Clinical Diagnostic Immunological Tests in A TB/HIV/AIDS Hospital Laboratory
Philip Ifesinachi Anochie1,2,*, Clementina Oghale Awenede2, Augustine Osasemeaga Okpiabhele2, Lucia Chioma Anochie1,4, Nelson Chibueze Anochie1,4 and Marcos Roberto Tovani Palone3
1Research Scientist/ Coordinator, Immunology and Vaccination Research Group, Philip Nelson Institute of Medical Research, Lagos, Nigeria
2TB/HIV/AIDS/NTD Research Group, Michael and Cecilia Ibru University, Agbarha Otor, Ughelli, Delta State, Nigeria
3Research Scientist, University of Sao Paulo, Brazil
4Department of Microbiology, Imo state University, Imo state, Nigeria
Received Date: 23/09/2023; Published Date: 28/02/2024
*Corresponding author: Philip Ifesinachi Anochie, Research Scientist, Immunology and Vaccination Research Group, Philip Nelson Institute of Medical Research, Lagos, Nigeria
Abstract
This review unravels the novel approaches, innovations and applications of immunology in the diagnosis of infections in a clinical microbiology laboratory. Many assays or tests in immunology are used in the diagnosis of infections. The availability of monoclonal antibodies has brought rapid progress to this area and they are used, for example, to identify specific microorganisms in culture or in tissues and fluids from infected patients.
Examples of common diagnostic applications of antibody- antigen reactions discussed here includes agglutination tests, complement tests, complement fixation tests, ELISA, cytotoxic tests, radioimmunoassay tests, haemagglutination inhibition tests, hypersensitivity tests, phagocytic cell activity test, migration inhibition test, lymphocyte transformation test, lymphocyte fixation test, skin tests, delayed hypersensitivity tests and many others.
The development of monoclonal antibody technology and the subsequent availability of unlimited quantities of pure antibody has improved the selectivity of these assays. The development of simple and highly sensitive methods for detection of nucleic acids is being applied to diagnosis of infection using nucleic acid hybridization and this provides a valuable additional aid to immunoassays in the clinical microbiology diagnostic laboratory.
Keywords: Clinical; Diagnostic; Immunology; Microbiology; Laboratory
Introduction
Clinical diagnostic immunology is the application of immunology in the diagnosis of infections. Many assays or tests in immunology are used in the diagnosis of infections. The availability of monoclonal antibodies has brought rapid progress to this area and they are used, for example, to identify specific microorganisms in culture or in tissues and fluids from infected patients. Agglutination, complement fixation tests, virus neutralization tests, ELISA assays, coagulation tests (i.e., blood grouping), radioimmunoassay and immunofluorescence (G6PD deficiency fluorescence tests) are widely used in the clinical microbiology laboratory [1].
Antigens reacts with antibodies to form an immune complex. Immune complex detection can be valuable in the diagnosis of bacterial endocarditis. The development of simple and highly sensitive methods for detection of nucleic acids is now being applied to diagnosis of infection using nucleic acid hybridization and is likely to provide a valuable additional aid to immunoassays in the diagnostic laboratory [2].
Examples of some common clinical microbiology diagnostic applications of antigen- antibody reactions in medical microbiology are agglutination tests, complement-fixation tests and haemagglutination –inhibition tests.
Clinical diagnostic immunology is therefore an interaction of antibody with antigen as applied to laboratory investigations [3].
Agglutination Tests
In this reaction, the antigen is part of the surface of some particulate material, such as a red cell, bacterium or perhaps an inorganic particle (e.g., polystyrene latex) which has been coated with antigen. Antibody added to a suspension of such particles combines with the surface antigens and links them together to form clearly visible aggregates or agglutinates [4].
In its simplest form, an agglutination test is set up in round- bottomed test tubes or Perspex plates with round-bottomed wells and doubling dilutions of the antiserum are made up in the tubes [5].
The particulate antigen is then added and after incubation at 37 oC, agglutination is seen in the bottom of the tubes. The last tube showing clearly visible agglutination is the end point of the test [6].
One of the classical applications of the agglutination test in diagnostic bacteriology is the widal test used for the demonstration of antibodies to Salmonellae in serum specimens taken from suspected enteric fever cases [7].
Agglutination is the basic technique used in blood grouping, the A, B, or O group of the red cells under test being determined by agglutination with a specific antiserum-an anti-A serum for example will agglutinate A cells but not B or O cells. Red cells and inert particles such as polystyrene latex can be coated with various antigens and suitably coated particles are used in a variety of diagnostic tests such as thyroid antibody cells using thyroglobulin –coated cells or latex particles [8].
Hormone –coated red cells or inert particles are used in many hormone assay procedures which are based in the inhibition of the antibody –induced agglutination of the hormone-coated particles by hormone added in the sample under test. Test of this type are in wide use in pregnancy diagnosis [9].
