TAPB vs Spinal Analgesia in Gynecological Laparoscopy for Endometriosis Surgery
Agrati S1, Ambrosoli AL2,*, Stella M1, Crespi A2, Musella G2, Prof Severgnini P3
1Università degli Studi dell’Insubria, Varese, Italy
2Department of Anesthesia, Perioperative Medicine and Intensive Care Unit - F. Del Ponte Women and Children’s Hospital, ASST Sette Laghi, Varese, Italy
3Dip. Biotecnologie e Scienze della Vita, Università degli Studi dell’Insubria, Varese, Italy
Received Date: 14/02/2024; Published Date: 24/06/2024
*Corresponding author: Ambrosoli AL, Department of Anesthesia, Perioperative Medicine and Intensive Care Unit - F. Del Ponte Women and Children’s Hospital, ASST Sette Laghi, Varese, Italy
Abstract
Endometriosis, a chronic gynecological condition, presents significant medical and social burdens with unclear etiology and limited treatment options. Perioperative pain management in endometriosis surgery is crucial for patient well-being. This study compares Transversus Abdominis Plane Block (TAPB) and spinal analgesia in gynecological laparoscopy for endometriosis surgery. Twenty women underwent laparoscopy, divided into TAPB (n=10) and spinal analgesia (n=10) groups. Both techniques were effective in pain control without significant differences in hemodynamic parameters, rescue analgesic use, or complications. Spinal analgesia provided rapid pain relief but carried risks of hypotension and post-dural puncture headache, while TAPB offered simplicity, safety, and patient comfort. Despite the small sample size and single-center design, our findings support TAPB as a viable alternative to spinal analgesia for intraoperative pain management in endometriosis surgery. Further studies with larger, multicenter cohorts are needed to validate these results and broaden their applicability, providing a comprehensive understanding of TAPB’s role in optimizing perioperative pain management in endometriosis surgery.
Keywords: Transversus pain block (TAPB); Spinal analgesia; Endometriosis; Laparoscopy
Introduction
Endometriosis is a chronic and often debilitating gynecological condition characterized by the presence of endometrial-like tissue outside the uterus. This misplaced tissue can be found on pelvic organs such as the ovaries, fallopian tubes, the lining of pelvis and rarely even in the torax; it triggers a chronic inflammatory reaction causing formation of adhesion between separate organs and structures. Endometriosis is associated with symptoms such as pelvic pain, painful menstruation, and infertility [1]. The medical and social impact of the disease is high, and it is estimated that between 2% up to 10% of the women general population suffer of it. Unfortunately, the exact causes of it remains unclear, even if there are several theories such as the retrograde menstruation [2], and effective treatment options are limited. Managing endometriosis typically involves a combination of medical therapies, surgical interventions, and pain management strategies aimed at alleviating symptoms and improving patients' overall well-being. Nowadays, when the surgical treatment is needed to eliminate peritoneal endometriosis, endometrioma and divide adhesion, laparoscopy is preferred because it relates to less surgical pain, faster discharge and recovery [3]. In this context, it becomes crucial for anesthesiologists to ensure optimal intra and postoperative pain control. Two commonly techniques have emerged as potential strategies to alleviate postoperative discomfort and enhance recovery: Transversus Abdominis Plane Block (TAPB) [4,5] and spinal analgesia [6]. However, the comparative efficacy and safety profiles of these approaches remain areas of active investigation in a population in which pain plays a a central role.
The aims of our study are to provide a comprehensive analysis of the advantages and limitations associated with TAPB and spinal analgesia in gynecological laparoscopy for endometriosis surgery, shedding light on their respective roles in optimizing perioperative pain management and patient outcomes.
Materials and Methods
Study population and study design
We then conducted an observational retrospective study involving 20 women who were treated for endometriosis with laparoscopy in our department in 2023; we divided them into two groups: TAPB group (n.10 patients) and spinal analgesia group (n.10 patients). Inclusion criteria were ASA class I and age >18 years. All the patients underwent general anesthesia (GA) with induction with propofol (1.5-2 mg/kg), fentanyl (1 mcg/kg) and maintenance with sevoflurane (MAC 0,8). In the TAPB group the block was performed before the beginning of the surgery with levobupivacaine 0,375% 20 mL for each side, with needle insertion using an in-plane US-technique. In the analgesic spinal injection group, spinal puncture was performed prior to GA, using Sprotte atraumatic needle 25G with levobupivacaine 0,1% 3 mL plus morphine 100 mcg. In both groups we administered ketorolac 30 mg iv, acetaminophen 1g iv and ondansetron 4 mg iv immediately before the end of the intervention. Sistoic blood pressure (SBP), heart rate (HR), pulse oxymeter saturation (SpO2), capnographic curve, endtidal CO2 value were monitored throughout the procedure. We assessed hemodynamic parameters and SpO2 at the end of the surgery, during the first 24 hours and 48 hours of recovery; pain using NRS scale post-surgery, at 6-12-24-48 hours postoperative; the frequency of rescue analgesic medication (morphine 10mg x 3 iv) during the first 24 hours after surgery; postoperative nausea and vomit (PONV) at the end of surgery and during the first 24 Hours; length of postoperative hospital stays. Other recorded variables were age, Body Mass Index (BMI), basal SBP, basal HR and basal SpO2.
