Surgical Management of Bronchial Dilatation in Children
Ochan M1,2, Benomar I1,2,*, Zitan H1,2, Boulajrouf J1,2, Hadir M1,2 and Kisra M1,2
1Department of pediatric surgery A, Children Hospital of Rabat, Morocco
2Faculty of medicine and pharmacy, Mohamed V University, Rabat, Morocco
Received Date: 02/06/2024; Published Date: 03/10/2024
*Corresponding author: Benomar Ismail, Department of pediatric surgery A, Children Hospital of Rabat, Faculty of medicine and pharmacy, Mohamed V University, Rabat, Morocco
Abstract
Introduction: Bronchiectasis is characterized by irreversible enlargement of subsegmental bronchi, often associated with structural deterioration. This study retrospectively analyzes bronchiectasis cases treated surgically at Rabat Children's Hospital. The aim is to elucidate demographics, clinical presentation, imaging findings, treatment modalities, and outcomes, emphasizing the importance of prevention.
Methods: Nineteen bronchiectasis cases undergoing surgical intervention at Rabat Children's Hospital between 2013 and 2023 were reviewed. Data on demographics, symptoms, imaging, treatment, and outcomes were collected and analyzed. Treatment consisted of preparatory phases including antibiotics and physiotherapy, followed by surgical intervention. Surgical indications, procedures performed, immediate postoperative outcomes, and long-term follow-up were assessed.
Results: The average age at diagnosis was 7.5 years, with a slight female predominance. Common symptoms included chronic cough, fever, bronchorrhea, and hemoptysis. Thoracic CT scans confirmed bronchiectasis in all cases. Surgical indications included recurrent infections, hemoptysis, parenchymal destruction, and bronchorrhea. Lobectomies, bilobectomies, and segmentectomies were the main surgical procedures performed, with no perioperative mortality. Immediate postoperative outcomes were uneventful in all cases. Long-term outcomes were favorable in 95% of cases, with only 5% experiencing disease recurrence.
Discussion: The study highlights the efficacy of surgical intervention in managing bronchiectasis, particularly in cases resistant to medical treatment or with severe complications. The importance of early detection, prompt treatment, and prevention through awareness of associated risk factors is emphasized. Surgical approaches tailored to individual patient characteristics contribute to favorable outcomes and reduced recurrence rates.
Conclusion: Surgical intervention plays a crucial role in managing bronchiectasis, offering favorable outcomes with low recurrence rates. However, emphasis should be placed on prevention through awareness and early intervention. Further research is needed to optimize surgical techniques and refine treatment strategies for better long-term outcomes in pediatric bronchiectasis.
Keywords: Bronchiectasis; Diagnosis; Surgical treatment
Introduction
Bronchiectasis is a chronic condition resulting from the destruction of the chondro-musculo-elastic framework, leading to irreversible dilation of the sub-segmental bronchi and can affect different lung territories [1]. History taking and clinical examination may suggest the diagnosis, but confirmation is made by computed tomography (CT) scan [2]. Surgery is reserved for complicated and localized forms and consists of lobectomy [3]. The aim of this study is to highlight the role of surgery in the management of bronchiectasis, to determine preventive measures, and to analyze the clinical and paraclinical evolution of this disease, while comparing our results with data from the medical literature.
Materials and Methods
This is a retrospective study conducted in the Surgery Department A at the Children's Hospital of Rabat between June 2013 and June 2023.
- Inclusion criteria:
- Patients between 0 and 15 years old, who present bronchial dilation, whether diffuse or localized, and who have undergone surgical intervention.
- Exclusion criteria:
- Patients who have not undergone surgery
- Incomplète médical records.
Results
We collected data from 19 patients. The average age of our patients ranged from 1 to 14 years with a mean of 7.5 years. We observed a predominance in the age group between 2 and 5 years (37%) (Figure 1). Female sex predominated with 53%, accounting for 10 cases, with a sex ratio of 0.9 (Figure 2).
