Understanding Exclusive Breastfeeding Practices among Mothers in Nahaki Charsada: Knowledge, Attitudes, and Implementation
Samrina Khan1, Maryam Raza Dar1, Huma Hanif1, Abbas Khan2, Moula Ghulam1, Abdullah1, Karishma Akbar1, Suman Shah1, Salman Ali1 and Nouman Anthony1,*
1Rehman Medical institute, Peshawar, Pakistan
2Combined Military Hospital, Pakistan
Received Date: 27/03/2024; Published Date: 21/08/2024
*Corresponding author: Nouman Anthony, Rehman Medical institute, Peshawar, Pakistan
Abstract
Background and Rationale: Breastfeeding is crucial for a child's health and survival, providing essential nutrients and protection against diseases. However, exclusive breastfeeding rates remain low globally. Understanding exclusive breastfeeding practices among mothers in specific regions, such as Nahaki Charsada, Khyber Pukhtunkhwa (KP), can provide insights into promoting this vital practice. This study aims to explore the knowledge, attitudes, and implementation of exclusive breastfeeding among mothers in Nahaki Charsada.
Methodology: A cross-sectional study design was employed, with 100 mothers selected using nonrandom, convenient sampling. A questionnaire was used to assess knowledge, attitudes, and practices related to exclusive breastfeeding. The data was collected through interviews with mothers conducted by healthcare professionals. Descriptive and inferential statistics were used to analyze the data.
Results: The study revealed that 39% of mothers were following the recommended guidelines for exclusive breastfeeding. Knowledge about exclusive breastfeeding was high, with 99% of participants having prior knowledge. Positive attitudes toward exclusive breastfeeding were observed, with the majority recognizing its positive impact on child health. Only 43% of mothers reported access to social media as an information source. Reasons for choosing bottle feeding over breastfeeding included personal preference (28%) and work or lifestyle demands (19%).
Conclusion: The study underscores the need for targeted educational interventions to improve exclusive breastfeeding rates in Nahaki Charsada. Strategies should address maternal knowledge, attitudes, and misconceptions and leverage diverse information sources to promote exclusive breastfeeding effectively. These findings can serve as a basis for evidence-based policies to support and enhance exclusive breastfeeding practices, leading to improved maternal and child well-being in the region.
Keywords: Exclusive breastfeeding, Mothers, Knowledge, Attitudes, Pakistan
Introduction
Breastfeeding is an essential and effective method to ensure the health and survival of children, playing a significant role in their growth and development. As the best source of nourishment for infants and young children, breast milk profoundly impacts a child's survival, health, nutrition, and overall development [1-3]. Breast milk provides all the necessary nutrients, vitamins, and minerals required for an infant's body's growth and development. Additionally, it carries antibodies from the mother, helping to combat diseases and protect the child's health [3]. Shockingly, in 2010, approximately 7.6 million children died globally before reaching their fifth birthday, with 40% of these deaths occurring in the neonatal period. Pakistan, unfortunately, has one of the highest neonatal mortality rates worldwide [4].
Exclusive breastfeeding, as defined by the World Health Organization (WHO), means that the infant receives only breast milk, with no other liquids or solids given, not even water, except for oral rehydration solutions, vitamins, minerals, or medicines in drops/syrups [5]. The WHO recommends breastfeeding for a minimum of 2 years for all infants [6]. Surprisingly, if all infants were breastfed within an hour of birth, exclusively breastfed for the first 6 months, and continued breastfeeding up to the age of 2 years, about 220,000 child lives could be saved annually. However, less than 40% of infants under six months of age are exclusively breastfed worldwide. Increasing the promotion of EBF is one of the most efficient approaches to reducing infant morbidity and mortality globally [7].
Breastfeeding not only positively affects child health but also provides crucial protection to mothers. Extended lactation duration in postmenopausal women is associated with a lower prevalence of hypertension, diabetes, hyperlipidemia, and cardiovascular disease [8]. Following the WHO's recommendations on breastfeeding could save around 800,000 children's lives annually. Furthermore, infants who are exclusively breastfed are more likely to crawl and walk sooner than those who are not [9]. Studies also show that infants exclusively breastfed for 6 months experience less morbidity from gastrointestinal tract infections compared to those breastfed for less than 6 months [10]. Additionally, breastfed children have a decreased risk of post-neonatal death [11].
