Effect of Regional Anaesthesia on Cognitive Function Among the Post Operative Cabg Patients
Kamalakkannan Ganapathy Sambandam1, Ranjith Karthekeyan B1,*, Saranya Nagalingam1, Rajesh Kumar Kodali2, Saranya Logaraj2 and Kiran Muthu Rajah1
1Department of Cardiac Anaesthesia, Sri Ramachandra Institute of Higher Education and Research (SRIHER), India
2Department of Anaesthesia, Sri Ramachandra Institute of Higher Education and Research (SRIHER), India
Received Date: 01/04/2024; Published Date: 26/08/2024
*Corresponding author: Professor and HOD, Department of Cardiac Anaesthesia, Sri Ramachandra Institute of Higher Education and Research (SRIHER), Ramachandra Nagar, Porur, Chennai-600116.India
Orcid- 0000-0001-7025-0134
Abstract
Background: Postoperative cognitive dysfunction (POCD) is a common complication after coronary artery bypass graft surgery. The use of opioids is associated with greater incidence of postoperative cognitive dysfunction compared to regional techniques.
Aim: The aim of the study is to compare the post-operative cognitive function among the patient undergoing off pump CABG with or without facial plane block.
Methodology: Type of study: Prospective observational study.
Place of study: Sri Ramachandra institute of higher education and research.
Sample size: The sample size was calculated n= 36 with 30 in each group, with a power of 95% and alpha error of 5%. After getting informed written consent a total number of 60 patients were enrolled in this study, which is further divided into 2 groups. Group A received bilateral Erector spinae plane block with 0.25% Bupivacaine+ Dexmedetomidine 1mics/kg divided into both sides (25 ml on each side). GROUP B received conventional opioid Fentanyl 1 to 2mics/hr. Both groups received Dexmedetomidine 0.1mic/kg/min infusion.
Procedure: After overnight fasting all the patients were premedicated with Tab.Diazepam 10mg PO HS / 6am and Tab.Pantaprazole 40mg PO HS / 6 am. General anaesthesia was induced after securing IV, artery and CV line as per hospital protocol. For induction Midazolam 1mg, Fentanyl 2-3mics/kg, Thiopentone 3-5mg/kg, Sevoflurane 1-2% and paralysed with Vecuronium 0.1mg/kg. Post induction all the patients were started with Dexmedetomidine 0.1mics/kg/hr infusion. Group A patient received bilateral ESP on the left lateral position. Maintained with Sevoflurane 1-2%, Fentanyl 1-2mic/kg on demand, Vecuronium ¼ ‘th of induction dose. All patients had undergone mini mental state examinations scoring system on postoperative day 1 in ICU and day 5 in the ward.
Results: There was no statistical significance among the age, sex, height and weight between the group. The MMSE score among the group A on POD 1 was significant, but POD 6 score were not significant between the groups. Post-operative Fentanyl usage was significantly lower among the group A, but there was no difference found in the intra-operative Fentanyl requirement. The length of ICU and hospital stay was not showed any significance among Groups. Based on the cognitive assessment by MMSE on POD 1 showed better score in ESP block patients, but those without ESP block had low MMSE score. From this regional block helps to improve post-operative cognitive function by means of reduced opioid usage.
Conclusion: Early postoperative cognitive score was better among the patient who received regional anaesthesia. Opioid conception also less in those had regional anaesthesia.
Keywords: Post-Operative Cognitive Dysfunction (POCD); Post CABG, Elderly; Regional Anesthesia; ESP Block; OPCABG
Introduction
Cardiac surgery, particularly Coronary Artery Bypass Grafting (CABG), is a common procedure for treating coronary artery disease. While advancements in surgical techniques have improved patient outcomes, concerns about postoperative cognitive dysfunction (POCD) remain. POCD is a condition characterized by a decline in cognitive function after surgery, impacting memory, attention, and other cognitive domains. Recognizing the potential impact of anaesthesia on cognitive outcomes, researchers have explored alternative approaches, such as regional anaesthesia, to mitigate the risk of POCD in postoperative CABG patients [1,2].