Certain viruses, e.g., the myxoviruses causing influenza and mumps, have the property of bringing about agglutination of red cells (haemagglutination). Inhibition of haemagglutination by antibody in patient’s serum is a widely-used diagnostic procedure. The presence of antibody in the patient’s serum is therefore detected by its ability to link with virus particles and prevent them from bringing about agglutination of the red cells. IgM antibodies capable of agglutinating human red cells (including those of the individual producing the antibody) between 0 oC and 4 oC are sometimes found in certain human diseases including primary atypical pneumonia, malaria, trypanosomiasis and acquired haemolytic anaemia [10].
The presence of antibody globulin in a red cell may not result in direct agglutination of the cells, for example, in some Rh-negative mothers with Rh-positive infants or in acquired haemolytic anaemia. It is, however, possible to show that the red cells are coated with antibody by using an antiglobulin serum (produced in the rabbit by injecting human globulin) which will bring about agglutination of the cells. This is the basis of the Coomb’s test which is a very widely used serological procedure. The coagulation test depends on the presence of protein A [11].
The agglutination test already referred to for the serodiagnosis of Salmonella infections is known as Widal test. It is usual to test dilutions of the patient’s serum against standard suspensions of somatic (O) antigen and flagellar (H) antigen of each organism likely to be encountered in the patient’s environment. The test usually becomes positive with both suspensions, a week after the onset of the illness but may be weakly positive with one of the antigens even earlier [12].
The titre in an acute infection rises to a maximum by the end of the third week. Complications in interpretation of the results may arise in patients who have been immunized with typhoid –paratyphoid vaccine (TAB). A rising titre may be of some help in diagnosing an infection; furthermore, some months after immunization, the titre of O agglutinins tends to fall off leaving only H agglutinins. Normal sera sometimes have low titres of agglutinins for Salmonella organisms and this varies in populations in different parts of the world [13].
These difficulties make the test of questionable diagnostic value and its use is now limited. Another widely used agglutination test is the Paul- Bunnel reaction. This is used for the diagnosis of infectious mononucleosis in which agglutinins develop for sheep erythrocytes. Normal serum may agglutinate sheep cells in low dilutions and a titre of 128 is taken as suggestive and 256 as positive for the test [14].
In some individuals who have received horse serum as a therapeutic agent (e.g., antitetanus serum) agglutinins develop for sheep cells because of the presence in the horse serum of an antigen very widespread in nature, known as Forssman antigen. This antigen is present in the red cells of sheep and the cells of a number of other species, including the guinea –pig [15].
The usual way of differentiating the two types of antibodies is to mix the serum with minced guinea-pig tissue (usually kidney). This treatment will absorb out the anti-Forssman antibody leaving the anti-sheep cell antibody unaffected. Ox red cells, which contain both the Forssman antigen and an antigen similar to that on sheep cells which reacts with the Paul-Bunnel antibody, will absorb out both types of antibodies [16].
Complement Fixation Tests
The classical complement-fixation test is the Wassermann reaction used in the diagnosis of Syphilis. The test system consists of Wassermann antigen mixed with dilutions of the patient’s serum in the presence of guinea-pig complement. After the antigen and patient’s serum have had time to react and take up the limited amount of compliment available in the system, the indicator system is added to show whether or not there is free complement [17].
Controls are included to ensure that none of the reagents are anticomplementary (able to take up complement nonspecifically as might, for example, occur with contaminated serum) and positive and negative control sera are tested in parallel [18].
These tests have wide applications in the diagnosis of bacterial and viral infections. One of the most commonly used methods is the Wasserman test used in the diagnosis of Syphilis. This reaction depends upon the fixation of complement by the patient’s antibody after it has reacted with cardiolipin, an alcoholic extract (a phosphatide lipoid) from normal animal tissues, usually ox heart. Why antibodies against this material develop in Syphilis is not clear. Some workers suggest that it results from autoimmunization with host lipids made antigenic in some way by Spirochaete (Trep. pallidum) responsible for Syphilis, while others believe that the Spirochate contains a cell wall antigen related to the tissue antigen [19].
Interpretation of the results of the Wassermann’s test is difficult and a final assessment depends on the results of both this and other serological tests and the clinical findings [20].
False –positive reactions are sometimes found in leprosy, malaria, sleeping sickness, tuberculosis, infectious mononucleosis and other febrile diseases. Persistent false-positive reactions are sometimes found in autoimmune haemolytic anaemia, systemic lupus erythematosus, and liver cirrhosis. A commonly performed test is the slide flocculation test using cardiolipin mixed with patient’s serum. This test is preferred by many laboratories because of its simplicity, as an alternative to the Wassermann test. It is known as the VDRL (Venereal Diseases Research Laboratory) slide test [21].
When there is doubt, a more specific test may have to be employed e.g., the treponomal immobilization test, in which motile treponemata can be seen to be immobilized when examined microscopically after exposure to patient’s serum. This test is, however, technically complicated and has largely been replaced by an indirect fluorescent antibody test (fluorescent treponemal antibody absorbed, FTA-ABS test). The test is highly specific and sensitive. It is able to detect antibody at all stages of syphilitic infection [22].