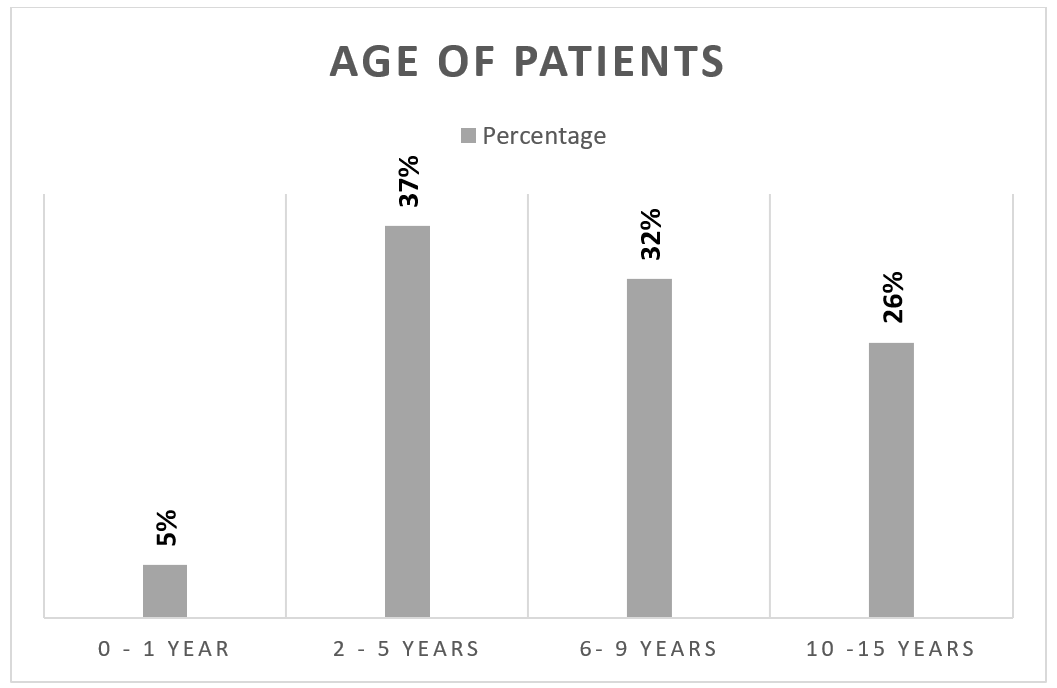
Figure 1: Age of Patients.
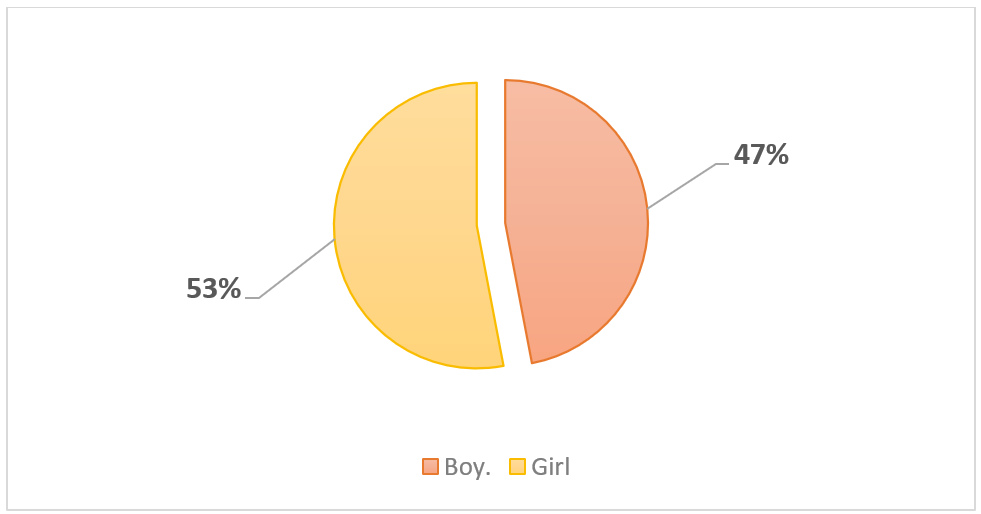
Figure 2: Sex of patients.
Among our 19 patients, medical history was predominantly characterized by foreign body inhalation in 48% of cases (n=9) and recurrent pneumonias in 26% of cases (n=5) (Figure 3).