Regional anaesthesia involves the administration of anaesthetics to specific regions of the body, effectively blocking nerve signals and providing analgesia. The potential neuroprotective effects of regional anaesthesia, compared to general anaesthesia, have been a subject of growing interest in the medical community. The rationale behind this exploration lies in the avoidance of systemic effects associated with general anaesthesia, such as inflammation, oxidative stress, and alterations in cerebral blood flow—all of which have been implicated in the development of cognitive dysfunction.
The impact of regional anaesthesia on cognitive function among postoperative CABG patients is a subject that warrants comprehensive investigation. Several studies have explored the relationship between the type of anaesthesia used during surgery and the subsequent cognitive outcomes in various patient populations. However, the specific effects of regional anaesthesia on cognitive function in the context of CABG surgery remain a relatively underexplored area [3-5].
Several studies have investigated the impact of regional anaesthesia on cognitive function in various surgical populations, but there is a notable gap in the literature concerning its specific effects on postoperative CABG patients. This study aims to address this gap by examining the relationship between the use of regional anaesthesia during CABG surgery and postoperative cognitive function.
The aim of the study is to find out the effect of cognition function among the patient undergoing off pump coronary artery bypass grafting (CABG) with Erector spine plane (ESP) block.
Primary outcome: Post-operative cognitive score. Secondary outcome: Length of Intensive care unit (ICU) stays and Opioids consumption.
Hypothesis: We hypothesize that CABG patients undergoing regional anaesthesia will exhibit a lower incidence and severity of postoperative cognitive dysfunction compared to those receiving general anaesthesia. Additionally, we anticipate that specific factors related to regional anaesthesia, such as the choice of technique, may influence cognitive outcomes.
Significance/Justification: Understanding the impact of regional anaesthesia on cognitive function in postoperative CABG patients holds significant clinical relevance. If regional anaesthesia proves to be associated with improved cognitive outcomes, it could represent a valuable strategy for minimizing the burden of POCD in a population already susceptible to cardiovascular and neurologic complications.
Objectives:
- To assess the severity of postoperative cognitive dysfunction in CABG patients receiving regional anaesthesia compared to those undergoing general anaesthesia.
- To investigate potential factors influencing cognitive outcomes, such as the type of regional anaesthesia used, duration of surgery, and patient demographics.
- To analyse the existing evidence on the neuro-protective mechanisms of regional anaesthesia and its potential role in mitigating cognitive dysfunction post-CABG.
Materials and Methods
A prospective observational study was conducted on 60 patients who underwent elective OPCABG in Sri Ramachandra Institute of higher education and research hospital between January 2022 to December 2022. Group A (30 patients) received bilateral ESP block with Bupivacaine 0.25% and Dexmedetomidine 1mcg/kg, which was divided into 25 ml on each side on the left lateral position. Group B (30 patients) received routine intravenous Fentanyl 1mcg/kg as required.
Sample Size calculation:
The sample size was calculated using a pilot study. The mean cognition scale score in group A with bilateral erector spinae block was 28.8 and 29.6 on post-operative day 1 and day 6 respectively in a pilot study of 10 CABG patients. The mean cognition scale score in group B without erector spinae block was 24.5 and 28 on postoperative day 1 and day 6 respectively in a pilot study of 10 CABG patients. The standard deviation for group A was assumed to be 3.6 and group B to be 3.6 with an attrition of 10%. Based on above calculation the sample size was calculated a total of 36 patients, 18 in each group, with a power of 95% and alpha error of 5%.
Inclusion criteria: age < 70 years, ASA 3, elective OPCABG, EF >45%.
Exclusion criteria: Age > 70 years, emergency surgery, history of persisting neuro cognitive disorders and spine surgery or spinal abnormalities, allergy to local anaesthetic, uneducated patients, EF<45%.
Once patients fulfil the inclusion criteria, they all fasted for 8 hrs and premedicated with T.Diazepam 10 mg and T.Pantaprazole 40 mg, PO at 9 pm day before surgery and 6 am on the day of surgery.