The Enzyme-Linked Immunosorbent Assay (ELISA) has the potential for large-scale application in syphilis serology. Complement- fixation tests are used widely in the diagnosis of virus diseases. The source of the antigen is usually the infected tissues of animals, or eggs, or infected tissue cultures. The virus is usually extracted from the tissues or cells by differential centrifugation or sometimes by purifying the virus by adsorbing it on to red cells and then eluting it later. Complement –fixation tests are used routinely for detecting viruses in tissue cultures which have been inoculated with specimens of blood or tissue fluids from humans with probable virus infections [23].
Antigen – Antibody Reactions Using Fluorescent Labels
The precise localization of tissue antigens or the antigens of infecting organisms in the body, of antitissue antibody and of antigen/antibody complexes was achieved by the introduction of the use of fluorochrome –labelled proteins by Coons and Kaplan in 1950. The adsorption of ultraviolet light between 290 and 495 nm by fluorescein and its emission of longer wavelength green light (525nm) is used to visualize protein, labelled with this dye. The technique is more sensitive than precipitation and complement –fixation techniques, and fluorescent protein tracers can be detected at a concentration of the order of 1ug protein per ml body fluid [24].
Some of the uses to which the technique has been put include the localization of the origin of a variety of serum protein components, for example, immunoglobulin production by plasma cells and other lymphoid cells. The demonstration and localization in the tissues of antibody globulin in a variety of autoimmune conditions has been shown, including an antinuclear antibody in the serum of patients with systemic lupus erythematosus and thyroid autoantibodies in the sera of patients with Hashimoto’s thyroiditis [25].
In clinical diagnosis field, in the clinical microbiology laboratory, most human pathogens can be demonstrated by immunofluorescence and a tentative diagnosis may be made much sooner than by cultivation by rapid molecular biology techniques. The fluorescent method at present can be used to supplement rather than replace conventional clinical diagnostic methods [26].
Other types of labelled antibody test have been developed on the same principles as the fluorescent methods [27].
Cytotoxic Tests
Tests of this type are used in combination with red blood cell agglutination for studying histocompatibility antigen systems in tissue typing. The cytotoxic test consists essentially of determining whether or not the permeability of cells changes after their incubation with antibody and complement [28].
Cytotoxic antibody, after combination with the target cell, will activate complement components and bring about changes in permeability of the cell membrane. The permeability changes can affect the ability of the cell to exclude a dye such as trypan blue which will penetrate the cell and be visible by simple microscopic examination [29].
Although the test is applicable to a wide range of nucleated cells and is the test of choice with blood leucocytes, it is rather less sensitive than the red cell haemagglutination tests and more laborious to perform [3].
Radioimmunoassay Methods
Increasing use has been made over the last few years of immunologically based assay methods for the accurate quantitative estimation of polypeptide hormones. These methods offer a unique combination of specificity, precision and simplicity and are already available for the assay of some 14 of the 20 or so polypeptide hormones in man. Monoclonal antibodies are now used extensively in the tests. The principle of the assay methods is that radio-iodine labeled (purified) hormone competes with the non-labeled hormone of a sample under test for the antihormone antibody with which the labeled and non-labeled hormone are mixed [21].
The more of the hormone in the test sample, the less chance the labeled hormone has of combining with the limited number of antibody molecules that are available in the antihormone serum. Therefore, by measuring the quantity of labeled hormone combined with antibody (using isotope counting equipment), a measure of the hormone in the test sample can be obtained [22].
The more labeled hormone combined with antibody, the lower the hormone level in the test sample. The quantity of isotope labeled hormone complexing with the antihormone antibody varies inversely with the quantity of unlabeled hormone in the test sample [23].
In order to measure the amount of labeled hormone attached to the antibody, it is necessary to separate the hormone /antibody complexes from the mixture. A variety of methods have been developed to achieve this, perhaps the most common being attachment of antibody to inert particles that can be removed by centrifugation [24].
Using the principle of competitive binding radioimmunoassay, an assay for IgE levels in serum has been developed using iodine labeled IgE and anti-IgE linked to cellulose, and assays using these principles are being developed for the detection of hepatitis B antigen in human serum [25].
Enzyme –Linked Immunosorbent Assay (ELISA)
This is an immunoassay using enzyme-linked antibody or antigen. Labels other than radioactive isotopes and fluorescent dyes can be linked on to antibody or antigen molecules. Enzymes such as horseradish peroxidase or alkaline phosphatase are linked to antibody or antigen molecules. The presence of the enzyme-linked molecule is detected by means of the enzyme substrate and can be measured by spectrophotometry [26].
Either the labelled antigen or the antibody can be attached to an insoluble support, such as plastic beads, or plastic agglutination plates. After the material has attached and the excess has been washed away, enzyme-linked antigen or antibody is added, together with the test substance. The antigen or antibody (whichever is being measured) in the test solution competes with the added labeled antigen or antibody reagent for the material attached to the plastic plates. The amount of enzyme- labeled reagent can then be estimated by the addition of enzyme substrate [27].
The product of the reaction between enzyme and substrate is finally determined by spectrophotometry. There are a number of variations of the technique similar to those used in fluorescent antibodies. These include a sandwich technique with antibody bound to the plastic plate, the antibody to be assayed as the second layer and enzyme linked to immunoglobulin as the top layer. Enzyme substrate is finally added and the product determined in the spectrophotometer by color change [28].