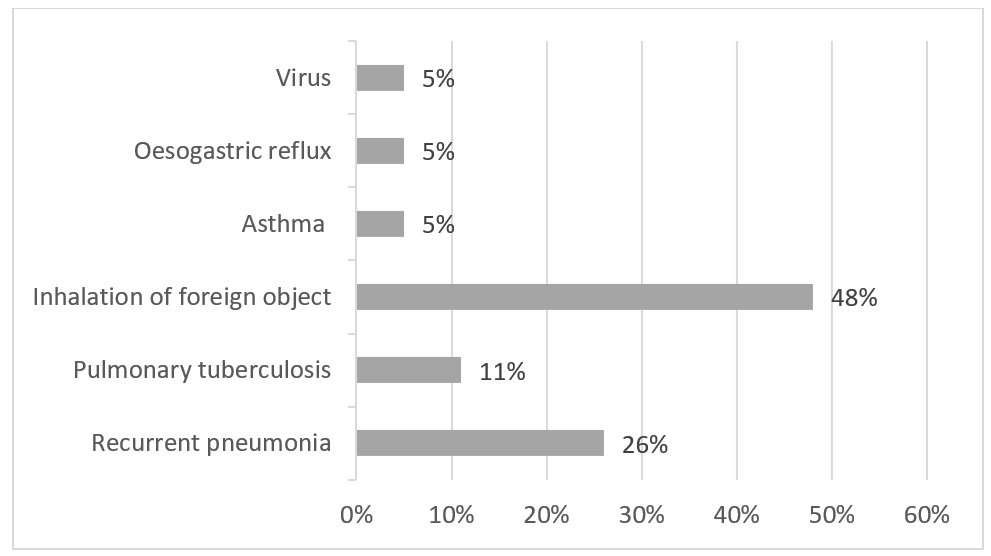
Figure 3: Medical History of patients.
All our patients were symptomatic. Clinical examination was normal in 13 of our patients, while we found snoring rales in 31.5% of patients, crepitus rales in 15.7%, sibilant rales in 10.5%.
Biologically, we found hypochromic microcytic anemia in 52.6% of patients. Detection of Koch Bacilli (BK) in sputum was positive in 10.5% (n=2) of cases. Cytobacteriological examination of sputum revealed Haemophilus influenzae in 2 patients and alpha-hemolytic streptococcus in 1 patient.