Statistical analysis
We analyzed datas calculating mean values and standard deviations of age, BMI, SBP, HR, SpO2 and length of stay of both groups. We perform a t-Student test to verify if there was a statistically significant difference between groups, setting alpha of 0.05.
All the data are reported in Table 1.
Table 1: Studied variables and statistical analysis.
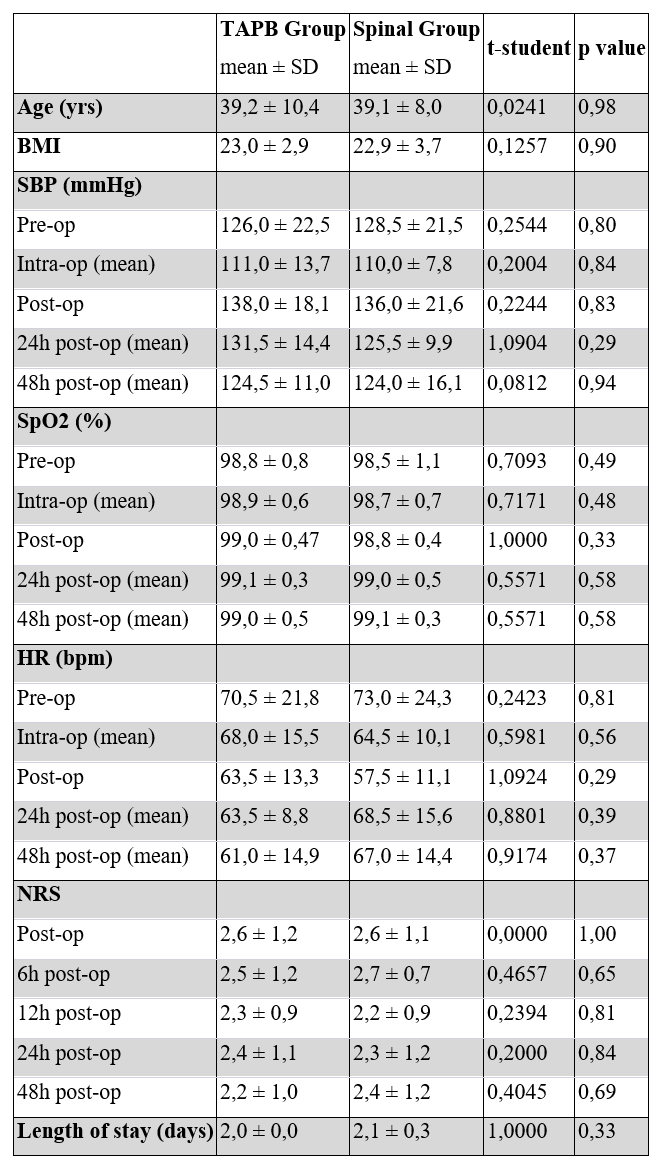
We obtained all p-values greater than the fixed alpha of 0.05 (using the t-distribution table): the difference observed between the means of the parameters analyzed in TAPB group and antalgica spinal group is then not statistically significant.
In both groups 20% of women asked for rescue morphine because of pain NRS ≥4. No PONV and other complications were reported in both groups.
Discussion
Spinal analgesia is a commonly used regional anesthesia technique for pain control during and after abdominal and pelvic surgeries. It involves the injection of local anesthetic into the subarachnoid space providing rapid and effective pain relief, allowing patients to recover more quickly and reducing perioperative opioid use [7].
