Precautions Taken During the COVID-19 Pandemic in Dental Practices of the Public and Private Sectors: A Cross-Sectional Study from a Developing Country
Muhammad Sharjeel Khan1,*, Urwatulwusqa Uqaili2, Nazia Riasat3, Latif Khan4, Muskaan Harwani5, Zuhair Ahmed Qureshi6, Rida Khalid Soleja7
1Jinnah Sindhi Medical University (Jsmu), Karachi Sindh Pakistan, Pakistan
2Liaquat University of Medical and Health Sciences Jamshoro Sindh Pakistan (LUMHS), Pakistan
3Department of Statistics, North Dakota State University Degree: PhD Statistics, Pakistan
4Altamash institute of dental medicine Karachi, Sindh Pakistan (AIDM), Pakistan
5Altamash institute of dental medicine. Jinnah Sindhi Medical University Karachi, Sindh Pakistan (Jsmu), Pakistan
6Liaquat University of Medical and Health Sciences Jamshoro Sindh Pakistan (LUMHS), Pakistan
7Jinnah Sindhi Medical University Karachi Sindh Pakistan (Jsmu), Pakistan
Received Date: 24/10/2023; Published Date: 04/04/2024
*Corresponding author: Muhammad Sharjeel khan, Instructor Oral Surgery at Altamash institute of dental medicine Degrees: Bachelor in Dental Surgery (BDS), PMDC Reg. Number: 27246-D, Affiliation: Jinnah Sindhi Medical University (JSMU), Pakistan
ORCID: 0000-0003-3491-652X
Abstract
Background: COVID-19 led to a global pandemic, becoming one of the most notable challenges for all healthcare professionals.
This pandemic requires great attention regarding appropriate measures to prevent a surge of the noble virus. Therefore, a study was conducted to assess how dental practices in the public and private sectors in Karachi coped during the COVID-19 pandemic by considering the measures taken following the internal SOPs (Standard Operative Procedures) as per the guidelines of the American Dental Association (ADA).
Method: A well-structured questionnaire was designed with demographic elements of age, gender, profession, and location of the health care practitioners. A list of questions relevant to ADA guidelines for dental practice under the influence of COVID-19 was evaluated among the same population to assess their practice and knowledge regarding using the guidelines. The questionnaire was filled out via social manoeuvre and analysed via the statistical package for social sciences, version 25. The chi-square and Spearman correlation tests assessed the data, and a p-value of less than 0.05 was considered significant for the results.
Results: A total of 418 respondents were evaluated, out of which more than two-thirds of the participants worked in an Outpatient Department (OPD) setup, and only 20.57% of the dentists worked in an executive setup. Overall, 56.45% believed that standard precautions should include avoiding hand shaking, frequent use of sanitiser, avoiding the exchange of equipment, and touching surfaces with bare hands to control the spread in the workplace. In order to prevent cross-contamination, which could hasten the spread of COVID-19, almost 60% of participants recommended taking all precautions in the waiting area, including limiting the number of attendants, maintaining a physical distance of 6 feet, taking the temperature to check for fever, and washing hands. A combination of a surgical face mask and a KN95 mask was suggested by about half of the participants.
Conclusion: This study concludes that there is prevalent awareness among dental healthcare professionals regarding the COVID-19 protocol as per the ADA and various other resourceful guidelines. Dentist’s awareness in the city of Karachi affirms safe practice in dental health care, and this promotes precautionary resistance against the spread and fear of COVID-19 infections involving this array of health care.
Keywords: COVID-19; Standard operating procedures; Dental practice, Pakistan
Introduction
On January 30, 2020, WHO designated COVID-19 a global health emergency [1]. The virus spreads through direct human contact, droplets, and significant aerosol formation in tight spaces [2]. Due to the frequent use of high-speed handpieces and triple syringes, dental procedures produce copious amounts of aerosol, which stays on hands, surfaces, and inanimate objects, suggesting a high infectivity and transmissibility duration [3,4]. Asymptomatic, pre-symptomatic, or symptomatic carriers transfer SARS-COV2 [4]. Exposure to symptoms takes 5–12 days [5]. Fever, tiredness, and coughing characterise mild to moderate cases. Headaches and malaise are rarer symptoms [4].
Like other health professionals, dentists are at considerable risk of contracting the virus [7]. During the initial COVID-19 outbreak, which caused high mortality and infectious rates, many national authorities sought to restrict the typical healthcare practice by which dental healthcare services were greatly affected due to their intimate contact with all routes of transmissibility via COVID-19 carriers or patients. This caused them to limit dental care to urgent nosocomial cases [7,8]. Henceforth, the suggestions to adopt evidence-based COVID-19 preventive SOPs like taking patients' travel history, monitoring body temperature, using a rubber dam, and using a high-volume suction were recommended to be consistently used in dental clinics [5,6].