Radiologically, each patient underwent at least one frontal and lateral chest X-ray before surgery. In 33% of case, the results were normal, while in 76%, they were abnormal (Figure 4). We also noted that the left side was the most affected in our series (63% of cases).
All patients underwent computed tomography (CT), which detected specific bronchiectasis lesions in all cases (100%) (Figure 6) .
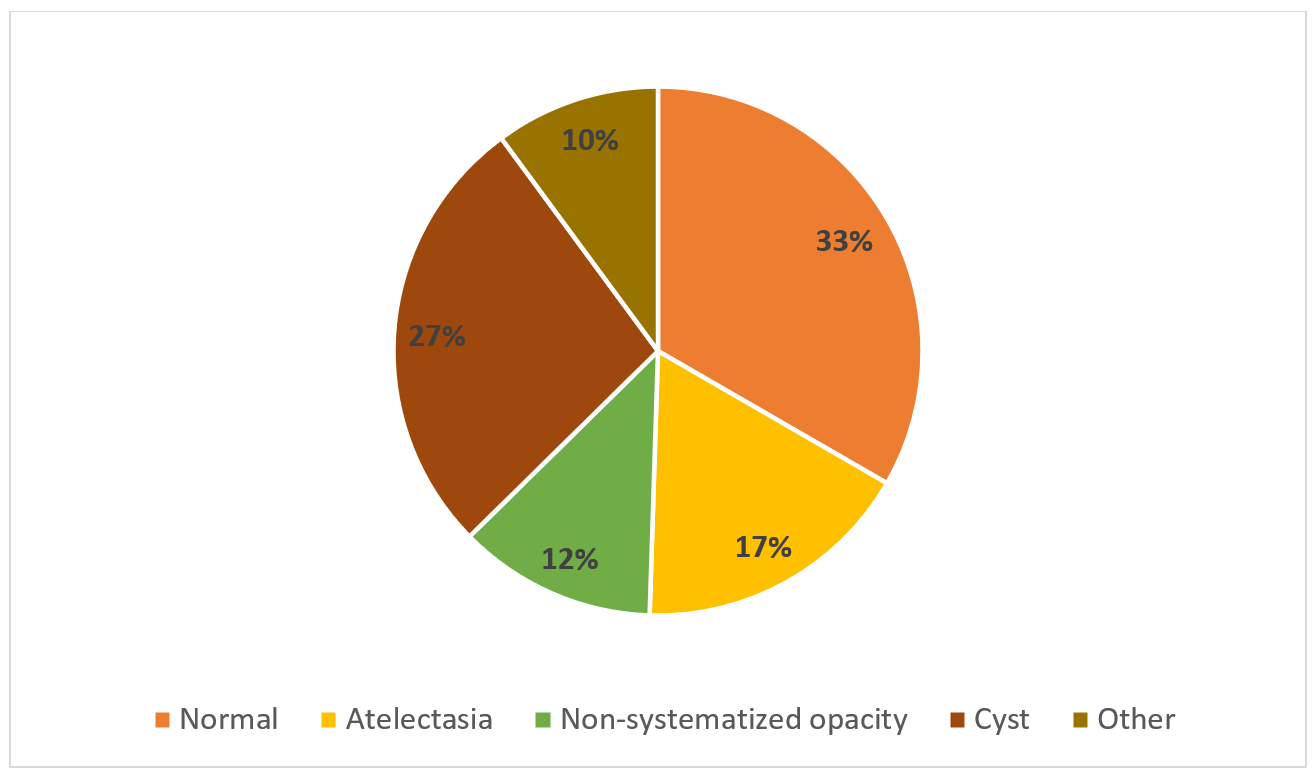
Figure 4: Result of X-Ray.

Figure 5: Non-Systematized opacity.
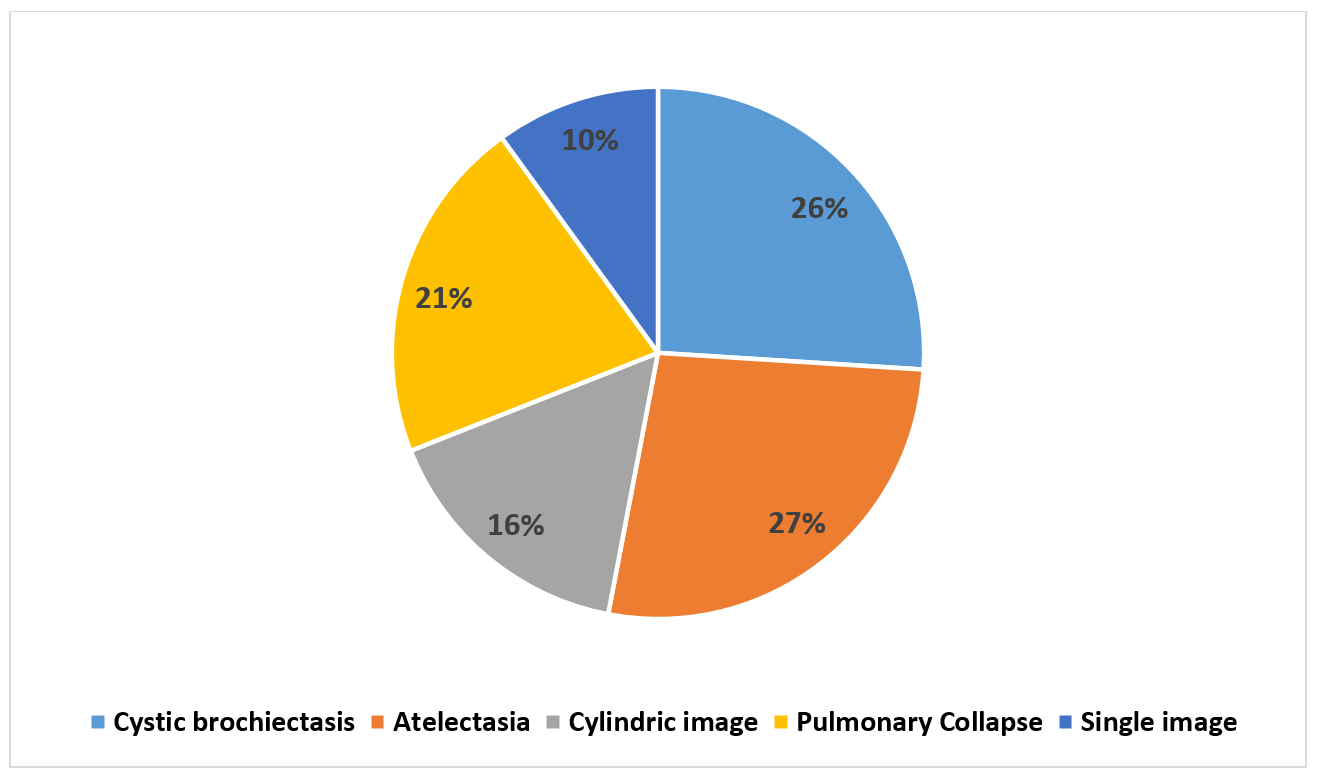
Figure 6: Result of computed tomography.
