A Study on Ectopic Pregnancy – Incidence, Risk Factors and Outcome at a Tertiary Care Centre
Adlin Ho1,* and Amreen Sharif2
1Study from the Department of Obstetrics and Gynecology, Hyderabad, Telangana, India
2Senior Resident in Department of Obstetrics and Gynecology, India
Received Date: 24/01/2024; Published Date: 10/06/2024
*Corresponding author: Dr. Adlin Ho, Study from the Department of Obstetrics and Gynecology, Hyderabad, Telangana, India
ORCHID ID: 0000-0002-7051-3050
Abstract
Introduction: Ectopic pregnancy is a diagnostic dilemma with drastic consequences. A thorough updated knowledge of incidence and risk factors is essential for early diagnosis and better management of ectopic pregnancy.
Methods: A retrospective observational study was conducted at a tertiary care hospital from July 2023 to November 2023. The incidence and risk factors associated with ectopic pregnancy were studied.
Results: The incidence of ectopic was 32/421 number of deliveries. In the given study population 31.25% had ruptured ectopic and 68.76% had unruptured ectopic. Majority of ectopic pregnancy occurred in the age group of 21-25 years. Among risk factors, history of PID (15.63%), history of ectopic (15.63%) and history of infertility (12.5%) were major contributors.
Conclusion: Patients with risk factors should be viewed with a high index of suspicion. Early diagnosis with ultrasound and clinical examination can prevent maternal mortality and morbidity.
Keywords: Ectopic pregnancy; Risk Factors; PID; Infertility; Unruptured ectopic
Introduction
Ectopic pregnancy is a life-threatening obstetric emergency quite often missed on diagnosis in young women. It is essential to be ectopic minded in the diagnosis of ectopic pregnancy. The incidence of ectopic pregnancies has increased due to early detection by ultrasound and making first trimester ultrasound as part of routine antenatal work up.
Extensive investigation of patients with risk factors like pelvic inflammatory disease, past history of ectopic and infertility in women between ages 15-44 years are quintessential for early diagnosis of ectopic [1].
Ectopic pregnancy may be responsible for nearly 5% of maternal deaths in developing countries compared with <1% in developed countries [2].
According to Mayo clinic 2020 guidelines, some conditions which make it more likely to have an ectopic pregnancy are: previous ectopic pregnancy, inflammation of infection, fertility treatments, tubal surgery, choice of birth control and smoking [3].
Incidence of ectopic pregnancy is around 1-2% in most hospital-based studies, 10 times higher in developing countries than those in developed countries [4].
Present study improves our understanding on risk factors and presentation of ectopic pregnancy. This further helps to identify critical areas in early diagnosis and management of ectopic pregnancy and prevention of maternal mortality.
Methods and Methodology
A retrospective observational study was conducted at a tertiary care hospital in Hyderabad from July 2023 to November 2023. Data regarding presentation, clinical features, risk factors, and outcome of ectopic pregnancy was studied from case records of patients. All data was entered and analysed using Microsoft Excel.
Inclusion criteria – All clinically diagnosed or scan diagnosed patients with ectopic pregnancy who were admitted and underwent laparoscopic surgery for ectopic pregnancy at this tertiary care centre from July 2023 to November 2023.
Exclusion criteria: Nil
Results
The incidence of ectopic gestation in the present study was 32/421 no.of deliveries in study period. The data was collected retrospectively from old case records of patients. All data was tabulated and analysed by using Microsoft Excel.
The given study data is represented in percentages. Out of the given 32 cases, 31.25% had ruptured ectopic and 68.76% had unruptured ectopic pregnancy. The distribution among parity was 31.25% multigravida and 68.76% were primigravidas.
Incidence of ectopic pregnancy was maximum in the age group of 21-25 years that is 46.88%, below 20 years was 18.75% , above 30 years was 15.63% and between 26-30 years was 18.75%.
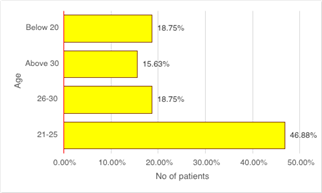
Figure 1: Age distribution graph among the study population.