The ADA issued recommendation guidelines during the outbreak to influence safer practice based on experiences with COVID-19 patients in different healthcare setups. After careful evaluation, these guidelines were considered applicable to all dental patients [6]. The guidelines involved adaptation to extra-oral radiographs such as orthopantomograms and cone beam computed tomography instead of intra-oral radiographs. Furthermore, periodontal procedures were suggested to be assisted with ultrasonic scalers instead of hand scalers to avoid further contamination by direct contact with aerosol and splatter spread. It also involved guidelines to encourage dentists to conduct only emergency dental procedures as per the ADA [3,6].
This questionnaire-based study aims to evaluate awareness, knowledge, and precautions in practice as per the new ADA guidelines for COVID-19 at dental practices conducted in the public and private sectors in Karachi, the largest city in Pakistan. It highlights comparisons in the use of international ADA guidelines.
Methodology
A cross-sectional survey was conducted in Karachi among institutions belonging to the public and private sectors from March 2023 to June 2023 on precautions taken during COVID-19 in dental practices in the public and private sectors. The ethical review committee of Altamash Institute of Dental Medicine, Karachi, Pakistan, approved the study protocol before initiating the formal survey. A total of 418 participants participated in it, including house officers/interns, residents, and private practitioners. The sample size was estimated using Epi Info software, assuming that 50% of the dentists adopted COVID-19 SOPs with a 95% confidence level and a bound-on error of +-9%. Data was collected using a self-administered structured questionnaire and analysed using SPSS version 25.
A well-structured questionnaire was designed, and an online medium through social media was adopted to distribute it as the route of transmission of COVID-19 is through human interaction. The survey comprised 12 questions, which were divided into two sections: demographics and preventive strategies. Descriptive analysis was done to calculate frequencies and percentages for the socio-demographics and preventive measures taken towards COVID-19 using the statistical package for the social sciences (SPSS) version 25. The descriptive analysis was taken out for the demographic distribution and association of the variables, and various tests like the chi-square test and the Spearman correlation were applied to the data. The Spearman test detected a relationship between the healthcare professional's response concerning their gender and age. A p-value of < 0.05 was considered statistically significant.
Results
A total of 418 participants recorded their responses. The descriptive data of the participants is presented in Table A1. Out of the total 418 participants, 318 were females and 100 were males. 89.95% of the participants belong to the age group ranging between 20 to 29 years, and 36 participants are between 30 and 39. No participants were aged between 15 and 19 and over 50 years. Among all the participants, 238 (56.94%) HCPs belonged to the private outpatient departments, 94 (22.49%) worked at the public sector outpatient department, and 86 (20.57%) worked at the executive clinics.
The active preventive strategies in practice by healthcare professionals towards COVID-19 are presented in the following table:
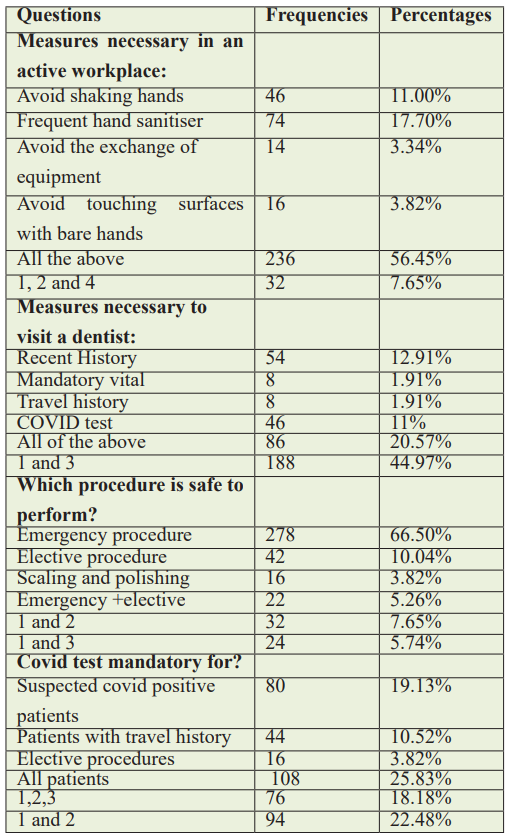
On evaluation, 46% of participants thought that necessary measures to control the virus at the workplace should include avoiding handshaking. In an active workplace, 74% believe that frequent sanitiser use is a critical measure. Overall, 56.45% of people have endorsed avoiding hand shaking, frequent use of sanitiser, avoiding the exchange of equipment, and touching surfaces with bare hands to control the spread in any active workplace.
