moulihi1,2, Rachid Belkacem1,2, Mohamed Rami1,2, Mohamed Amine Bouhafs1,2 and Nawfal Fejjal1,2
1Plastic Surgery Unity, Children hospital of Rabat
2Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Received Date: 19/06/2024; Published Date: 07/10/2024
*Corresponding author: Ismail Benomar, Plastic Surgery Unity, Children hospital of Rabat; Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Abstract
Objective: Report the experience of our department concerning the management of foot defect in pediatric population, by analyzing the circumstances of its occurrence and etiologies, the surgical techniques allowing its repair, their indications, result, and complications.
Material and Methods: It is a retrospective study over a period of 11 years from October 2011 to December 2022 at the plastic surgery unity in children’s hospital of Rabat, including 30 patients.
This study includes all patients with foot defect who were surgically treated (initially or secondarily).
For our study, we proceeded to the collection of data from the computerized files based on an exploitation form. We used Excel software for the analytical study.
Results and Discussion: The average age of the children treated was 10.2 years, with a male predominance of (67%). The predominant etiology was public road accidents (60%). 6.6% of these Foot defect was associated with other lesions. The results obtained after surgery were globally good, with 93% of the patients (or their parents for the youngest) declaring that the final appearance after the repair was good or moderately good. Most of the patients with an initially no suturable defect had benefited from a skin graft sometimes associated with flaps (59%). The results obtained were similar to those found in the literature, and confirm the conclusions drawn by other teams, which are that this method is effective in the repair of large defect and their sequels.
Conclusion: The foot defect is a pathological entity frequently found in children and is potentially serious. It requires rapid and appropriate management to avoid serious complications that put at risk vital, functional and aesthetic prognosis of the child.
Keywords: Child; Foot defect; Coverage; Sural flap
Introduction
Skin defects are wounds, which cannot be primarily managed by sutures. Their management is problematic when it involves functional areas such as hand or foot. For this reason, it is performed in two stages. The first stage comes in the context of emergency to close the defect and the second one in a purely aesthetic procedure. The etiologies are various (post traumatic, burns, after carcinologic surgery). There are several techniques for the treatment of the foot defect such as suture, secondary healing, skin graft and flaps.
