Analysis of Telehealth Coverage Amongst Maxillofacial Emergency Services during the COVID-19 Pandemic: A Comparison of Three Academic Institutions
Briana J Burris, Atijah J Collins, Jettie Uyanne, Diana Messadi, Anh D Le, and Colonya C Calhoun Burns*
Division of Oral & Maxillofacial Surgery and Dentistry, Oral and Maxillofacial Surgery, Harbor – UCLA Medical Center Lecturer, UCLA School of Dentistry, USA
Received Date: 20/12/2023; Published Date: 02/05/2024
*Corresponding author: Colonya C Calhoun, Program Director, Division of Oral & Maxillofacial Surgery and Dentistry, Oral and Maxillofacial Surgery, Harbor – UCLA Medical Center Lecturer, UCLA School of Dentistry, USA
Abstract
Aims of Study: The coronavirus disease 2019 (COVID-19) pandemic has required a shift in healthcare delivery platforms, necessitating a new dependence on telehealth. This study evaluates the use of telehealth in dental specialty services during the COVID-19 pandemic and assesses insurance reimbursement rates of services for both telemedicine and tele dentistry codes.
Materials and Methods: We conducted a study to determine the percentage of telehealth usage during the COVID-19 pandemic and the cost of reimbursement based on telemedicine and teledentistry codes. Three major clinical centers, Harbor-UCLA Medical Center, UCLA School of Dentistry, and Hospital of the University of Pennsylvania (HUP), participated in this study. Teledentistry codes, established by the American Dental Association (ADA), include: D9999, Unspecified adjunctive procedure; D9995, Teledentistry-Synchronous; D9996, Teledentistry-Asynchronous. Telemedicine codes established by the Center for Medicare and Medicaid Services (CMS) include management during COVID-19, 3599, and 99213, with modifier GT.
Results: During the COVID pandemic, the percentage of telehealth visits increased across all oral healthcare services, in particular during the early months of shutdowns. From the dental specialty services, OMFS, Oral Medicine (OM), and Hospital Dentistry, 44-78% of all visits at HUP and Harbor-UCLA were telemedicine visits. UCLA School of Dentistry was able to provide teledentistry in Oral Medicine, Orofacial Pain, Pediatric Dentistry and Orthodontics specialty clinics, at 30-50% of total visits.
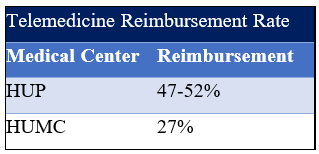
There was a discrepancy in reimbursement for oral health service coverage via telemedicine and teledentistry. At the medical center, depending on the payor-mix, more commercial insurers have stepped up to cover telehealth service at the same rate as in-office visit. Telemedicine reimbursement for OMFS and OM services at the medical centers averages 47-52% depending on the patient insurance carriers. At UCLA School of Dentistry, teledentistry reimbursement averaged $21 by DentiCal, $34 by Delta Dental, and $43-73 by Medicare, a 50% reduction of in- person encounter visits.
Conclusion: Teledentistry reimbursement for oral health service has not reached the same coverage level as in-person encounters, rendering telehealth access in the dental setting challenging. Professional and dental associations, patient and consumer advocacy groups should advocate for better coverage and extension of telehealth benefits to improve oral health access during pandemic.
Introduction
Teledentistry, a concept championed since the early 1990s, has long been recognized as a key tool in improving access to oral healthcare. The COVID-19 pandemic prompted a resurgence in the utilization of tele dentistry, driven by the need to minimize face-to-face interactions and efficiently triage cases to determine the necessity of emergency dental treatment. Despite initial hopes for the pandemic's resolution, the recent surge in the Delta variant of the virus and ongoing vaccine hesitancy suggest that the end may not be imminent. The World Health Organization (WHO) expresses concerns that COVID-19 may transform into an endemic virus, persisting in pockets of the global population.
In light of this prolonged uncertainty, it becomes imperative for dental healthcare providers to integrate tele dentistry into their practices, strategically limiting face-to-face visits when indicated. A review paper published in 2013 in the Journal of Telemedicine and e-Health underscored the extensive applications of tele dentistry in preventive, orthodontic, endodontic, oral surgery, periodontal conditions, early caries detection, patient education, oral medicine, and diagnosis, among others. These applications aim to enhance efficiency, widen access to underserved populations, improve the quality of care, and concurrently reduce the burden of oral diseases.