After connecting standard monitoring, intravenous (IV), radial artery and internal jugular lines were secured under local anaesthesia. Prophylactic antibiotic covered with inj.Cefuroxime 1.5gm IV given immediately after IV line in place. General anaesthesia induced with O2 6lit/min, inj. Midazolam 1mg, Inj. Fentanyl 2-3mcg/kg, Inj. Thiopentone 3-5mg/kg, Inj. Vecuronium 0.1mg/kg and Sevoflurane 1-2%. After 3 min, once the BIS < 50, Intubated with appropriative size endotracheal tube (8.5 ID for male and 7.5 ID for female). Post intubation both groups received injection Dexmedetomidine 0.1mcg/kg/hr infusion, which was continued post-operatively up to first 24 hrs in ICU.
Anaesthesia was maintained with oxygen and air (50:50), Sevoflurane 1-2%, inj. Fentanyl 1mcg/kg (was given if the heart rate and blood pressure rise more than 15% from the baseline value). Muscle relaxant with inj. Vecuronium ¼ of the induction dose was given every 30 min. Anaesthesia depth was monitored by Bispectral index (BIS), which was maintained between 40 to 60 throughout the surgery.
Group A received ultrasound guided bilateral ESP block on the left lateral position. All the patient underwent OPCABG by the same surgeon through midline sternotomy. Both groups received Injection Fentanyl 1mcg/kg as rescue analgesia for both intra and post operatively.
Postoperatively patients were shifted to postoperative ICU and fast tracked based on the hospital protocol. Postoperative analgesia was maintained with intravenous Paracetamol 1gm q8h and intravenous Fentanyl 1mcg/kg to keep the VAS (Visual analogue scale) score lesser than 4.
Two hours post extubation all the patients were assessed for cognition function on POD 1 and POD 6 using the Mini-Mental Status Examination (MMSE). It is a simple pen‐and‐paper test of cognitive function based on a total possible score of 30 points. It tests orientation, concentration, attention, verbal memory, naming and visuospatial skills. Normal 25 to 30, but value below 25 is considered as POCD. Advantages: rapid administration, availability of multiple language translations and high levels of acceptance.
Statistical analysis: Data were presented as mean, standard deviation, frequency and percentage. Continuable variables were compared using independent sample ‘t’ test. Categorical variables were compared using Pearson chi-square test. Data analysis was performed using IBM-SPSS version 21.0 (IBM-SPSS Science Inc.., Chicago, IL).
Results
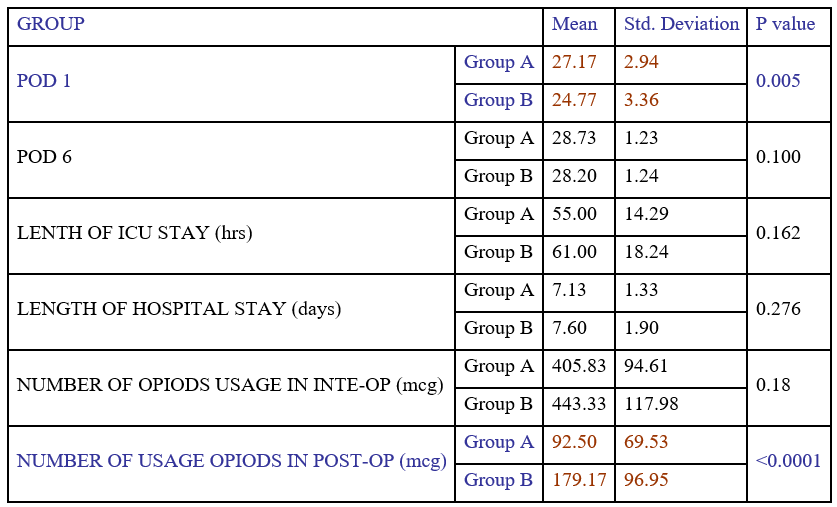
The males and females in the study were 24, 6 in group A and 21, 9 in group B. (Table – 1). There was no statistical significance among the age, sex, height and weight between the group. (Table – 2) The MMSE score among the group A on POD 1 was significant, but POD 6 score were not significant between the groups. Post-operative Fentanyl usage was significantly lower among the group A, but there was no difference found in the intra-operative Fentanyl requirement. The length of ICU and hospital stay was not showed any significance among Groups. Based on the cognitive assessment by MMSE on POD 1 showed better score (Group A – 27.17 and Group B - 24.77) in ESP block patients, but those without ESP block had low MMSE score. From this regional block helps to improve post operative cognitive function by means of reduced opioid usage. (Group A – 92.5 and Group B – 179.17)
Table 1: Demographic factors.