Despite the critical role of exclusive breastfeeding in child health and survival, there has been limited research conducted on this topic in Khyber Pukhtunkhwa (KP). This study aims to fill this knowledge gap and establish a baseline in KP regarding exclusive breastfeeding practices. Given the lack of awareness and knowledge about this essential practice, there is a pressing need for comprehensive studies to address the issue effectively in KP. By enhancing our understanding of exclusive breastfeeding and its benefits, the study will significantly contribute to raising awareness among mothers, healthcare providers, and the community at large. Moreover, the findings will serve as a valuable resource for developing targeted educational programs to promote exclusive breastfeeding. Through the dissemination of the study's results across both rural and urban areas, we can effectively advocate for and reinforce the significance of exclusive breastfeeding, ultimately leading to healthier babies and improved maternal well-being.
Objectives
- To find out about the knowledge of exclusive breastfeeding among mothers.
- To find the attitude and behavior of the mother towards it.
- To find attitudes towards the practice of exclusive breastfeeding.
- To know about misconceptions regarding breastfeeding.
- To find the reasons for not practicing exclusive breastfeeding.
Materials and Methods
The study was set in Charsada and utilized a cross-sectional study design. The target population comprised mothers, and a sample size of 100 participants was selected using a nonrandom, convenient sampling technique. A questionnaire was specifically designed to assess the knowledge, attitude, and practice of exclusive breastfeeding among the mothers, employing a random sampling approach. Inclusion criteria for participants included women who were currently breastfeeding their child or had a child less than 2 years old. The exclusion criteria consisted of mothers who expressed unwillingness to participate in the study and those facing language barriers.
For data collection, healthcare professionals working in the basic health unit conducted the study in Nahaki village, employing a standard questionnaire to interview the mothers. The questionnaire covered various aspects, including demographic information such as the mother's age, address, occupation, educational status, family income, exposure to information sources (TV, radio, newspaper, internet), as well as ethnic group affiliation. Additionally, questions were asked about the number and sex of the participants' children, breastfeeding practices, including the frequency of breastfeeding per day, the use of bottles, animal milk, and formula milk, and the sources of advice received. The practice of "ghutti" (traditional feeding) by the child was also assessed.
Furthermore, the mothers were questioned about their willingness and attitudes towards breastfeeding, as well as their perception regarding the importance of breastfeeding. Only information related to the most recent child in terms of breastfeeding practices was recorded. The study aimed to explore the association between knowledge, attitude, and practice of exclusive breastfeeding among mothers in the specified region.
Data obtained from the questionnaire will be analyzed using SPSS 16.0 to identify patterns, trends, and correlations related to exclusive breastfeeding. Descriptive statistics will be used to summarize demographic characteristics and key variables, while inferential statistics, such as chi-square tests and regression analysis, will be employed to assess relationships between variables. The significance level will be set at p < 0.05 to determine statistical significance. The findings will be presented using tables and charts to enhance clarity and facilitate a comprehensive understanding of the results.
Results
The study results are summarized in Table 1, which presents the baseline characteristics of the 100 included mothers. The mean age of the mothers was 29.11 years, with a standard deviation of 7.589. Among them, 55 mothers had male children, while 45 had female children. On average, each mother had 3.9 children, with a standard deviation of 2.213. In terms of education, 81 mothers had no formal education, 9 had education below the matric level, 2 had a matric education, 6 had completed FA/FSc, and 2 had education above FSc/FA. Furthermore, 43 mothers reported having access to social media. Regarding exclusive breastfeeding practices, 39 mothers were observed to be following the recommended guidelines (Table 1).
Table 1: Baseline characteristics of the included mothers.