However, the incorporation of tele dentistry is not without its challenges. Pitfalls include risk management, disparities in internet access and speed, HIPAA compliance, Electronic Medical Record (EMR) integration, and the persistent issue of reimbursement. Early in the pandemic, California sought a government waiver to cover Medicaid recipients and expand telehealth options. Consequently, Medicare demonstrated flexibility in telehealth and virtual communications to facilitate healthcare delivery in individuals' homes.
The provided flexibility allowed for telehealth and virtual/telephonic communications for various covered State plan benefits, including behavioral health treatment services. It also waived face-to-face encounter requirements for Federally Qualified Health Centers (FQHCs), Rural Health Clinics (RHCs), and Tribal 638 Clinics relative to covered services via telehealth. Moreover, reimbursement for virtual communication and e-consults for FQHCs, RHCs, and Tribal 638 clinics was permitted, along with the waiver of limitations around virtual/telephonic communications before or after an in-office visit.
In this evolving landscape, health plans were mandated to reimburse providers at the same rate for services delivered via telehealth as for in-person services, provided the nature of the service remained consistent. The COVID-19 pandemic, therefore, serves as a catalyst for a paradigm shift in healthcare delivery, pushing providers to embrace innovative solutions, especially within the domain of teledentistry. This paper aims to analyze the telehealth coverage for oral health services during the pandemic, with a specific focus on the experiences of an academic public hospital. Understanding the complexities of this transition is paramount for shaping the future of oral healthcare delivery.
Materials and Methods
We conducted a study to assess telehealth utilization and cost reimbursement during the COVID-19 pandemic, focusing on telemedicine and teledentistry codes. Three prominent clinical centers—maxillofacial emergency services at Harbor-UCLA Medical Center, UCLA School of Dentistry, and the Hospital of the University of Pennsylvania (HUP)—participated in this research endeavor. The study specifically examined the application of teledentistry codes, as defined by the American Dental Association (ADA), which comprise D9999 for Unspecified Adjunctive Procedure, D9995 for Teledentistry-Synchronous, and D9996 for Teledentistry- Asynchronous. Additionally, telemedicine codes established by the Center for Medicare and Medicaid Services (CMS) were considered, including 3599 and 99213 for management during COVID-19, both designated with modifier GT.
Results
During the COVID pandemic, the percentage of telehealth visits increased across all oral healthcare services, in particular during the early months of shutdowns. From the dental specialty services, OMFS, Oral Medicine (OM), and Hospital Dentistry, 44-78% of all visits at HUP and Harbor-UCLA were telemedicine visits. UCLA School of Dentistry was able to provide teledentistry in Oral Medicine, Orofacial Pain, Pediatric Dentistry and Orthodontics specialty clinics, at 30-50% of total visits (not shown on graph).
In comparing maxillofacial emergency consult service, otolaryngology utilized telehealth upto five times more that both dental/OMS and plastics combined at HUMC while dental/OMS and otolaryngology both utilized telehealth more often than plastics. All services had a dip in utilization during the month of September 2020.
There was a discrepancy in reimbursement for oral health service coverage via telemedicine and teledentistry. At the medical center, depending on the payor-mix (If you have a higher % of Medical then the #’s may be lower. Demographics is different), more commercial insurers have stepped up to cover telehealth service at the same rate as in-office visit. Telemedicine reimbursement for OMFS and OM services at the medical centers averages 47-52% depending on the patient insurance carriers. At UCLA School of Dentistry, tele dentistry reimbursement averaged $21 by DentiCal, $34 by Delta Dental, and $43-73 by Medicare, a 50% reduction of in- person encounter visits.
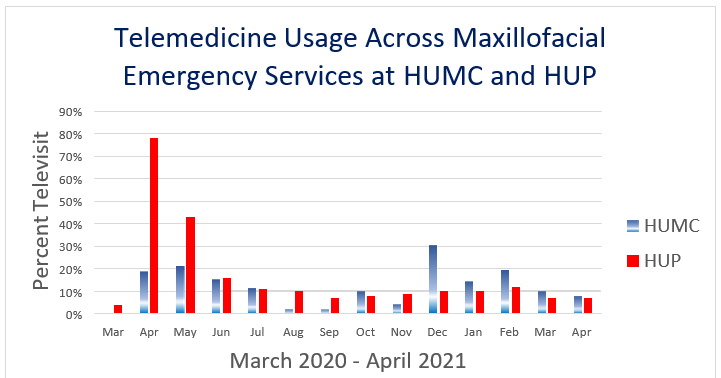
Figure 1: Telemedicine Usage Across Maxillofacial Emergency Services at HUMC and HUP.