In this work we report the experience of the plastic surgery unity in children’s hospital of Rabat.
Materials and Methods
It is a retrospective study over a period of 11 years from October 2011 to December 2022 at the plastic surgery unity in children’s hospital of Rabat, including 30 patients.
This study includes all patients with foot defect who were treated (initially or secondarily).
For our study, we proceeded to the collection of data from the computerized files based on a referral form. We used Excel software for the analytical study.
Results
Among the 30 subjects 66.6% (n=20) were males and the overall average age was 10.23 years (3 months - 17 years)
Most foot defects (60%) were post-traumatic (n=18) such as road accidents, 23% to burns (n=7), and 17% other (n=5) were due to a plantar ulcer or fulminant purpura.
73% (n=22) of patients consulted immediately while 27% (n=8) consulted late after a first consultation in another structure than our department.
The most observed localization was the foot’s back (50%, n=15), then the heel (34%, n=10). The other localizations were the ankle, the foot’s plant, the toes, and the whole foot (Figure 1).
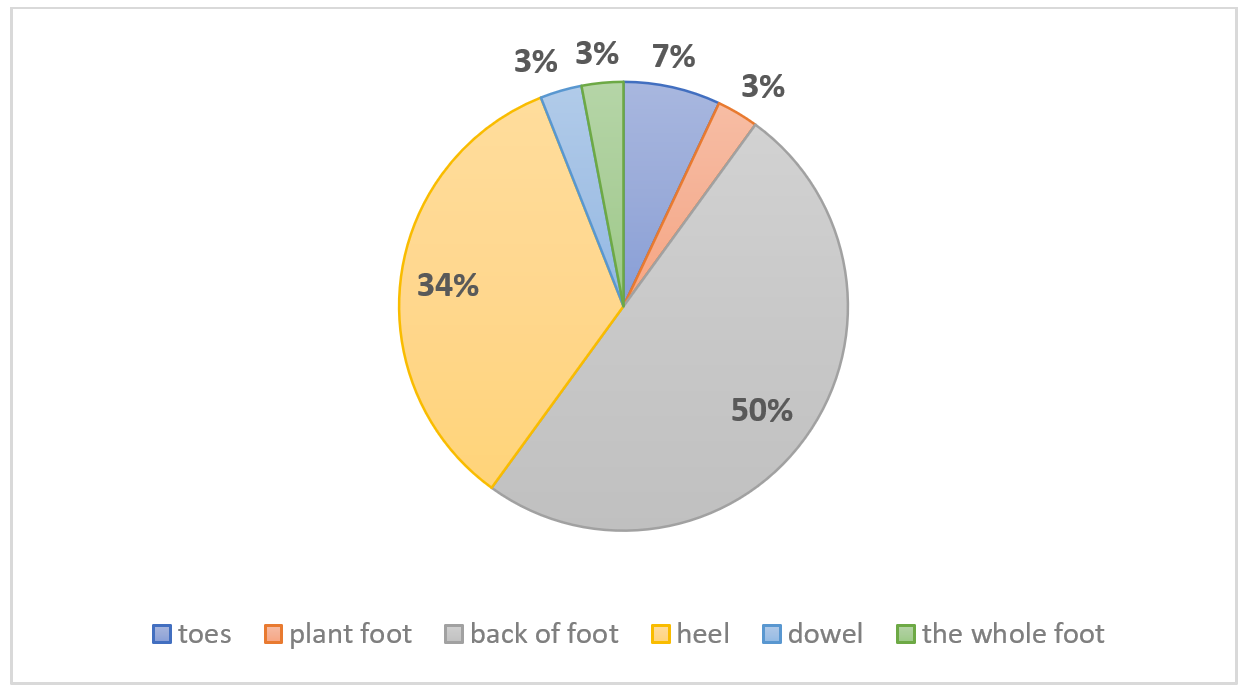
Figure 1: Topography of foot defect in our study.
We used full thickness skin graft for 27% of patient (n=8), split thickness skin graft for 27% (n=8). 17% (n=5) were under secondary healing, sural flap was used for 17% (n=5) of patient. Plantar flap was used for 6% (n=2), while comissuroplasty, net graft and were used for each of the two rest patients (Figure 2).
Table 1: Surgical techniques used for our patients.
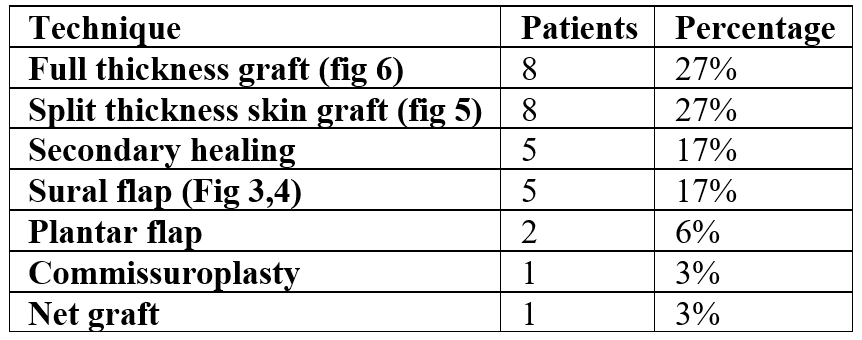

Figure 2: Sural Flap.
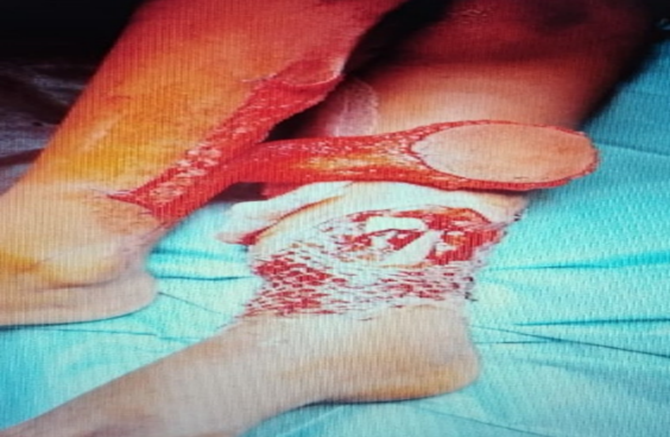
Figure 3: Cross leg.

Figure 4: Split thickness skin graft.

Figure 5 : Full thickness graft.
Treatment outcomes: For the surgical team 70% of the results were good, and 30% of the results were average, while for the family/patient, 33% of the results were judged good, 60% average and 7% of the families/patients were not satisfied with the results.
This evaluation is based on two factors for the surgical team: the functional quality of the foot and the quality of the tissue covering the lesioned area. For the patient's family, the evaluation is centered mostly on the aesthetic aspect.
Discussion
Children, like adults, can be victims of a foot defect. The child’s growth potential gives him particularities in terms of healing. The defect can be caused by different etiologies: trauma, infection, iatrogenic (by an accident of drug subcutaneous extravasation), plantar ulcer, burn, bite, tumor… [1].
