OTS as a Prognostic Tool in Open Globe Injuries for the assessment of Final Visual Acuity
Chaudhry Nasir Ahmad*, Maria Khalid, Salman Hamza, Raza Ali Shah, Abdul Basit and Irfan Muslim
Department of opthalmology, Kind Edward medical college and allied hospitals, Pakistan
Received Date: 26/10/2023; Published Date: 04/12/2023
*Corresponding author: Chaudhry Nasir Ahmad, Department of opthalmology, Kind Edward medical college and allied hospitals, Pakistan
Abstract
Rationale: The objective of this study is to evaluate the significance of ocular trauma score (OTS) in estimating the final visual acuity in patients suffering from open globe injuries.
Material and Methods: Prospective observational study was done on 94 patients troubled with open globe injuries. Variables like pre-op visual acuity, associated endophthalmitis, relative afferent pupillary defect, type of injury, globe rupture, retinal detachment were used to assign ocular trauma score (OTS) to each patient, primary repair was done. According to ocular trauma score, visual acuity at six-month post-op follow up was done and compared with the predicted visual outcome.
Results: Males had a higher percentage of patients. Average age was less than 10 years. After analysis, visual acuity at the time of presentation, endophthalmitis, perforating injury, globe rupture, retinal detachment, relative afferent pupillary defect appeared to be associated with worse final visual acuity. The final visual acuity was comparable with the predicted values according to ocular trauma score.
Conclusion: OTS assists as a very useful tool in forecasting the final visual acuity in patients with open globe injuries and can help in management and counseling of the patient and his family.
Introduction
The prevalence of open globe injuries following trauma in both rural and urban areas is quite high and presents with a huge responsibility over the ophthalmologists to manage and deal with such cases. Following an ocular trauma, it is of upmost importance that the ophthalmologist and the patient can comprehend the extent of damage and therefore, predict the visual outcome before all the treatment measures have been taken so that proper counseling of the patient and his family can be done regarding the prognosis and the most appropriate treatment and rehabilitation plan can be devised.
Many factors influence the final visual acuity in patients with open globe injuries like extensive intraocular injuries involving larger areas are related with poor visual outcomes and more post-operative complications [1]. Presence of relative afferent papillary imperfection at the time of presentation [2], retinal detachment [3], poor visual acuity at the time of appearance [4,7] have also been associated with decreased final visual acuity. Similarly, traumatic cataract has been found a very significant vision-limiting factor in all types of open-globe injuries. [5] Along with post traumatic endophthalmitis [6] which significantly reduces the chances of visual rehabilitation after open globe injuries. Due to variation in the type of ocular trauma and a vast range of factors that influence the final visual outcome, it is a huge challenge for the ophthalmologist to predict the final visual outcome.
Many systems have been introduced in the past which tried to incorporate all the factors persuading the final visual result in such patients. Our study is based on assessing the importance of ocular trauma score (OTS) in predicting the final visual acuity in our patients with open globe injuries. OTS has incorporated the most significant variables affecting the visual outcome and given each variable a numerical value. The sum of the numbers belongs to a specific OTS group from which the predicted final visual acuity can be estimated.
Material and Methods
After approval from the hospital administration, prospective observational study of 94 patients who presented to OPD of eye unit two in mayo hospital between first January 2020 to first June 2020 with open globe injuries was done. Patients with previous ocular injuries, with pre-existing chronic ocular diseases e.g., glaucoma, retinopathy, patients with past ocular surgeries, patients with less than four months of follow up were excluded from the study. Proper history of every patient was taken including the age, time between onset of injury and presentation to the hospital, mode of injury, previous ocular injuries or surgeries or any ocular pathology. Thorough examination was done to find the initial visual acuity, extent of injury, relative afferent papillary defect, associated hyphemia, iris prolapse, endophthalmitis, globe rupture, retinal detachment, along with the rest of ocular examination. These findings were utilized via a numerical number to assign ocular trauma score to each patient and categorize it into one of the five OTS categories which predict the final visual acuity after six months. Primary repair was done. Follow up was done after one week, one month and six months and best corrected visual acuity, status of the wound, retinal status, intraocular pressure were specially noted along with the rest of examination. Data was statistically analyzed using SPSS-13. The final visual acuity of patients was compared with the projected values of OTS score (Table 2).
Results
In this research, total of 94 patients with ocular trauma were included (69.1% males; 30.9% females). All of these presented with uniocular trauma either penetrating (91.46%) or perforating (8.51%). Presenting patients had the following age ranges with maximum lying in range <10years (43.6%) (Figure1).
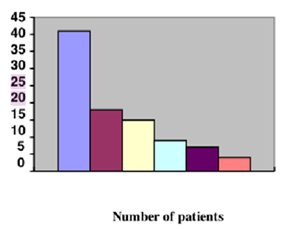
Figure 1: Age Distribution.