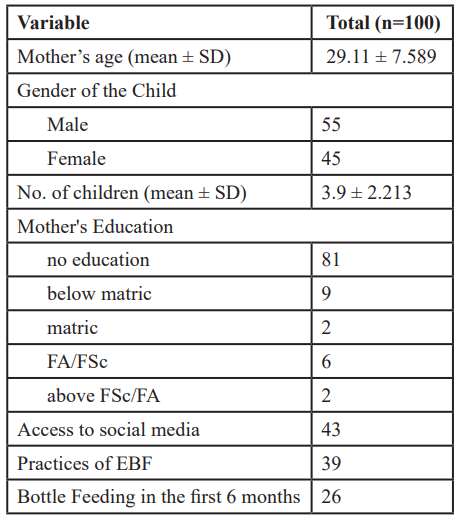
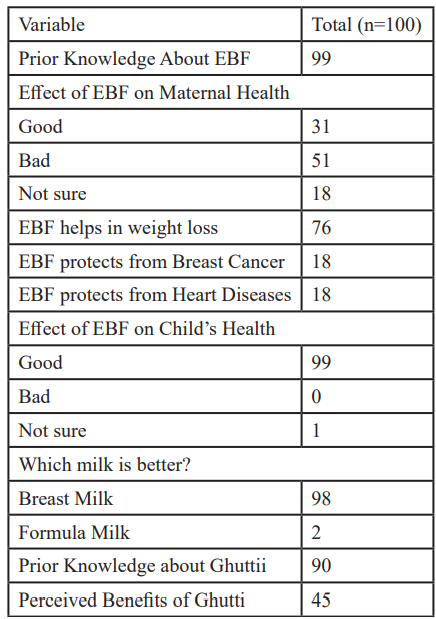
Table 2 reports maternal knowledge and perceptions of Exclusive Breastfeeding (EBF), and the results are presented in Table 2. Out of the 100 participants, 99 had prior knowledge about EBF, indicating a high awareness of the practice. Regarding its impact on maternal health, 31 participants viewed EBF positively, 51 held negative perceptions, and 18 were unsure. Moreover, 76 participants believed that EBF contributes to weight loss, but only 18 were aware of its potential for protecting against Breast Cancer and Heart disease. Turning to the child's health, an overwhelming majority of 99 participants acknowledged the positive influence of EBF, with only one participant expressing uncertainty, and none considering it to have adverse effects. Furthermore, the study revealed a strong preference for Breast Milk as the better choice of milk, as 98 participants opted for it, while only 2 chose Formula Milk.
Table 2: Maternal Knowledge and Perception About EBF.
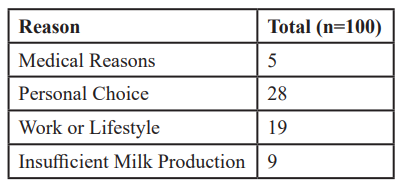
The study's results on bottle feeding are presented in Table 3, which includes data from 100 participants. The reasons for choosing bottle feeding over breastfeeding were categorized into four main factors. Medical reasons accounted for 5% of the participants' decisions, while 28% cited personal preference as their primary influencing factor. Work or lifestyle demands were mentioned by 19% of the respondents as the key reasons for opting for bottle feeding. Additionally, 9% reported insufficient milk production as a contributing factor to their decision.
Table 3: Reasons for Bottle Feeding.
Discussion
The present study aimed to explore the knowledge, attitudes, and practices of exclusive breastfeeding among mothers in Nahaki Charsada, Khyber Pukhtunkhwa (KP). Exclusive breastfeeding is crucial for the health and survival of infants, providing essential nutrients and protection against diseases [1,12]. A systematic review of exclusive breastfeeding practices in East Africa highlighted the challenges in maintaining exclusive breastfeeding, where the knowledge and attitude of mothers played significant roles [13]. Understanding mothers' knowledge and attitudes towards exclusive breastfeeding in Nahaki Charsada is essential, as it may have implications for breastfeeding practices in this region.
Inadequate knowledge about exclusive breastfeeding, its duration, and its perceived benefits may hinder mothers from exclusively breastfeeding infants for six months. This issue was evident in a study conducted in Noakhali, Bangladesh, which found that mothers' education level and socioeconomic status influenced their exclusive breastfeeding practices [14]. This aligns with earlier studies that reported similar findings [13-18]. In our study, we observed that 81% of mothers had no formal education, which might have impacted their understanding of exclusive breastfeeding practices. Addressing the educational disparity among mothers in Nahaki Charsada could be a key strategy for promoting exclusive breastfeeding.
Comparing findings from studies conducted in rural and urban settings can provide valuable insights. A study in Rajshahi, Bangladesh, found that exclusive breastfeeding practices were less prevalent in rural areas, similar to our observation in Nahaki Charsada [19]. Health education and counseling play pivotal roles in promoting exclusive breastfeeding practices. For example, a study in Masaka District Hospital, Kigali, Rwanda, showed that health education sessions were associated with improved exclusive breastfeeding rates among mothers [7]. Implementing similar health education initiatives in Nahaki Charsada could positively impact mothers' knowledge and attitudes towards exclusive breastfeeding, thereby promoting its practice.