Figure 7: Pulmonary collapse.

Figure 8: Cystic bronchiectasis.
Figure 9: Cystic bronchiectasis.
There is concordance between the results of standard X-rays and CT scans, with a more specific study of lesions on the CT scan. Out of the 19 patients included in the study, bronchoscopy was performed in at least 13 of them, accounting for 68.4% of cases. In all cases, bronchoscopy revealed a first-degree inflammatory aspect of the affected bronchus. Purulent secretions were observed in 27% of patients, while bronchoscopy was without apparent abnormalities in 18% of patients. Segmental stenosis was detected in 9% of patients, while a foreign body was found in 54% of cases.
Perfusion lung scintigraphy was performed in 2 patients and showed a perfusion defect, while pulmonary function testing was conducted in 2 patients, revealing a discreet restrictive syndrome in only one patient.
- Therapeutic Management:
- Medical: All patients received antibiotic therapy + corticosteroids + mucolytics. Two patients also received anti-tubercular treatment.
- Physiotherapy: A cornerstone in the management of bronchiectasis, all our patients underwent daily sessions of respiratory physiotherapy.
- Surgery: In our series, the interval between diagnosis and surgery was 1.25 years. The objective of surgery in our series was either cure or at least improvement in the quality of life of our patients. Indications were as follows: recurrent pneumonia in 32% (N=6), recurrent or life-threatening hemoptysis (n=5) in 26% of cases, disabling chronic bronchorrhea in 21% of cases (n=4), and total destruction of lung parenchyma in 21% of cases (n=4).
In our series, surgery consisted of lobectomy in 79% of cases (n=15), segmentectomy in 16% of cases (n=3), and pneumectomy in 5% of cases (n=1).
Postoperative outcomes were uncomplicated in all patients with removal of the thoracic drain at day 5.
Long-term outcomes were categorized as follows:
- Excellent: 9 patients showed complete resolution of symptoms, allowing them to lead a normal life without any restrictions.
- Very good: 7 patients experienced occasional episodes of hemoptysis or respiratory infections, but these symptoms did not impede their ability to lead a normal life without restriction.
- Improvement: 2 patients showed improvement in symptoms, although it did not allow them to lead a normal life without constraints.
- Failure: 1 patient experienced recurrence of symptoms, indicating failure of the procedure.
Discussion
The incidence and prevalence of bronchiectasis remain unknown [4]. The average age reported in the literature is 10.5 years [5], while in our series; the average age was 7.5 years. We observed a female predominance [6], which is consistent with other studies. Clinical examination plays an important role and can reveal thoracic deformities and bronchial wheezes [7].
Paraclinical examination serves three purposes: confirming the diagnosis, assessing pulmonary function, and searching for etiology [8]. Literature suggests the use of laboratory tests to detect infectious origins, chest X-rays and CT scans for diagnosis and assessment of pulmonary architecture, perfusion lung scintigraphy, and respiratory functional exploration to evaluate respiratory function [9].
Therapeutic management includes several components. Respiratory physiotherapy and antibiotics are recommended only during exacerbations. Antibiotic therapy should cover the most common pathogens, including Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis. Azithromycin as maintenance therapy in children halves the frequency of exacerbations compared to placebo [9]. The aim of surgical treatment is to improve the patient's quality of life after failed medical treatment and manage complications, ultimately breaking the vicious circle described by Cole through excision of the suppurative zone while preserving as much healthy tissue as possible [10].
It is crucial not to delay surgical intervention, especially in localized disease, as early intervention offers better chances of complete remission. Preoperative bronchoscopy is strongly recommended to rule out mechanical obstruction responsible for bronchiectasis. Cardiac function evaluation is also recommended since studies have shown frequent impairment of both right and left ventricular functions in bronchiectasis patients [10].