Among all 278 (66.51%) participants believed that emergency procedures are safest to perform, and only 3.83% suggested that scaling and polishing are safer procedures to perform. Of 418 participants, 25% thought the COVID test should be mandatory for all patients.
The execution level of healthcare professionals toward COVID 19 is as follows, around 60.29% of participants suggested that all the precautions, attendants should be at least six feet apart and limited to one, temperature measurements, and sanitation should be performed as precautions in the waiting area before triage. Out of 418 responses, 30% support pre-procedural mouthwash, reduction of the three-way syringe, and rubber dams to help reduce microbes in an aerosol. Around 91% of participants think that surgical gowns, face masks, and gloves should be used to limit the transmission of the virus.
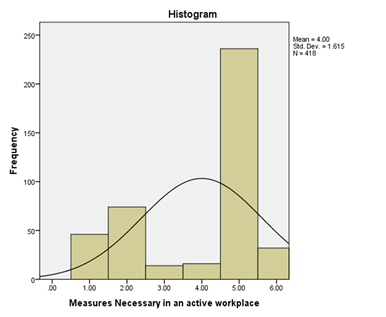
where 1= Avoid shaking hands, 2= frequent hand sanitizer, 3= Avoid exchange of equipment, 4= Avoid touching surfaces with bare hands, 5= All of the above and, 6= 1,2 and 4
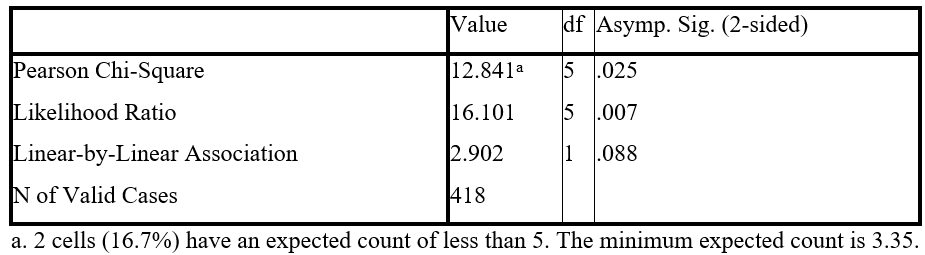
Chi-square calculations:

Where Age groups are divided as: 1=15-19, 2=20-29, 3=30-39, 4=40-49, 5=50-59, 6=60-69.
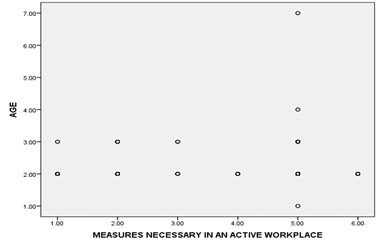
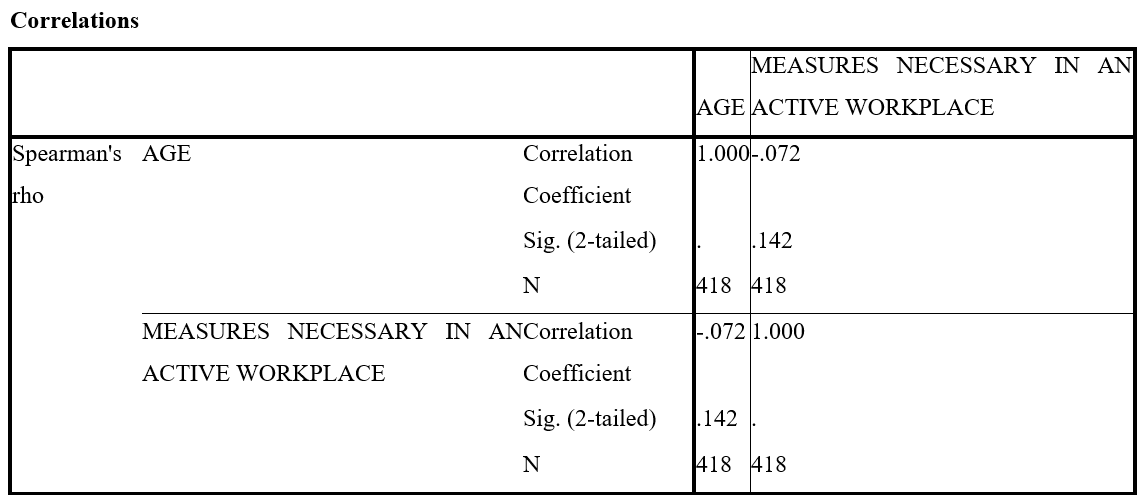
Nonparametric Correlations
The chi-square test has been applied to check the association between the dentist's response and their gender. On evaluation and analysis of the association between dentist’s responses and gender, the chi-square test gave us evidence that dentist responses have some degree of association with gender female that includes the proportion of workplace (32.50%), measures necessary in the workplace (17.53%), measures necessary to visit dentists (22.09%), COVID-19 test mandatory (25.87%), waiting for area precautions (19.35%), reducing microbes in aerosol (20.25%), and protocol to limit the transmission (17.40%). The chi-square test shows a statistically significant relationship between gender and protocols to limit transmission with a p-value less than the level of significance of alpha = 0.05.