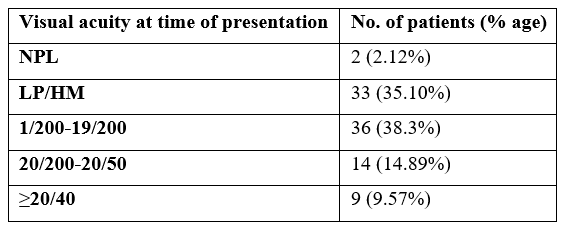
At the time of presentation, 2 eyes were NPL (2.12%), while the visual acuity of remaining is given below in
Table 1:
Complications developed in 44.68% of the patients (42/94). These included Traumatic cataract (16/42), Globe rupture (8/42), Retinal detachment (8/42), Afferent papillary defect (7/42) and Endophthalmitis (3/42). All the observed complications were helpful in evaluating the OTS and Six month follow up showed the final visual acuity which was compared with the expected visual outcome according to OTS study.
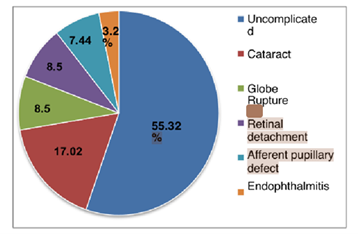
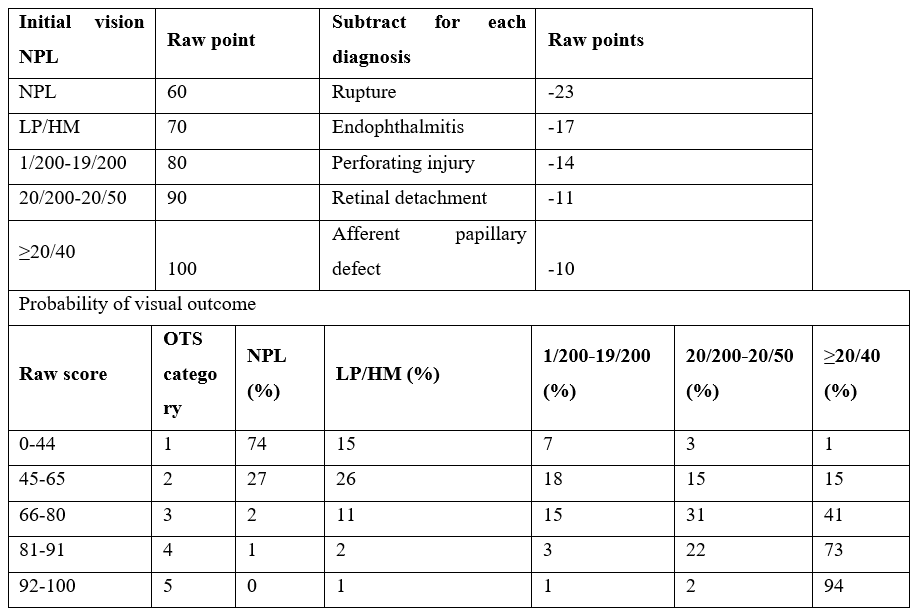
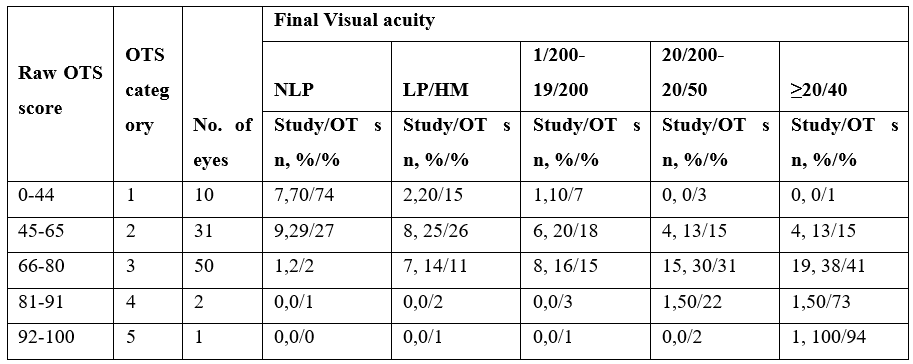
Table 2: OTS calculation and probability of visual outcome.
Most of our patients fell in category two and three of OTS (86%). Presenting visual acuity of 1/200-19/200 was seen in most of the patients (38.3%). Final best adjusted visual acuity of >20/40 was achieved in 25 (26%) of the patients while 45(47.8%) patients in general had reached best corrected final visual acuity of 20/200-20/50 after six months. Overall, results of most of our patients were comparable with the results of OTS study except for OTS category four in which 1 patient (50%) developed final visual acuity of 20/200- 20/50 as opposed to 22% predicted by the OTS study. Overall, there is significant improvement in best corrected visual acuity of our patients.
Table 3: Final visual outcome in our study in comparison with OTS study.