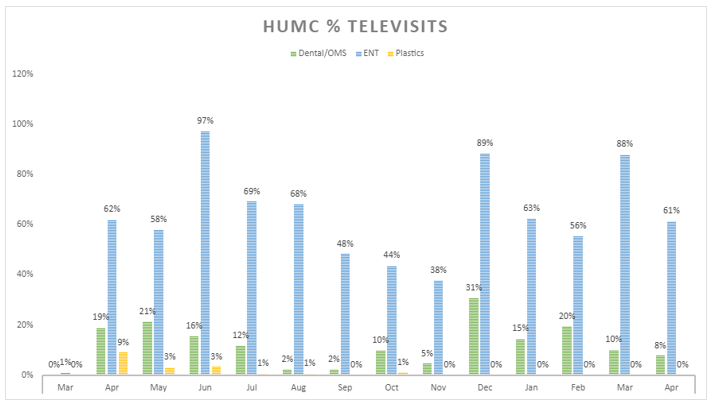
Figure 2: Telemedicine Usage Dental/OMS, ENT and Plastics at HUMC.
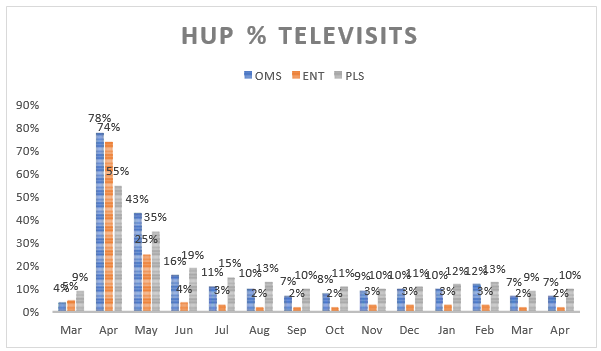
Figure 3: Telemedicine Usage Dental/OMS, ENT and Plastics at HUP.
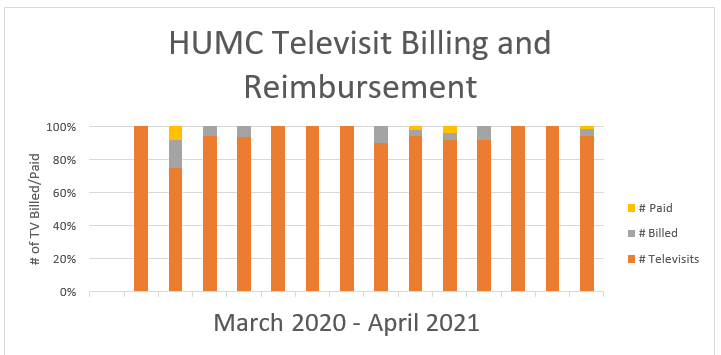
Figure 4: HUMC Televisit Billing and Reimbursement.
Table 1: UCLA SOD Teledentistry Reimbursement for the three major payor sources.
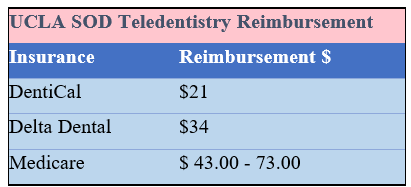
Table 2: Telemedicine Reimbursement Rate.
Discussion
Some of the pitfalls would include risk management, internet access/speed, HIPPA, EMR integration and lack of reimbursement. At the beginning of the pandemic, California requested a government waiver to cover medical recipients and expand telehealth options.
Health plans shall reimburse providers at the same rate, whether a service is provided in-person or through telehealth, if the service is the same regardless of the modality of delivery, as determined by the provider’s description of the service on the claim. For example, if a health plan reimburses a mental health provider $100 for a 50-minute therapy session conducted in-person, the health plan shall reimburse the provider $100 for a 50-minute therapy session done via telehealth.2
Health plans shall provide the same amount of reimbursement for a service rendered via telephone as they would if the service is rendered via video, provided the modality by which the service is rendered (telephone versus video) is medically appropriate for the enrollee.