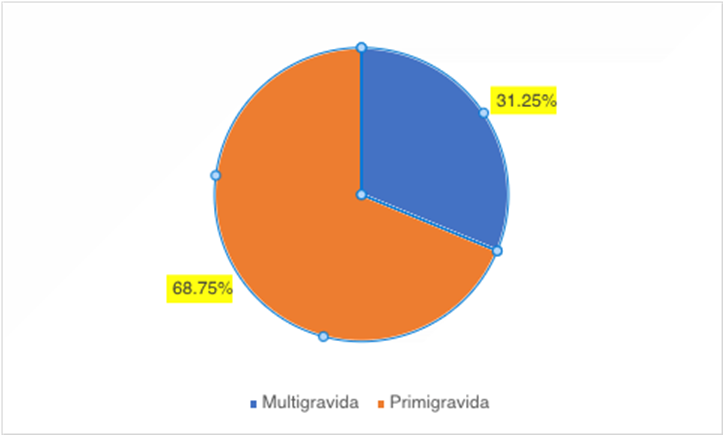
Figure 2: Percentage distribution of parity in study population.
There were 68.76% primigravidas and 31.25% multigravidas among the study population. Among the given study group 59.38% had normal examination findings, 12.5% had left forniceal fullness, 12.5% had left forniceal tenderness, right forniceal fullness was seen in 9.38% and right forniceal tenderness was seen in 6.25%.
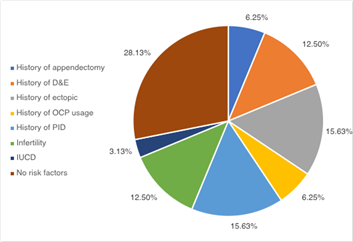
Figure 3: The distribution of the study population according to risk factors.
Among the risk factors of the ectopic in the given study, history of Pelvic inflammatory disease was seen in 15.63% and history of ectopic pregnancy was seen in 15.63%. There were no risk factors in 28.13% of the cases and there was history of dilatation and evacuation in 12.5% of cases and history of infertility in 12.5% of cases.History of appendectomy was seen 6.25% and history of use of Oral Contraceptive pill was seen in 6.25% of cases and history of IUCD usage was seen in 3.13% of the cases.
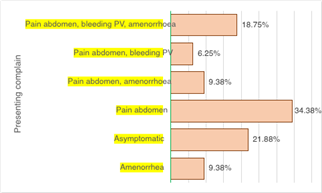
Figure 4: Distribution of symptomatology among study population.
According to symptomatology only 18.75% had classical triad of pain abdomen, bleeding PV and amenorrhea, whereas 34.38% of the patients had pain abdomen. Pain abdomen and bleeding PV was seen in 6.25% and pain abdomen and amenorrhea was seen in 9.38%, amenorrhea was seen in 9.38% and 21.88% were asymptomatic.
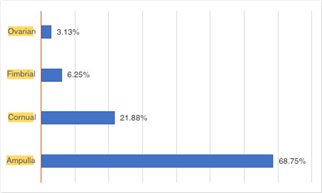
Figure 5: Site of ectopic among study population.
Majority of patients had an ampullary ectopic that is 68.75%. Cornual ectopic was seen in 21.88%, Fimbrial ectopic was seen in 6.25% and ovarian ectopic was seen in 3.13%.
Discussion
Incidence of ectopic in present study was 32/421 no of deliveries, whereas in the study conducted by Shanti et al, the incidence of ectopic was 1 in 380 deliveries.
According to present study incidence of ectopic was 48.66% between the age groups 21-25 years as comparable to other studies. According to Shanti et al [5], the study population distribution was 72% between age 20-30 years. As reported by Neelima et al [6], there were 40.3% patients between the age group of 26-30 years and according to Pranati et al [7] 57.14% belonged to the age group 21-30 years.
Among the risk factors for ectopic pregnancy, history of PID was seen in 15.63% of the patients. According to Shanti et al [5], history of PID was noted in 25.8% of cases and according to Neelima et el [6] 19.4% had history of PID. According to Pranati et el [7], the history of PID was seen at 14.28%. The higher incidence in the study conducted by Shanti et al was probably due to selection bias.