The technique has been applied widely in detection of bacterial and viral antigens and antibodies, particularly for rotavirus and cytomegalovirus. It has been of use in the study of a variety of parasitic diseases due to helminthes or protozoa. These assays are increasingly used for qualitative and quantitative determinations of macromolecules [29].
The development of monoclonal antibody technology and the subsequent availability of unlimited quantities of pure antibody has improved the selectivity of these assays. The drawback of the limited surface area of the wells of the micro titer plates used in the assay can be overcome by the use of macro beads (e.g., polystyrene latex or Dynal copolymer beads). The beads are coated with the appropriate reagent and the detection stage involves the use of fluorescent or enzyme conjugation. The sensitivity of test of this type tends to be lower than that of assays in ELISA plates [10].
Haemagglutination – Inhibition Tests
Another useful procedure for the diagnosis of some types of virus disease is the haemagglutination –inhibition test. This depends on the fact that certain viruses, e.g., those of influenza, mumps and parainfluenza, will agglutinate chicken, human and guinea-pig red cells. Other viruses e.g., the adenoviruses, agglutinate rat or monkey red cells; the reoviruses and many enteroviruses agglutinate human red cells [11].
The test is performed by mixing the virus with the appropriate red cells in the presence of patient’s serum. If antibodies to the virus are present, the virus will be unable to bring about haemagglutination. These tests are very valuable in diagnostic immunology because of their extreme specificity and their ability to distinguish antibodies to various substrains and variants of viruses, e.g., the influenza virus [12].
The complement-fixation test on the other hand is less valuable for detecting these fine differences of distinguishing antibodies to various substrains and variants of viruses [13].
Tests of the Function of the Cell –Mediated Immune System
The tests used to test for the function of the cell-mediated immune system are the skin tests, lymphocyte function tests, lymphocyte transformation tests, migration inhibition test, test of phagocytic cell activity, complement system test, immune complex detection tests and other detection methods in general that require specialized laboratory facilities [14].
Skin Tests
Type IV; cell mediated or delayed hypersensitivity skin test is a classical method for testing the responsiveness of the cells involved in cell-mediated immunity. The tuberculin response is the best-known example. It is induced by the intradermal injection of 0.1 ml of a 1: 1000 dilution (or a greater dilution in a highly sensitive individual) of a protein extract of tubercle bacilli (purified protein derivative, PPD) [15].
This reaction is only one of a number of similar tests of delayed hypersensitivity such as that using lepromin (in leprosy) and brucellin (in brucellosis). One of the main uses of tests of this type is to detect sensitization to the relevant microorganism, as for example prior to the use of the BCG vaccine in the prevention of tuberculosis [16].
Clearly in the presence of a positive tuberculin test, immunization with the vaccine will not be called for. A negative reaction in an adult, particularly in one known to have previously shown a positive test, raises the possibility of a defect of the cell-mediated immune system, which in the adult would likely to be secondary to some disease state affecting the lymphoid tissues such as Hodgkin’s disease, multiple myeloma, Leukaemia and Lymphosarcoma [17].
Lymphocyte Function Tests
A particularly useful and widely used assay of lymphocyte function is the lymphocyte transformation test. This is usually carried out using plant phytohaemagglutinin (PHA) as the stimulating agent. In other situations, a transformation test may be performed with specific antigens to which the individual is believed to be sensitized (e.g., tuberculin) [18].
In contrast to the use of PHA, which stimulates a high proportion of T-lymphocytes, specific antigen will only stimulate those lymphocytes that are specifically “committed” to the antigen in question and this is usually only a small portion of the total T-lymphocytes. A low level of lymphocyte transformation (when compared with control subjects), either with PHA or specific antigen, indicates impaired cell –mediated immunity (or perhaps, absence of previous exposure to the antigen used), whilst increased transformation in the presence of a specific antigen may occur in certain hypersensitivity states e.g., drug allergies [29].
Migration Inhibition Test
A modification of the macrophage migration inhibition test using human peripheral blood leucocytes (instead of guinea –pig peritoneal macrophages) can be used in the assessment of cell-mediated immunity. Peripheral blood leucocytes are collected in a small capillary tube in the same way as for the macrophage inhibition test and, when put in a culture chamber, grow out of the end of the tube in a fan shape. If, however, antigen, to which the cell donor has previously been sensitized, is put into the chamber, the leucocytes fail to grow out of the tube [1].
This inhibitory effect is due to a “lymphokine” produced by the sensitized lymphocytes on exposure to antigen. This form of assessment of lymphocyte function has very much the same value as the transformation tests referred to above [2].
Phagocytic Cell Activity Test
Defective phagocytic mechanisms can be assayed in a variety of ways in the laboratory.
- The ability of phagocytes to respond to a chemotactic agent (e.g., antigen/antibody complexes in fresh serum) can be measured by inducing the phagocytes to migrate from a chamber through a Millipore membrane towards an outer chamber containing the Ag/Ab complexes and serum [3]. The number of phagocytes that respond can be estimated by removing the membrane, staining it with a suitable stain and, under the microscope, counting the number of cells either in the process of passing through the membrane or on the outer side of the membrane [4].