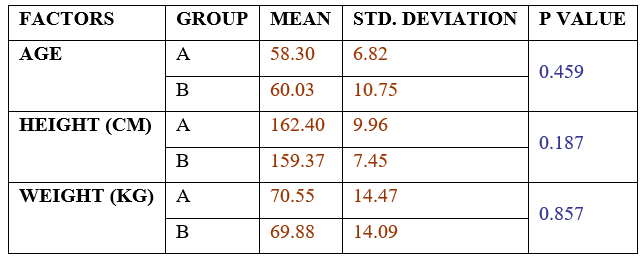
Table 2: MMSC scoring with opioid usage and hospital stay.
Discussion
The findings we have presented suggests that post-operative Fentanyl usage was significantly lower in Group A, where patients received an Erector Spinae Plane (ESP) block. However, there was no observed difference in intra-operative Fentanyl requirement. Additionally, the length of ICU and hospital stay did not show any significant differences between groups. A notable aspect is the cognitive assessment using the Mini-Mental State Examination (MMSE) on Postoperative Day 1 (POD 1), where patients who received the ESP block demonstrated better cognitive scores compared to those without the block [6,7].
This raises interesting implications for the role of regional blocks, specifically the ESP block, in improving postoperative cognitive function by reducing opioid usage. The significant reduction in postoperative Fentanyl usage in patients who received the ESP block aligns with the growing interest in regional anesthesia techniques as an effective means of pain management. Regional blocks target specific nerve pathways, providing targeted analgesia and reducing the need for systemic opioids, which are known to have cognitive side effects. The absence of a difference in intra-operative Fentanyl requirement may suggest that the ESP block primarily influences the postoperative phase rather than the immediate intra-operative period. This could be due to the time needed for the regional block to take effect.
Based on the study by Cao et al we chose MMSE for cognitive evaluation as most of our patients belonged to geriatric population. He showed that MMSE can be used for risk stratification and prognosis evaluation in the geriatric surgical population [8]. A retrospective study done by Ge Y et al. demonstrated that CABG is the most common cause of POCD after a cardiac operation on POD 7 and 3 months later [9], in our study also showed similar finding on POD 1, but failed to demonstrate the same on POD 6. There was no difference between off pump CABG and on pump CABG as per Yuan SM [10]. We took only OPCABG to see the effect of facial plane block on POCD, but excluded the on-pump CABG in view of neurovascular insult caused by Cardiopulmonary bypass exposure [11]. We used Dexmedetomidine as a sedative for all patient because it reduces the post operative cognitive dysfunction, which was similar to Catia et al study, but our study we combined ESP block with Dexmedetomidine showed better cognitive function [12]. The lack of significant differences in the length of ICU and hospital stay between groups may imply that the impact of the ESP block on opioid usage and cognitive function may not directly translate into shorter hospital stays. Other factors, such as surgical complexity or patient comorbidities, could contribute to the overall length of hospitalization [13,14]. The improved MMSE scores in patients who received the ESP block on POD 1 suggest a potential cognitive benefit associated with reduced opioid usage. Opioids are known to have central nervous system effects, including sedation and cognitive impairment. The better cognitive scores in the ESP block group could be attributed to the sparing effect on opioid consumption. These findings have clinical implications for enhancing postoperative recovery by minimizing opioid-related cognitive side effects. Future research could explore the long-term cognitive outcomes, potential differences in various types of surgeries, and the cost-effectiveness of incorporating regional blocks into perioperative care [15,16]. The study provided valuable insights into the potential benefits of incorporating ESP blocks to reduce postoperative opioid usage and improve early cognitive function. Further research and exploration of these findings in diverse surgical populations are warranted to establish the broader applicability and long-term implications of regional blocks on postoperative outcomes.