Spearman correlations have been applied to the data set. The results show that variable age was a negative (-0.072) correlation measure with the dentist's responses to protocols to limit transmission. The sig 2-tailed value of 0.142 is greater than the alpha. Overall, according to the Spearman correlation, there is no positive association between dentist’s responses and the variable age.
Discussion
The results of this study showed that from March to June 2021, 418 participants responded via the online questionnaire, and among them, the largest dental professionals were compliant and aware of the ADA guidelines. Furthermore, on close inspection of the data, it was found that the demographic distribution via descriptive statistics highlighted 76.07% female respondents and the rest, 23.92%, representing male respondents, as per Table 1. Our study started with a socio-demographic demonstration of the respondents, which showed relevant results to an earlier study conducted in Polish dental health care. The resemblance started with gender respondents having an ample response count of females in the dental profession in Poland; out of 730 dentists, 641 were females. Our respondents mostly belonged to the age group of 20–29 years old, with the prevalence of dentists from 238 private clinics in comparison to responses from 94 Public sector OPD and Executive clinic dentists; this data also precipitated comparison with the Polish study on the same narrative, highlighting 372 private practice dentists and 320 NHF dentists [9].
Additionally, our study evaluated various aspects of dental care in light of the COVID-19 outbreak. The socio-demographic component of the questionnaire focuses on attitudes and knowledge of what dental healthcare professionals during the COVID-19 outbreak should perform. The results in our section are based on fundamental questions such as "What measures are necessary for an active workplace during the COVID-19 pandemic?" The respondents were given options to choose the most suitable measure as per their knowledge and awareness of COVID-19. Out of 418 participants, 236 showed responses for all measures mentioned in the question, i.e., avoiding handshakes, frequent hand sanitisation, avoiding the exchange of equipment, and halting contact with surfaces using bare hands. This response showed relevant awareness of the precautionary measures as per the guidelines of the ADA for the COVID-19 era [3].
Furthermore, the section on attitude and exercise assessment involved measures necessary to allow patients a grant for a dental visit; 188 respondents affirmed choosing careful evaluation of a patient's recent travel history, while 86 respondents considered it mandatory to evaluate a patient's dental visit via the record of prior mentioned histories alongside a COVID-19 test and vital check. A great number of respondents, 108, further suggested making the COVID test mandatory for a dental visit. In contrast, others fluctuated between patients with a suspected COVID history, patients with a travel history, or patients who must undergo an elective procedure at the dental clinic. This information suggested that the dentists at different clinical setups in the city of Karachi, Pakistan, were aware of the information regarding protocols issued by various societies and associations, such as the ADA and WHO, to deal with a patient during the COVID-19 wave surge, like various dental professionals internationally, such as dentist's in Switzerland, Turkey, and Italy [10–12].
The questionnaire further follows up on a great deal of precautionary practice in limiting the spread of COVID-19 through dental care. Our study asked dentist respondents how they would approach any patient in their setup, especially COVID-19-positive patients requiring urgent dental care. Among the respondents, ample professionals opted for PPE and pharmaceutical treatment of the disease for the patient, which aligns with protocols under the ADA guidelines; others opted for these same measures as an individual regime in practice. Furthermore, our study highlights what prophylactic measures should be utilised in the waiting area before providing dental healthcare to avoid COVID-19; the respondents believe safe practices in relevance to COVID-19 patients in the waiting area involve checking temperature, a minimum of 6 feet between COVID-19 patients in the waiting room, sanitisation before entry and a limited number of attendants in accomplice with that patient. Our study also asked the respondent dentist's on how the reduction of microbes could be optimised in the dental care facilities of their setup. They chose pre-procedural mouthwash, rubber dams, and reducing the use of three-way syringes in varying proportions, this result precipitated a correlation with the guidelines under dental association [9,10].