- The ability of phagocytes to injest and kill microorganisms (e.g., Staphylococci) or ingest inert particles such as latex or oil droplets can be determined by microscopic examination of cell preparations mixed with the microorganisms or inert particle. Killing of microorganisms within phagocytes can be estimated by disrupting the cells e.g., by distilled water and counting the colonies of microorganisms that can be grown on a suitable nutrient agar plate [5].
- The normal functioning of phagocyte lysosomal enzyme activity can be assessed by a dye reduction test using tetrazolium nitroblue. A defect on the part of the patient’s cells can be detected by a failure of the leucocytes to reoxidise the reduced colourless dye to its blue colour. A deficiency of this function is characteristic of chronic granulomatous disease [6].
The Complement System Test
Changes in the levels of this complex group of serum protein constituents are often a reflection of an underlying disease process. Raised levels of the complements are frequently found in acute inflammatory and infective disease states in conjunction with raised levels of “acute phase proteins” such as C reactive protein [7].
Reduction in complement levels is a more useful guide to the understanding of disease pathogenesis and falls into two categories:
- Primary deficiencies: These are genetically determined deficiencies of complement components and
- Secondary deficiencies: This is as a result or consequence of complement consuming antigen- antibody interactions or associated with renal or liver disease. The genetically determined deficiencies are rare conditions, the best known of which is the deficiency of C1 esterase inhibitor. Very rare deficiencies of other components (C3, C1, C5) have been described. The secondary deficiencies are much more frequently found and most often occur in renal disease such as poststreptococcal nephritis, in the nephritis of systemic lupus erythematosus and in chronic membranoproliferative glomerulonephritis. Low levels also occur in serum sickness (immune complex disease), bacteria septicaemia, malaria and in various forms of liver disease [8].
In the laboratory, two main types of assay are available.
- Functional tests of the haemolytic activity of the complement system, and
- Immunochemical estimation of the levels of individual complement components.
Haemolytic activity of the complement system is usually assayed by the method described by Mayer, which measures the number of “units” of complement per ml of serum. A unit of complement is defined as the quantity required to lyse 50% of a standard sheep cell suspension, optimally sensitized with anti-sheep cell antibody. The volume, buffer components and incubation condition are likewise defined. The test is sometimes referred to as a CH5O assay. Estimation of individual components, while possible by assays of their functional activity, is usually performed by immunochemical methods utilizing specific antisera against individual components. The method of choice is the quantitative radial immunodiffussion test in which the antisera are incorporated in the agar and the serum specimens are placed in the wells. Commercially prepared plates are available for a wide range of complement components [9-11].
Immune Complex Detection Test
In the circulation of the immune system, the potentially pathogenic complexes are those found in antigen excess. There is now convincing evidence that they play a role in the pathogenesis of rheumatoid arthritis, glomerulonephritis, polyarteritis, rheumatic fever and a number of infective states [12].
Detection of complexes is valuable in the diagnosis of bacterial endocarditis. In most instances, complement activation seems likely to be responsible for the inflammatory changes that occur, with chemotaxis of neutrophils and release of lysosomal enzymes as the prime factors involved [13].
Immunobiological Detection Methods That Require Specialized Laboratory Facilities
- Electron –microscopic demonstration of complexes in tissues, such as those found in the liver of patients with hepatitis B virus infections. Precipitations of complexes in the cold, cryoprecipitation, and subsequent identification of microbial antigens e.g., hepatitis B antigens [14].
- Detection of bound complement component (e.g., Clq) in the complexes, often after precipitation by polyethylene glycol. The principle of the assay is that the naturally bound Clq is then added, followed by polyethylene glycol to precipitate the complexes. The Clq remaining in the supernatant is then measured, allowing the estimation of the bound Clq. A similar test commercially available involves the binding of bovine conglutinin to the bound complement [15].
- Immunobiological tests such as aggregation of platelets and inhibition of antibody – mediated cytotoxicity. The later test is quite widely used and involves inhibition of the killing by non-sensitized lymphocytes of target cells (e.g., chang cells, a line of human liver cells) coated with antibody. If immune complexes are added to the lymphocytes, their Fc receptors are blocked by the antibody in the complexes so that the receptors cannot bind the antibody on the target cell [16].
- Immunoblotting technique or Western blotting, is a powerful method by which macromolecules, usually proteins, are separated by polyacrylamide gel electrophoresis (PAGE) and then transferred electrophoretically to a nitrocellulose membrane. It has largely superseded the traditional immunoelectrophoresis techniques and is used in all areas of immunological research and diagnostic serology. Immunoblot analysis is a valuable confirmatory test for HIV antibodies and its use is being extended to the detection of many hospital pathogens [17].
- Laser based flow cytometry which measures forward angle light scatter that is related to the size of cells being measured is increasingly used in immunology for the identification of cell populations (phenotyping) and for separation (sorting) on the basis of staining patterns with fluorescent ligands [18].
- The polymerase chain reaction (PCR) is used for the direct detection of nucleic acids- i.e. DNA and RNA. It is particularly useful for the detection of viruses that are difficult to identify by conventional methods. The major requirement is that at least, part of the sequence of the nucleic acid of the agent to be detected is known. In essence, the technique as an in vitro technique for nucleic acid amplification specially applied to a particular segment of DNA [19].