Postero-lateral thoracotomy is a basic surgical approach that must be performed with scrupulous respect for thoracic wall anatomy to avoid sequelae. However, deciding on surgical indication requires ensuring that the intervention can be successfully performed from both a functional and anatomical perspective. Pulmonary function assessments and imaging examinations are essential for surgical indication and determining which areas must be respected.
We aimed to compare predominant surgical indications in our series with those reported by Dr. Haci Ibrahim Oglu in Turkey [5] and Dr. Ibrahim Otgun [11]. We found that recurrent respiratory infections remain the primary indication for surgery in our series, while bronchorrhea is less frequent but six times more common than in other series. This observation can likely be attributed to better compliance with medical treatment and regular physiotherapy sessions among our patients.
From this analysis, it emerges that isolated lobectomy is the most commonly performed surgical procedure by all authors. However, we observed that segmentectomies are much more common in our series than in others, likely due to late diagnosis or extensive lesions that no longer allow limited resections. Pneumectomies are very rare in our series compared to others.
Conclusion
Bronchial dilation is a condition characterized by a permanent and irreversible increase in the diameter of sub-segmental bronchi, resulting from alterations in their chondro-musculo-elastic structure, which can affect unilateral or bilateral areas.
The results of this study indicate that surgery to treat bronchial dilations is an extremely effective approach, leading to cure or improvement in the condition of 92% of patients.
The treatment of this condition primarily relies on medical means aiming to both cure and prevent, with the goal of reducing bacterial colonization of the bronchi and decreasing bronchial inflammation.
Once it is determined surgical intervention is necessary, the patient must undergo a comprehensive evaluation of their lesions, both clinically and through medical imaging, to precisely define the areas for resection. It is essential to perform as complete a resection as possible while preserving as much healthy lung parenchyma as possible.
References
- Bird K, Memon J Bronchiectasis. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024.
- Chang AB, Fortescue R, Grimwood K, et al. European Respiratory Society guidelines for the management of children and adolescents with bronchiectasis. Eur Respir J, 2021; 58(2): 2002990. doi:10.1183/13993003.02990-2020.
- Kumar A, Lodha R, Kumar P, Kabra SK. Non-cystic fibrosis bronchiectasis in children: clinical profile, etiology and outcome. Indian Pediatr, 2015; 52(1): 35-37. doi:10.1007/s13312-015-0563-8.
- Fall A, Spencer D. Paediatric bronchiectasis in Europe: what now and where next? Paediatr Respir Rev, 2006; 7(4): 268-274. doi: 10.1016/j.prrv.2006.05.003.
- Gokhan Haciibrahimoglu, Mithat Fazlioglu, Aysun Olcmen, Atilla Gurses, Mehmet Ali Bedirhan. Surgical management of childhood bronchiectasis due to infectious disease. J Thorac Cardiovasc Surg, 2004; 127: 1361-1365; 0022-5223.
- Karadag B, Karakoc F, Ersu R, Kut A, Bakac S, Dagli E. Non-cystic-fibrosis bronchiectasis in children: a persisting problem in developing countries. Respiration, 2005; 72(3): 233-238. doi:10.1159/000085362.
- Kim HY, Kwon JW, Seo J, et al. Bronchiectasis in children: 10-year experience at a single institution. Allergy Asthma Immunol Res, 2011; 3(1): 39-45. doi:10.4168/aair.2011.3.1.39.
- Li AM, Sonnappa S, Lex C, et al. Non-CF bronchiectasis: does knowing the aetiology lead to changes in management? Eur Respir J, 2005; 26(1): 8-14. doi:10.1183/09031936.05.00127704.
- Kelly C, Chalmers JD, Crossingham I, et al. Macrolide antibiotics for bronchiectasis. Cochrane Database Syst Rev, 2018; 3(3): CD012406. doi: 10.1002/14651858.CD012406.pub2
- Jancovici R, Pons F, Pailler JL. Interventions en chirurgie thoracique : la chirurgie endoscopique. Collection chirurgie pratique. Masson 67-71th.
- I˙brahim Otgun, Ibrahim Karnak F, Cahit Tanyel M, Emin S Enocak, Nebil Buyu kpamukcu. Surgical Treatment of Bronchiectasis in Children. Journal of Pediatric Surgery, 2004; 39(10): pp 1532-1536.