The COVID-19 pandemic has spurred a transformative shift in healthcare delivery, necessitating the rapid adoption of telehealth across various medical specialties. This research specifically delves into the realm of dental specialty services, evaluating the utilization of telehealth and examining the corresponding insurance reimbursement rates during the pandemic. The findings shed light on the evolving landscape of teledentistry, presenting both opportunities and challenges for oral healthcare providers.
Increased Telehealth Utilization: The study reveals a notable surge in telehealth visits across all oral healthcare services, especially in the early months of the pandemic-induced shutdowns. The dental specialty services, including Oral and Maxillofacial Surgery (OMFS),
Oral Medicine (OM), and Hospital Dentistry, exhibited substantial proportions of telemedicine visits, ranging from 44-78% at Harbor-UCLA and the Hospital of the University of Pennsylvania (HUP). UCLA School of Dentistry also demonstrated significant utilization of teledentistry in various specialty clinics, accounting for 30-50% of total visits. This uptick in telehealth adoption highlights the adaptability of oral healthcare services to leverage technology for patient care.
Discrepancy in Reimbursement Rates: While telehealth usage increased, the study identifies a significant gap in reimbursement rates for oral health services delivered through telemedicine and teledentistry. The data indicates that commercial insurers at the medical centers, such as HUP and Harbor-UCLA, have shown a willingness to cover telehealth services at rates comparable to in-office visits. However, disparities exist, with reimbursement rates ranging from 47-52% for OMFS and OM services, depending on patient insurance carriers. UCLA School of Dentistry's teledentistry reimbursement rates further underscore the variability, with DentiCal reimbursing $21, Delta Dental at $34, and Medicare ranging from $43-73. This discrepancy in reimbursement poses a substantial challenge to the widespread adoption and sustainability of teledentistry.
Challenges and Advocacy for Improved Coverage: The study's findings point to the critical issue of teledentistry reimbursement lagging behind in-person encounters, presenting a hurdle to the seamless integration of telehealth into oral healthcare practices. To address this challenge, the conclusion recommends collaborative efforts from professional and dental associations, patient advocacy groups, and consumer advocates to advocate for better coverage and an extension of telehealth benefits. Such advocacy is crucial for ensuring equitable access to oral healthcare, especially during a prolonged public health crisis like the COVID-19 pandemic.
Tele dentistry’s Role in the Future of Oral Healthcare: In the broader context, the discussion emphasizes the importance of teledentistry as a strategic tool for improving access to oral healthcare services. The COVID-19 pandemic serves as a catalyst for a paradigm shift in healthcare delivery, pushing providers to embrace innovative solutions.
Despite the challenges associated with risk management, internet disparities, HIPAA compliance, and reimbursement issues, the study underscores the need for continued efforts to integrate teledentistry into routine practice. The discussion suggests that understanding the complexities of this transition is crucial for shaping the future of oral healthcare delivery, particularly in a landscape where the persistence of COVID-19 as an endemic virus remains a concern.
In conclusion, this research contributes valuable insights into the dynamics of telehealth adoption in dental specialty services during the COVID-19 pandemic. The findings highlight both the potential benefits and the existing challenges, with a call to action for collaborative advocacy to improve telehealth reimbursement and enhance access to oral healthcare.
Key Takeaways: Effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to patients in broader circumstances.
These visits are considered the same as in-person visits and are paid at the same rate as regular, in-person visits.
Starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for professional services furnished to beneficiaries in all areas of the country in all settings.
While they must generally travel to or be located in certain types of originating sites such as a physician’s office, skilled nursing facility or hospital for the visit, effective for services starting March 6, 2020 and for the duration of the COVID-19 Public Health Emergency, Medicare will make payment for Medicare telehealth services furnished to beneficiaries in any healthcare facility and in their home.
The Medicare coinsurance and deductible would generally apply to these services. However, the HHS Office of Inspector General (OIG) is providing flexibility for healthcare providers to reduce or waive cost-sharing for telehealth visits paid by federal healthcare programs.
To the extent the 1135 waiver requires an established relationship, HHS will not conduct audits to ensure that such a prior relationship existed for claims submitted during this public health emergency.
DDS vs. MD reimburse at lower rate for ICD-9 codes