Two synthetic oligonucleotide primers are required that will hybridize to the ends of opposite strands of the target sequence. The process is cyclical, involving three stages:
- Denaturation of target DNA by heating at 91- 95 oC.
- Cooling to 37 – 50 oC at which point the primers anneal to the target DNA strands and,
- Copying of the DNA and extension of the primers by means of a polymerase (Taq polymerase from Thermus aquaticus – a thermophilic bacterium). From 25 to 35 cycles can lead to a million-fold increase of the target DNA. The table below lists some of the widely used tests in clinical immunology [20].
Clinical Immunology Tests
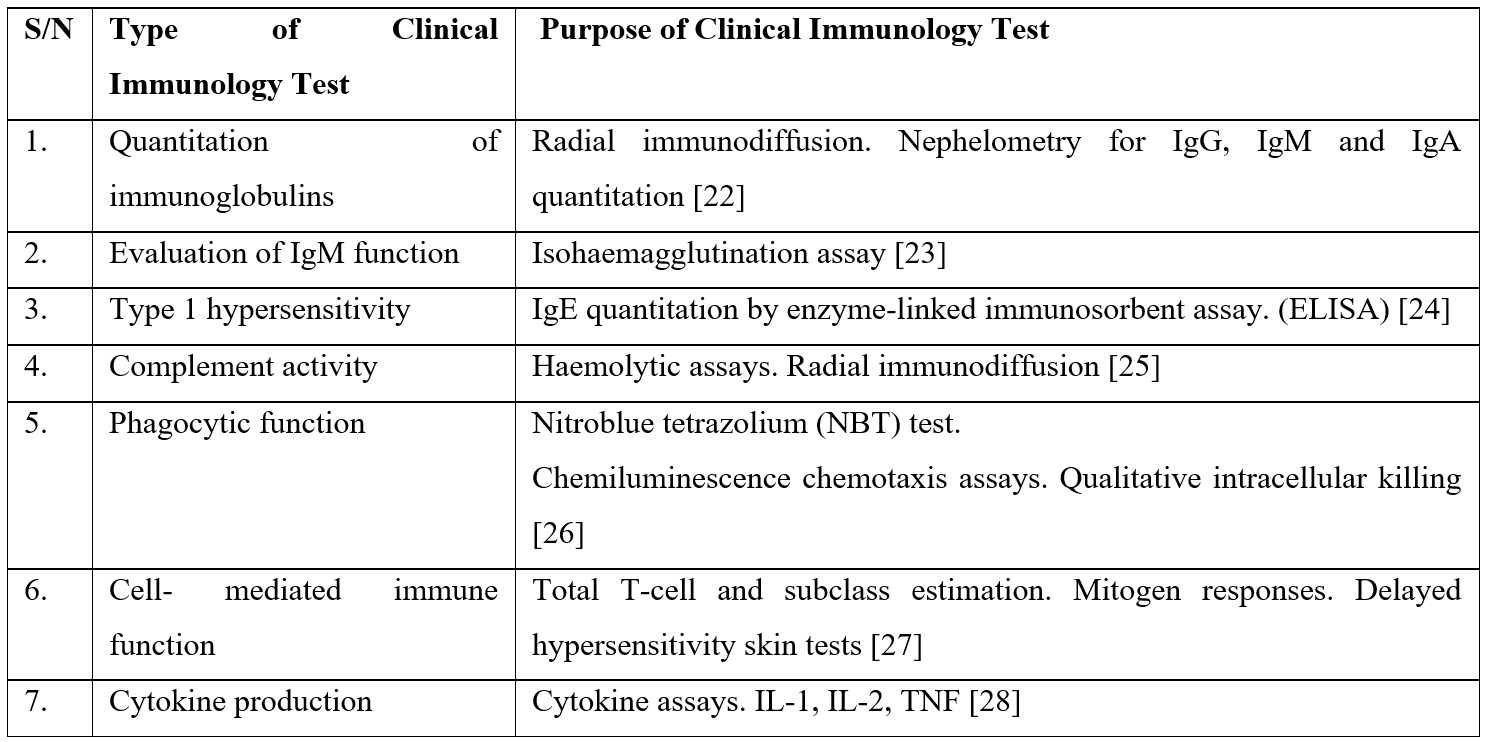
The ELISA assay has wide applications. Assays of specific IgM may be helpful in atypical measles or mumps and in certain arbovirus infections. Electron –microscopic examination is widely used in biopsy materials as well as the fluorescent antibody technique [21,29].
Laser nephelometry is the measurement of light scattered from a transmitted light source. It is used for the determination of antigens by adding constant amounts of highly purified optically clear specific antibody to varying amounts of antigen. Monoclonal antibodies are widely available for the detection of cellular and soluble antigens with enzyme linked assays and immunofluorescence [1-3].