Limitations: Our study lacks a complete geographical representation of the country Pakistan; the data of this study was conducted in a concise period, resulting in a smaller sample collection. The study faces limitations in evaluating all hospitals in Karachi due to a lack of compliance with filling out the questionnaire by all dentists; henceforth, the representation needs to be more generalisable.
Lastly, our study assessed their willingness to resist further virus transmission by wearing N95, surgical masks, and any relevant physical barrier to avoid aerosol contact, and these responses were consistent with previous international studies. [10]
Conclusion
This study highlights the results affirming knowledge, behavior, and practice utilisation under ADA guidelines, and this promotes a safer practice around dental health care in Karachi's public and private sectors. Safe practice and sound knowledge of the surge of COVID-19 waves ultimately result in protection and limit virus transmission. This break in the chain of infection results in the reduction of the increased incidental rates of the virus in the area under a COVID-19 wave and the control of the nation's COVID-19 case rate.
Acknowledgements: None.
Funding: None
Conflict of interests: None
Data availability: Data will be available upon reasonable request to the corresponding author.
References
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N Engl J Med, 2020; 382(13): 1199-1207. doi: 10.1056/NEJMoa2001316. Epub 2020 Jan 29. PMID: 31995857; PMCID: PMC7121484.
- Zhu H, Wei L, Niu P. The novel coronavirus outbreak in Wuhan, China. Glob Health Res Policy, 2020; 5: 6. doi: 10.1186/s41256-020-00135-6. PMID: 32226823; PMCID: PMC7050114.
- Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci, 2020; 12(1): 9. doi: 10.1038/s41368-020-0075-9. PMID: 32127517; PMCID: PMC7054527.
- Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA, 2020; 324(8): 782-793. doi: 10.1001/jama.2020.12839. PMID: 32648899.
- Ge ZY, Yang LM, Xia JJ, Fu XH, Zhang YZ. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang Univ Sci B, 2020; 21(5): 361-368. doi: 10.1631/jzus.B2010010. Epub 2020 Mar 16. PMID: 32425001; PMCID: PMC7089481.
- Ahmed MA, Jouhar R, Ahmed N, Adnan S, Aftab M, Zafar MS, et al. Fear and Practice Modifications among Dentists to Combat Novel Coronavirus Disease (COVID-19) Outbreak. Int J Environ Res Public Health. 2020; 17(8): 2821. doi: 10.3390/ijerph17082821. PMID: 32325888; PMCID: PMC7216192.
- COVIDental Collaboration Group. The COVID-19 pandemic and its global effects on dental practice. An international survey. J Dent, 2021; 114: 103749. doi: 10.1016/j.jdent.2021.103749. Epub 2021 Jul 17. PMID: 34280498; PMCID: PMC8285212.
- Abdelrahman H, Atteya S, Ihab M, Nyan M, Maharani DA, Rahardjo A, et al. Dental practice closure during the first wave of COVID-19 and associated professional, practice and structural determinants: a multi-country survey. BMC Oral Health, 2021; 21(1): 243. doi: 10.1186/s12903-021-01601-4. PMID: 33962609; PMCID: PMC8102846.
- Turska-Szybka A, Prokopczyk M, Winkielman P, Olczak-Kowalczyk D. Knowledge and Attitude of Polish Dental Healthcare Professionals during the COVID-19 Pandemic. Int J Environ Res Public Health, 2021; 18(22): 12100. doi: 10.3390/ijerph182212100. PMID: 34831856; PMCID: PMC8621051.
- Putrino A, Raso M, Magazzino C, Galluccio G. Coronavirus (COVID-19) in Italy: knowledge, management of patients and clinical experience of Italian dentists during the spread of contagion. BMC Oral Health, 2020; 20(1): 200. doi: 10.1186/s12903-020-01187-3. PMID: 32650753; PMCID: PMC7349471.
- Duruk G, Gümüşboğa ZŞ, Çolak C. Investigation of Turkish dentists' clinical attitudes and behaviors towards the COVID-19 pandemic: a survey study. Braz Oral Res, 2020; 34: e054. doi: 10.1590/1807-3107bor-2020.vol34.0054. Epub 2020 May 29. PMID: 32490887.
- Wolf TG, Zeyer O, Campus G. COVID-19 in Switzerland and Liechtenstein: A Cross-Sectional Survey among Dentists' Awareness, Protective Measures and Economic Effects. Int J Environ Res Public Health, 2020; 17(23): 9051. doi: 10.3390/ijerph17239051. PMID: 33291659; PMCID: PMC7730085.