Conclusion
Immediate postoperative cognitive score was better among the patient who undergone OPCABG with ESP block and the postoperative opioid requirement also less among these patients. Length of ICU and hospital stay was not benefited by regional anaesthesia.
Limitations: Preoperative MMSE would have helped to identify patient with mild cognitive dysfunction. A prospective randomised single blind trial would reduce the observer bias and the confounding factors. Adding cerebral biomarkers along with MMSE may give added weightage to this study. We did MMSE for 6 post-operatively days only, instead of that a yearlong follow-up should give better understanding about POCD.
References
- Monk TG, Weldon BC, Garvan CW, et al. Predictors of cognitive dysfunction after major noncardiac surgery. Anesthesiology, 2008; 108(1): 18-30.
- Rasmussen LS, Larsen K, Houx P, et al. The assessment of postoperative cognitive function. Acta Anaesthesiol Scand, 2001; 45(3): 275-289.
- Royse CF, Andrews DT, Newman SN, et al. The influence of propofol or desflurane on postoperative cognitive dysfunction in patients undergoing coronary artery bypass surgery. Anaesthesia, 2011; 66(6): 455-464.
- Evered L, Silbert B, Scott DA, et al. Postoperative Cognitive Dysfunction is Independent of Type of Surgery and Anesthetic. Anesth Analg, 2011; 112(5): 1179-1185.
- Wang Y, Sands LP, Vaurio L, et al. The effects of postoperative pain and its management on postoperative cognitive dysfunction. Am J Geriatr Psychiatry, 2007; 15(1): 50-59.
- Evered L, Silbert B, Scott DA, Knopman DS, Knopman D, DeKosky ST, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Anesthesiology, 2018; 129: 872–879.
- Greaves D, Ross TJ, Ghezzi ES, Keage HAD, Psaltis PJ, Davis DHJ, et al. Risk factors for delirium and cognitive decline following coronary artery bypass grafting surgery: a systematic review and meta-analysis. J Am Heart Assoc, 2020; 9: e017275. doi: 10.1161/JAHA.120.017275
- Cao, et al. Effects of an abnormal mini-mental state examination score on postoperative outcomes in geriatric surgical patients: a meta-analysis. BMC Anesthesiology, 2019; 19: 74.
- Ge Y, Ma Z, Shi H, Zhao Y, Gu X, Wei H. Incidence and risk factors of postoperative cognitive dysfunction in patients underwent coronary artery bypass grafting surgery, 2014; 39(10): 1049-1055.
- Yuan SM, Lin H. Postoperative Cognitive Dysfunction. Braz J Cardiovasc Surg, 2019; 34(1): 76-84.
- Diederik, et al. Cognitive outcome after off-pump and on-pump coronary artery graft surgery. JAMA, 2002; 287: 11.
- Catia, et al, Dexmedetomidine reduces postoperative cognitive and behavioural dysfunction in adults submitted to general anesthesia for non-cardiac surgery: meta-analysis of randomized clinical trials. Braz J Anesthesiol, 2021; 71: 413-420.
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med, 2016; 41(5): 621-627. doi:10.1097/AAP.0000000000000451.
- Brummett CM, Waljee JF, Goesling J, et al. New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg, 2017; 152(6): e170504. doi:10.1001/jamasurg.2017.0504.
- Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res, 1975; 12(3): 189-198. doi:10.1016/0022-3956(75)90026-6.
- Audrey Miang, Ying Tan, Derek Amoako. Postoperative cognitive dysfunction after cardiac surgery. Continuing Education in Anaesthesia, Critical Care & Pain j, 2013; 13: 219-223.