Biotin-avidin techniques are being increasingly used in immunohistochemistry. Avidin is a glycoprotein from egg albumin, has a very high affinity for the vitamin biotin. Biotin is coupled to antibody covalently and interaction of the antibody with its antigen is demonstrated using fluorochrome – labelled avidin. The procedure can be used in the same way as in direct fluorescent antibody tests. Most of these procedures require specialized laboratory facilities not generally available in the routine clinical pathology laboratory [4].
Applications of Monoclonal Antibodies
The applications of monoclonal antibodies in clinical diagnostic immunology are listed below:
- Lymphocyte subset and leucocyte determination.
- Detection of HLA antigens.
- Detection of viruses including typing.
- Microbial and parasite antigen detection.
- RIA for polypeptide hormones.
- Typing of leukaemias and lymphomas.
- Detection of tumor antigens [5].
Conclusion
Some other clinical applications of diagnostic immunology are shown below:
(A) Quantitation of Serum Immunoglobulin Levels
- Patients with severe or repeated infection, e.g. actinomycosis, subacute bacterial endocarditis, and infectious mononucleosis.
- Liver disease.
- To monitor immunotherapy of patients with immune-proliferative disorders e.g., monoclonal gammopathies of IgG, IgA or IgM.
- To distinguish transient changes, such as those following burns and in primary immunodeficiencies.
- Estimation of immune responses following natural infection or immunization- IgA levels in patients with infections of mucosal surfaces or IgE levels in patients with allergies.
- Rise in levels of antibodies in cerebrospinal fluids of patients with infections or in demyelinating diseases.
- To detect free heavy or light chains of immunoglobulins in the urine of patuients with multiple myeloma [6].
(B) Detection of Levels of C Reactive Proteins
This is used to follow the progress of treatment for an infection [7].
(C) Detection and Autoantibodies
Using immunofluorescence in tissue sections, thyroid sections for antithyroid antibodies, commercial assay kits for rheumatoid arthritis, and an antinuclear factor in systemic lupus erythematosus [8].
(D) Detection Of Immune Complexes in Type III Hypersensitivity States
Many methods are available – cryoprecipitation, precipitation by polyethylene glycol, and detection of complement, if it is bound to the complexes. Unfortunately, the results tend to be variable and difficult to interpret. It is valuable in bacterial endocarditis [9].
(E) Skin Tests for Type 1 And Type IV Hypersensitivity States
There are various forms of the skin test.
- Intradermal injection of dilute antigen (allergen).
- Prick tests, in which test material is placed in absorbent materials and placed on the skin- particularly used for type IV hypersensitivity contact dermatitis [10].
(F) Estimation of Complement Components
The most common procedure in the past was to measure total complement levels, but individual components can be measured more conveniently with commercially available immunodiffusion plates [11].
(G) Tests of Lymphocyte Function
- Lymphocyte transformation test: used for in vitro test of cell- mediated immunity in suspected immunodeficiency.
- Macrophage (leucocyte) migration inhibition test: This is less commonly used than the transformation test alone [12].
(H) Test of Phagocyte Function
For suspected chronic granulomatous disease in patients in unresolving infections, this test is used for the detection of:
- Intracellular enzyme activity - the ability to reduce the dye nitroblue tetrazolium (NBT) as an indicator of the activity of oxygen –dependent bactericidal activities [13].
- Phagocytosis – the ability to injest inert particles (yeast or latex), opsonized red cells or bacteria to test for Fc receptor function [14].
- Chemotaxis- ability to be attracted by a chemoattractant through a membrane filter [15].
- Chemiluminescence – emission of light by phagocytes as a test for their ability to be activated [16].
Author Contributions:
P1A: Concept and design of the study, reviewed the literature, manuscript preparation, critical revision of the manuscript, collected data and review of study.
COA, AOO, LCA, NCA, MRTP: Conceptualized study, literature search, prepared first draft of manuscript and critical revision of the manuscript.
Work Attributed To:
- Immunology and Vaccination Research Group, Philip Nelson Institute of Medical Research, Lagos, Nigeria.
- TB/HIV/AIDS Research Group, Michael and Cecilia Ibru University, Agbarha Otor, Ughelli, Delta State, Nigeria.
- Department of Medicine, University of Sao Paulo, Brazil.
- Department of Microbiology, Imo state University, Imo state, Nigeria.
Sources of Funding: None.
Acknowledgement: We wish to express our thanks to Dr. Juan Bueno Gabriel Sanchez MD of Fundacion Centro De Investigacion De La Biodiversidad Biolabb, Bogota, Colombia for his active interest and cooperation in this work and also, we give many thanks to God Almighty for his support.
Conflict of Interest: None
References
- Cavallaro JJ, Palmer DF, Bigazzi BE. Immunofluorescence detection of autoimmune disease. Immunol. Ser. no. 7. Center for Disease Control, Atlanta, 1976.
- Food and Drug Administration. Test for hepatitis B surface antigen. Fed. Regist, 1975; 40: 29706-29712.
- Fulford KM, Taylor RN, Przbyszewski VA. Reference preparation to standardize results of serological test for rheumatoid factor. J. Clin. Microbiol, 1978; 434-441.
- Griffin CW, Taylor RN. Proficiency testing-is it worthwhile? (editorial) Clin. Microbiol. Newsl, 1979; 1: 4-5.