However, spinal analgesia may have some complications, including hypotension, post-dural puncture headache, and nerve injury [8]. The tap block, on the other hand, is more recent regional anesthesia technique involving the injection of local anesthetic around peripheral nerves to block pain transmission. It is particularly effective in controlling post-operative pain after abdominal surgery [9]. For sure TAPB guarantees less complications and offers several advantages over spinal analgesia, it does not require assessment of the patient’s coagulation status and platlets number [10] and can be performed after the induction of general anesthesia, creating less discomfort for patients compared to spinal analgesia, which requires the patient to be awake. Additionally, it can be safely performed even by less experienced anesthesiologists, as it has a very rapid learning curve thanks to the guance of ultra-sound [11]. In conclusion, while both spinal analgesia and tap block are effective in controlling post-operative pain, tap block offers advantages in terms of lower risks of complications, ease of execution, and reduced patient discomfort, making it a preferred choice in many clinical settings.
Based on the results of our study, we can affirm that TAPB is not inferior to spinal analgesia in terms of postoperative pain and perioperative parameter variations. However, the major limitations of our study are that it was conducted at a single center involving a small number of patients, all of whom were ASA I; thus, it cannot be generalized to all the women undergoing laparoscopic surgery for the treatment of endometriosis.
Conclusion
Based on our study findings, we suggest performing TAPB for intraoperative pain control. It is a valid alternative to spinal analgesia without the risks of central nervous system block. Have a safe, quick and easy way to control the pain during and after surgery should be the one of the anesthesiology goals in the ERAS prospective, and it could be particularly challenging in women with endometriosis, who are usually more susceptible to severe pain.
However, it is necessary to expand the study to a larger sample size involving multiple centers for more comprehensive results. In this way we could enhance the generalizability and robustness of the results, providing a clearer understanding of the efficacy and safety profile of TAPB in the management perioperative pain in endometriosis surgery.
Author Contributions: Andrea Luigi Ambrosoli and Silvia Agrati planned the presented study. Andrea Ambrosoli supervised the work. Silvia Agrati contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript and performed the statistical analysis. All authors discussed the results and contributed to the final manuscript.
Conflict of interest and Grant information: All the authors declare no conflict of interests. The authors received no specific funding for this work.
References
- Christian M Becker, Attila Bokor, Oskari Heikinheimo, Andrew Horne, Femke Jansen, Ludwig Kiesel, et al. ESHRE guideline: endometriosis, Human Reproduction Open, 2022; 2022(2).
- Bulun Serdar E. Endometriosis caused by retrograde menstruation: now demonstrated by DNA evidence. Fertility and Sterility, 2023; 118(3): 535–536.
- Bafort C, Beebeejaun Y, Tomassetti C, Bosteels J, Duffy JMN. Laparoscopic surgery for endometriosis. Cochrane Database of Systematic Reviews, 2020; 10.
- Oostvogels L, Weibel S, Meißner M, Kranke P, Meyer-Frießem CH, Pogatzki-Zahn E, et al. Erector spinae plane block for postoperative pain. Cochrane Database of Systematic Reviews, 2024; 2.
- Alessandri F, Lijoi D, Mistrangelo E, Nicoletti A, Ragni N. Effect of presurgical local infiltration of levobupivacaine in the surgical field on postsurgical wound pain in laparoscopic gynecological surgery. Acta Obstet Gynecol Scand, 2006; 85: 844-849.
- Pirie K, Doane MA, Riedel B, Myles PS. Analgesia for major laparoscopic abdominal surgery: a randomised feasibility trial using intrathecal morphine. Anaesthesia, 2022; 77: 428-437.
- Kukreja P, Streetzel C, Short RT, Mabry SE, Feinstein J, Brazeel K, et al. Intrathecal Morphine Use Improves Postoperative Analgesia and Reduces Opioid Consumption in Patients Undergoing Total Knee Arthroplasty Under Spinal Anesthesia: A Retrospective Study. Cureus, 2023; 15(8): e43039.
- Olawin AM, M Das J. Spinal Anesthesia. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2024.
- Elsharkawy H, Bendtsen TF. Ultrasound-Guided Transversus Abdominis Plane and Quadratus Lumborum Blocks. In: Hadzic A. eds. Hadzic's Textbook of Regional Anesthesia and Acute Pain Management, 2e. McGraw-Hill Education, 2017.
- Van Veen JJ, Nokes TJ, Makris M. The risk of spinal haematoma following neuraxial anaesthesia or lumbar puncture in thrombocytopenic individuals. British Journal of Haematology, 2010; 148: 15-25.
- Vial F, Mory S, Guerci P, Grandjean B, Petry L, Perrein A, et al. Évaluation de la courbe d'apprentissage du bloc du plan transverse abdominal: étude prospective observationnelle [Evaluating the learning curve for the transversus abdominal plane block: a prospective observational study]. Can J Anaesth, 2015; 62(6): 627-633.