Discussion
OTS is a very effective tool in assessing visual potential in patients with the open globe injuries [8]. It helps in predicting the final visual acuity of the patient which is useful in guiding the patient and his family. Yaprak Banu in her research confirmed the significance of OTS in evaluating the visual potential of patients with open globe injuries [9] Kalla A Gervasio et al in his retrospective study emphasized the significance of initial visual acuity along with OTS as predictor of final visual acuity in patients with combined facial fracture and open globe injury [10]. Rupesh agarwal et al. concludes that preoperative visual acuity, traumatic cataract, mode of injury, hyphaema, vitreous loss, vitreous hemorrhage, relative afferent papillary defect are important factors in foreseeing the final visual acuity in patients with open globe injury. He also stated OTS as a viable analytical tool. In our study 69.1% patients were male indicating the association of outdoor activities with open globe injuries. Vasu et al in his study found that 95% of his patients were males [12]. Many factors show significant relationship with final visual outcome. Factors that are most relevant include age of the patient, relative afferent papillary defect, presence of intra ocular foreign body, endophthalmitis, hyphema, vitreous haemorrhage, retinal detachment [11,13,14]. Similarly, Erdurman FC et al in their research established strong association between presenting visual acuity of worse than 5/200 and poor visual outcome [15]. In our study the initial visual acuity appears to be the main feature associated with poor final visual acuity. The results that we achieved after six month follow up were similar to the results predicted by OTS with very great sensitivity and specificity. Due to the incorporation of factors in OTS that influence the visual potential in patients with open globe injuries it appears to be a very effective method in evaluating the visual outcome in patients with open globe injuries.
Conclusion
OTS score proves to be a very helpful criteria for evaluating the final visual outcome in patients with open globe injuries and hence counsel the patient and his family regarding the visual potential and lifestyle modification that should be done for the betterment of patient.
Limitations: Sample size contained limited number of patients in OTS category four and five therefore the association of variables with final visual outcome could not be assessed with certainty.
References
- Colyer MH, Weber ED, Weichel ED, Dick JS, Bower KS, Ward TP, et al. Delayed intraocular foreign body removal without endophthalmitis during Operations Iraqi Freedom and Enduring Freedom. Ophthalmology, 2007; 114(8): 1439-1447. doi: 10.1016/j.ophtha.2006.10.052.
- Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye (Lond), 2006; 20(12): 1336-1341. doi: 10.1038/sj.eye.6702099.
- Cruvinel Isaac DL, Ghanem VC, Nascimento MA, Torigoe M, Kara-José N. Prognostic factors in open globe injuries. Ophthalmologica, 2003; 217(6): 431-435. doi: 10.1159/000073075. PMID: 14573978.
- Rofail M, Lee GA, O'Rourke P. Prognostic indicators for open globe injury. Clin Exp Ophthalmol, 2006; 34(8): 783-786. doi: 10.1111/j.1442-9071.2006.01309.x.
- Thakker MM, Ray S. Vision-limiting complications in open-globe injuries. Can J Ophthalmol, 2006; 41(1): 86-92. doi: 10.1016/S0008-4182(06)80074-8.
- Silpa-Archa S, Dejkong A, Kumsiang K, Chotcomwongse P, Preble JM, Foster CS. Poor prognostic factors in post- traumatic endophthalmitis following open globe injury. Int J Ophthalmol, 2020; 13(12): 1968-1975. doi: 10.18240/ijo.2020.12.19.
- Rao LG, Ninan A, Rao KA. Descriptive study on ocular survival, visual outcome and prognostic factors in open globe injuries. Indian J Ophthalmol, 2010; 58(4): 321-323. doi: 10.4103/0301-4738.64116.
- Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am, 2002; 15(2): 163-165, vi. doi: 10.1016/s0896-1549(02)00007-x.
- Unver YB, Kapran Z, Acar N, Altan T. Ocular trauma score in open-globe injuries. J Trauma, 2009; 66(4): 1030-1032. doi: 10.1097/TA.0b013e3181883d83.
- Gervasio KA, Weinstock BM, Wu AY. Prognostic Value of Ocular Trauma Scores in Patients with Combined Open Globe Injuries and Facial Fractures. Am J Ophthalmol, 2015; 160(5): 882-888.e2. doi: 10.1016/j.ajo.2015.08.007.
- Agrawal R, Wei HS, Teoh S. Prognostic factors for open globe injuries and correlation of ocular trauma score at a tertiary referral eye care centre in Singapore. Indian J Ophthalmol, 2013; 61(9): 502-506. doi: 10.4103/03014738.119436.
- Vasu Usha, Vasnaik Andrew, Battu Ravindra, Kurian Mathew, George Sony. Occupational open globe injuries. Indian Journal of Ophthalmology, 2001; 49.
- Yu Wai, Man C, Steel D. Visual outcome after open globe injury: a comparison of two prognostic models-the Ocular Trauma Score and the Classification and Regression Tree. Eye (Lond), 2010; 24(1): 84-89. doi: 10.1038/eye.2009.16.
- Meng Y, Yan H. Prognostic Factors for Open Globe Injuries and Correlation of Ocular Trauma Score in Tianjin, China. J Ophthalmol, 2015; 2015: 345764. doi: 10.1155/2015/345764.
- Erdurman FC, Hurmeric V, Gokce G, Durukan AH, Sobaci G, Altinsoy HI. Ocular injuries from improvised explosive devices. Eye (Lond), 2011; 25(11): 1491-1498. doi: 10.1038/eye.2011.212.