- Kaplan EJ, Anthony BF, Chapman SS, Ayoub EM, Wannamaker LW. The influence of the site of infection on the immune response to group A streptococci. J. Clin. Invest, 1970; 49: 1405-1414.
- Klein GC. Immune response to streptococcal infection. In N. R. Rose and H. Friedman (ed.), Manual of clinical immunology. American Society for Microbiology, Washington, D.C., 1976; 264-273.
- Klein, G. C., and W. L. Jones. 1971. Comparison of streptozyme test with the antistreptolysin O, antideoxyribonuclease B, and antihyaluronidase tests. Appl. Microbiol, 1971; 2:157-259.
- Palmer DF, Herrmann KL, Cavallaro JJ. Modified rubella hemagglutination-inhibition test, In Palmer DF, Cavallaro JJ, Herrmann K, Stewart JA, Walls KW (ed.), Serodiagnosis of: toxoplasmosis, rubella, cytomegalic inclusion disease, and herpes simplex. Center for Disease Control, Atlanta, 1974; 57-83974.
- Palmer DF, Herrmann KL, Lincoln RE, Hearn MV, Fuller JM. Standardized rubella hemagglutination-inhibition tests. Immunol. Ser. no. 2. Procedural guide. Center for Disease Control, Atlanta, 1970.
- Pope V, Larsen SA, Taylor RN. Proficiency testing summary analysis. Syphilis serology III. Center for Disease Control, Atlanta, 1979.
- Pope V, Larsen SA, Taylor RN. Proficiency testing summary analysis. Syphilis serology IV. Center for Disease Control, Atlanta, 1980.
- Pope V, Larsen SA, Taylor RN, Feeley JC. Proficiency testing summary analysis. Syphilis serology I. Center for Disease Control, Atlanta, 1979.
- Pope V, Larsen SA, Taylor RN, Feeley JC. Proficiency testing summary analysis. Syphilis serology II. Center for Disease Control, Atlanta, 1979.
- Pope V, Taylor RN, Larsen SA, Feeley JC. Proficiency testing summary analysis. WHO and PAHO laboratories? Syphilis serology. Center for Disease Control, Atlanta, 1979.
- Taylor RN, Ehrhard H, Marcus S. Evaluation of tests for infectious mononucleosis through proficiency testing. Health Lab. Sci, 1976; 13: 34-44.
- Taylor RN, Fulford KM, Huong AY. Comparison of kinetic and end-point diffusion methods for quantitating human serum immunoglobulin. J. Clin. Microbiol, 1978; 8: 23-27.
- Taylor RN, Fulford KM, Jones WL. Reduction of variation in results of rheumatoid factor tests by use of a serum reference preparation. J. Clin. Microbiol, 1977; 5: 42-45.
- Taylor RN, Fulford KM, Przybyszewski VA. Proficiency testing summary analysis. Diagnostic immunology. I. Hepatitis B. Center for Disease Control, Atlanta, 1979.
- Taylor RN, Fulford KM, Przybyszewski VA. Proficiency testing summary analysis. Diagnostic immunology. II. Hepatitis B. Center for Disease Control, Atlanta, 1979.
- Taylor RN, Fulford KM, Przybyszewski VA. Proficiency testing summary analysis. Diagnostic immunology. I. Center for Disease Control, Atlanta, 1977.
- Taylor RN, Fulford KM, Przybyszewski VA. Proficiency testing summary analysis. Diagnostic immunology 1979. II. Center for Disease Control, Atlanta, 1979.
- Taylor RN, Fulford KM, Przybyszewski VA. Proficiency testing summary analysis. Diagnostic immunology. III. Center for Disease Control, Atlanta, 1979.
- Taylor RN, Fulford KM, Przybyszewski VA. Proficiency testing critique. Diagnostic immunology. Center for Disease Control, Atlanta, 1979.
- Taylor RN, Fulford KM, Przybyszewski VA. Proficiency testing critique. Diagnostic immunology, Center for Disease Control, Atlanta, 1980.
- Taylor RN, Fulford KM, Przybyszewski VA, Pope V. Center for Disease Control Diagnostic Immunology Proficiency Testing Program results for 1976. J. Clin. Microbiol, 1977; 6: 224-232.
- Taylor RN, Fulford KM, Przybyszewski VA, Pope V. Center for Disease Control Diagnostic Immunology Proficiency Testing Program results for 1977. J. Clin. Microbiol, 1978; 8: 388-395.
- Taylor RN, Fulford KM, Pryzybyszewski VA, Pope V. Center for Disease Control Diagnostic Immunology Proficiency Testing Program results for 1978. J. Clin. Microbiol, 1979; 10: 805-814.
- Taylor RN, Huong AY, Fulford KM, Przybyszewski VA, Hearn TL. Quality control for immunologic tests. DHEW Publ. no. (CDC) 1979; 79- 8376. Center for Disease Control, Atlanta.
- U.S. Department of Health, Education, and Welfare. Serology evaluation and research assembly 1956-1957. Public Health Service Publ. no. 650. Bureau of State Services, Communicable Disease Center, Atlanta.