The objective of the treatment is to cover the noble elements (bone, tendon, vessels) [2].
The first step is trimming or debridement that correspond to the cleaning of the wound, by excising the necrotic tissues, in order to avoid bacterial proliferation and infection with the aim to promote healing [3].
If the local conditions of the tissues allows it and the sutures can be performed without tension, they are made layer by layer, starting with the muscle, then the aponeurosis, the subcutaneous tissue and finally the skin [3].
In children, the results of secondary healing are impressive, given the extremely rapid regeneration of the skin coverage compared to the adults. Secondary healing is based on the use of the natural healing properties, and it can be helped by conventional or negative pressure dressings. This technique can be used when the noble elements are not exposed. [4].
Skin grafts can also be used to cover a foot defect, by using a skin fragment separated from its donor site to be on a recipient site intended to revascularize it spontaneously. It is only possible if the defect is properly vascularized. There are several types of graft: a full thickness skin graft, a split thickness skin graft [5].
The flaps present themselves as an alternative:
- Local flaps: These flaps rely on the dermis vascularization. They can be performed on the entire skin surface. {Bipedicuar flap, Rotation (or Z) flaps, Special cases of the toes: Hueston flap, Medial plantar flap,) [6]. They are indicated for the minimal defect.
- For extensive defect, loco regional flaps are the ideal solution: neuro-sural flap, external supra-malleolar flap (mobilization of this flap allows us to cover the heel and malleolar region, the instep, and the medial-tarsal region), short fibular flap (Its only indication is to cover Achilles tendon’s exposure), posterior fascio-Musculo-cutaneous flap of the leg, cross-leg [7].
The use of free flaps to cover defects has become common in reconstructive surgery when the locoregional flaps are impossible to use free latissimus dorsi flap, free serratus anterior flap, anterolateral thigh flap [8,9].
Conclusion
Foot defect in children is a challenge for the surgeon. There are several techniques to manage it. When the noble elements are not exposed, we proceed to the Secondary Healing. If there is a minor defect and sutures can be achieved without tension, they remain the ideal solution; otherwise, local flaps seem to solve the problem. For larger defects, locoregional flaps and free flaps are the best solution.
Declarations section:
- Abreviation list: None
- Ethics approval and consent to participate: This study reflects every day clinical practice, and therefore, ethics approval was granted.
- Consent for publication: A consent was obtained from the parents for anonymous publication cases
- Competing interests: The authors declare the absence of any conflict of interest
- Funding: No funding was required for this study
- Data availability: Please contact author for data requests
- Authors contribution:
- Ismail Benomar and Nawfal Fejjal performed the surgical procedures for the patients.
- Ismail Benomar,Chaimae Ben Driss, Souha Qarouach, Fadoua Boughaleb, Abdarahamne Lemhaba and Ghita El Moulihi, wrote the article.
- Nawfal Fejjal approved the final version.
- Acknowledgment: None
References
- Peden M, et al. Rapport mondial sur la prévention des traumatismes chez l’enfant. 2009.
- Leemrijse T, Besse JL, Valtin BDB. Patho du Pied Et De La Cheville. Elsevier Masson SAS; 2015.
- Courbier R, Monties JR, Villani R, Henry E. Experimental study of tissue reactions to suture thread. Mars Chir, 1964; 16: 391-402.
- Plancq MC, Goffinet L, Duquennoy-Martinot V. Les spécificités de la brûlure chez l’enfant. Ann Chir Plast Esthétique, 2016; 61(5): 568-577. DOI: 10.1016/J.ANPLAS.2016.06.009.
- Engelhardt TO, Djedovic G, Pierer G, Rieger UM. The art of skin graft inset in the treatment of full-thickness burns and postburn contractures in the pediatric palm. J Burn Care Res, 2012; 33(4): 222-224. DOI: 10.1097/BCR.0b013e318248b410.
- Reconstruction of scar contractures by using multiple z-plasties. Download Scientific Diagram.
- Belmahi A, El Mazouz S, Gharib N, Oufkir A, Benazzou S. The fasciomusculocutaneous flap at the leg. About 9 clinical cases. Ann Chir Plast Esthet, 2003; 48(3): 173-179. DOI: 10.1016/s0294-1260(03)00042-6.
- Bayol JC, Sury F, Petraud A, Laure B, Goga D. The free anterolateral thigh flap for head and neck reconstruction: Technical particularities of the harvesting and results about six cases. Ann Chir Plast Esthet, 2011; 56(6): 504-511. DOI: 10.1016/j.anplas.2009.12.004. Epub 2010 Jun 18.
- Gasnier P. Technique du «cross-leg».