Our study revealed that only 43 mothers reported having access to social media, which might limit their exposure to breastfeeding-related information. Utilizing various information sources, such as TV, radio, newspapers, and the Internet, can help disseminate knowledge about exclusive breastfeeding more effectively [13]. Efforts should be made to improve access to diverse information sources for mothers in Nahaki Charsada.
Based on the study findings, comprehensive interventions are needed to promote exclusive breastfeeding practices in Nahaki Charsada. These interventions should address maternal knowledge, attitudes, and misconceptions, consider socioeconomic factors, utilize community clinics, involve healthcare providers, and enhance access to information sources. Moreover, these findings can serve as a foundation for developing evidence-based policies to support and promote exclusive breastfeeding in the region.
Conclusion
In conclusion, this study provides valuable insights into the knowledge, attitudes, and practices of exclusive breastfeeding among mothers in Nahaki Charsada. The findings underscore the need for targeted educational programs and interventions to improve exclusive breastfeeding rates in the region. By drawing comparisons with studies conducted in other regions and leveraging evidence-based practices, we can develop effective strategies to promote exclusive breastfeeding, ultimately leading to healthier babies and improved maternal well-being.
References
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid ReportTechnology Assess, 2007; 153: 1–186.
- Sayres S, Visentin L. Breastfeeding: uncovering barriers and offering solutions. Curr Opin Pediatr, 2018; 30(4): 591–596.
- Hossain S, Mihrshahi S. Exclusive Breastfeeding and Childhood Morbidity: A Narrative Review. Int J Environ Res Public Health, 2022; 19(22): 14804.
- Determinants of exclusive breastfeeding practice in Bangladesh: Evidence from nationally representative survey data | PLOS ONE, 2023.
- Agho KE, Ezeh OK, Ghimire PR, Uchechukwu OL, Stevens GJ, Tannous WK, et al. Exclusive Breastfeeding Rates and Associated Factors in 13 “Economic Community of West African States” (ECOWAS) Countries. Nutrients, 2019; 11(12): 3007.
- Indicators for assessing infant and young child feeding practices: definitions and measurement methods, 2023.
- Infant feeding practices and maternal socio-demographic factors that influence practice of exclusive breastfeeding among mothers in Nnewi South-East Nigeria: a cross-sectional and analytical study | International Breastfeeding Journal, 2023.
- Schwarz EB, Ray RM, Stuebe AM, Allison MA, Ness RB, Freiberg MS, et al. Duration of lactation and risk factors for maternal cardiovascular disease. Obstet Gynecol, 2009; 113(5): 974–982.
- Breastfeeding, 2023.
- Optimal duration of exclusive breastfeeding – PMC, 2023.
- Chen A, Rogan WJ. Breastfeeding and the risk of postneonatal death in the United States. Pediatrics, 2004; 113(5): e435-439.
- Duijts L, Jaddoe VWV, Hofman A, Moll HA. Prolonged and Exclusive Breastfeeding Reduces the Risk of Infectious Diseases in Infancy. Pediatrics, 2010; 126(1): e18–25.
- Knowledge, attitude, and practice of exclusive breastfeeding among mothers in East Africa: a systematic review, 2023.
- Sultana M, Dhar S, Hasan T, Shill LC, Purba NH, Chowdhury AI, et al. Knowledge, attitudes, and predictors of exclusive breastfeeding practice among lactating mothers in Noakhali, Bangladesh. Heliyon, 2022; 8(10): e11069.
- Knowledge, attitude, and practice of exclusive breastfeeding among mothers in East Africa: a systematic review, 2023.
- Knowledge, attitude, and practice of exclusive breastfeeding among mothers in East Africa: a systematic review | International Breastfeeding Journal, 2023.
- Knowledge, attitudes and determinants of exclusive breastfeeding practice among Ghanaian rural lactating mothers | International Breastfeeding Journal, 2023.
- Vijayalakshmi P, Susheela T, Mythili D. Knowledge, attitudes, and breast-feeding practices of postnatal mothers: A cross sectional survey. Int J Health Sci, 2015; 9(4): 364–374.
- Knowledge and practices of exclusive breastfeeding among mothers in rural areas of Rajshahi district in Bangladesh: A community clinic based study | PLOS ONE, 2023.