History of infertility was seen in 12.5% of cases. According to a study conducted by Shanti et al [5], history of infertility was seen in 4.83% of the cases and according to Pranati et al [7] history of infertility was noted in 7% of the patients. The higher incidence of infertility in present study could be due to increased awareness among patients and anxiousness to conceive and hence the use of treatment modalities for infertility.
In the present study, the previous history of ectopic pregnancy was seen in 15.63% of the patients. According to Pranati et al [7], the previous history of ectopic pregnancy was seen in 1% of cases. As reported by Neelima et al [6], history of ectopic was seen in 14 % of the cases and according to Shanti et al [5] history of ectopic was 6.45% in her study.
The classical triad of pain abdomen, bleeding PV and amenorrhea was seen in 18.75% of the cases.
According to Pranati et al [7] this classical triad was reported in 40.7% of cases and according to Shanti et al the pain abdomen was seen in 80.2% of cases and amenorrhea was seen in 70% of the cases.
Ruptured ectopic was seen in 31.25% of the cases where unruptured ectopic was seen in 68.76% of the cases. According to Shanti et al [5], ruptured ectopic was seen in 82.3% of cases, according to Pranati et al [7] incidence of ruptured ectopic was 83.33%. This could be explained by high clinical suspicion of ectopic based on history and risk factors and early detection of ectopic pregnancy by ultrasound.
In our present study, ampullary ectopic was seen in 68.75% and Cornual ectopic was seen in 21.88% of the cases which was comparable to data from other studies. Tubal ectopic was seen in 97% of cases according to Pranati et al, according to Neelima et al ampullary ectopic was seen 54.8% of the cases and according to Shanti et al tubal ectopic was seen in 54.8% of the cases.
Conclusion
Ectopic pregnancy is a diagnostic dilemma. High index of suspicion on part of the physician for diagnosis of ectopic is advisable. The analysis of risk factors for ectopic pregnancy reveals that history of ectopics in previous pregnancy, history of PID and history of infertility should be viewed with a high index of suspicion. Pre pregnancy work up and planning the conception may be useful. The mortality rate for tubal ectopic pregnancy was reported at 0.14% whilst that for interstitial pregnancy was reported to be nearly 15 times higher at 2-2.5% [8]. Early confirmation of intrauterine gestation in these cases may help reduce mortality and morbidity associated with ectopic in such cases. Further this study also highlights that there were no risk factors in 28.13% of the cases, warranting the need for further studies regarding other etiological factors.
Authorship Criteria:
Dr. Adlin Ho (Guarantor)- Concept and Design of Study, acquisition and analysis of data, drafting the article.
Dr. Amreen Sharif- Final approval of the version to be published.
Conflict of Interest: None
Grant Information: The authors received no specific funding for this work.
References
- Andola S, Kumar RR, Desai RM, Krutika SA. Study of Risk factors and treatment modalities of ectopic pregnancy. J Family Med Prim Care, 2021; 10: 724-729.
- Rose Mcgready, Glen D Liddell Mola, Marcus AJ Rijken, François H Nosten, Theonest Mutabingwa. Obstetrics in the Tropics, Manson's Tropical Infectious Diseases (Twenty-third Edition), W.B. Saunders, 2014; Pages 1177-1196.
- Ectopic Pregnancy. Mayo clinic: diagnosis and management, 2020.
- Yeasmin MS, Uddin MJ, Hasan E. A clinical study of ectopic pregnancies in a tertiary care hospital of Chittagong, Bangladesh, Chattagram Maa-O-Shrishu Hospital Med Coll J, 2014; 13: 1-4.
- Asuri SS, Kalpana P. A clinical study of ectopic pregnancy. Int J Reprod Contracept Obstet Gynecol, 2016; 5: 3750-3753
- NeelimaB, VanamalaVG. Risk factors of ectopic pregnancy: a study in a tertiary care centre. Int J Reprod Contracept Obstet Gynecol, 2017; 6: 2858-2861.
- Pranati L, Madhavi Y. A clinical analysis of ectopic pregnancies in a tertiary care hospital in Hyderabad, Asia PAC J, Health SCI, 2018; 5(1): 20-24.
- Jurkovic D, Mavrelos D. Catch me if you scan: ultrasound diagnosis of ectopic pregnancy. Ultrasound Obstet Gynecol, 2007; 30: 1-7.

