Work Ability in Patients with COPD: Sick Leave Frequency and Duration
Minov J*, Stoleski S, Mijakoski D, Atanasovska A, Panajotovic Radevska M and Bislimovska D
1Institute for Occupational Health of RN Macedonia, Skopje, Balkans
2Medical Faculty, Ss Cyril and Methodius University in Skopje, RN Macedonia, Balkans
Received Date: 04/09/2023; Published Date: 08/02/2024
*Corresponding author: Minov Jordan, Institute for Occupational Health of RN Macedonia, Medical Faculty, Ss Cyril and Methodius University in Skopje, RN Macedonia, Balkans
Abstract
Introduction: Findings of several studies indicated that chronic obstructive pulmonary disease (COPD) affects patients’ work ability and everyday life activities.
Aim of the study: To compare frequency and duration of absence from work in workers with COPD and non-COPD controls.
Methods: We performed a cross-sectional study including 114 workers with COPD (63 males and 51 females, mean age 53.2 ± 3.7) and an equal number of non-COPD controls (60 males and 54 females, mean age 52.7 ± 3.1), classified by skill level in four occupation groups. Evaluation of the study subjects consisted of completion of a questionnaire, baseline spirometry, and bronchodilator reversibility testing.
Results: Frequency of the sick leave episodes was significantly higher in workers with COPD than in non-COPD controls (44.7% vs. 20.1%; P = 0.004). In addition, frequency of sick leave episodes was higher in all occupation groups of workers with COPD than in non-COPD controls with significant difference for the workers performing physical or manual tasks (48.3% vs. 21.2%; P = 0.045). In regard to duration of sick leave episodes, the frequency of episodes lasting equal or less than 15 days and more than 15 days was higher in workers with COPD being significantly higher for episodes longer than 15 days (50.9% vs. 26.9%; P = 0.045).
Conclusion: Our findings indicated significantly higher frequency of sick leave episodes, as well as significantly higher frequency of sick leave episodes lasting more than 15 days, in workers with COPD than in non-COPD controls.
Keywords: Absence from work; Occupation; Questionnaire; Spirometry; Worker
Introduction
COPD remains one of the most important public health problems in the modern world due to its substantial impact to all aspects of the life of the patients, as well as to their families and to the whole society. Research in COPD has expanded rapidly in the last decades primarily aimed to unravel the pathobiology, to find noninvasive biomarkers that indicate the presence and severity of inflammation and oxidative stress, and to analyze shirt- and long-term efficacy of therapeutic interventions. On the other side, there is a lack of information about the economic burden of COPD contributing to the insufficient attention that governments and policy makers pay to this chronic condition. According to the National Heart, Lung, and Blood Institute (NHLBI), the costs of COPD and asthma in the United States (US) in 2008 totaled 68 billion US dollars (USD), of which 53.7 USD were direct costs, i.e., costs that included costs for inpatient care, physician services, prescription drugs, home health care and nursing home care. COPD exacerbations accounted for up to 75% of these direct health care expenditures. In addition, indirect costs, i.e. the costs including lost wages of the patient, lost wages of family caregivers and employer-borne costs (absenteeism and sick leave, disability and impaired work performance), accounted for a significant proportion of disease’s burden [1-3].
Results from the review of Patel et al. indicated that 13-18% of patients with COPD were limited in the amount or type of work they could do and one-third or more experienced general activity limitation [4]. Furthermore, results from a few studies indicated that patients with COPD had a 10-fold higher risk of work disability than members of the general population, as well as that COPD was associated with greater disability than other chronic health conditions, such as diabetes or heart disease [5]. On the other hand, the evidence for COPD-related work absence is still not sufficient. The aim of the present study was to explore work absence, i.e., the frequency and duration of sick leave episodes, in workers with COPD.
Methods
Study design and setting
A cross-sectional study (study of prevalence) was performed at the Institute for Occupational Health of RN Macedonia, Skopje, in the period September 2022 - June 2023. For the aim of the study, self-reported frequency of sick leave episodes, as well as of sick leave episodes lasting more than 15 days, in the past 12 months were compared between a group of workers with COPD and a group of non-COPD workers.
Study population
Study population included 228 workers recruited during their preventive check-ups in the mentioned period at the Institute for Occupational Health of RN Macedonia, Skopje, divided in two groups.
The first group included 114 workers with COPD diagnosed by physician to whom proper therapy has been prescribed.
The second group included an equal number of non-COPD controls, i.e. workers in whom COPD was excluded, matched to the workers from the first group by sex, age and occupation classified by required skill level.
All study subjects were informed about study and their written consent was obtained.
Study protocol
Study protocol included completion of a questionnaire and lung function measures.
An interview-led questionnaire was consisted of four parts.
The first part included questions regarding demography of the study subjects (sex, age, level of education, and smoking status). Smoking status (active smoker, ex-smoker, and non-smoker) was defined by the World Health Organization (WHO) criteria [6].
The second part of the questionnaire included questions about occupation and work characteristics of the study subjects. Occupations were classified in four groups following the International Standard Classification of Occupations (ISCO-08) based on the skill level, i.e., on the ability to carry out the tasks and duties of a given job. Occupations at Skill Level 1 (Group 1) involved the performance of simple and routine physical or manual tasks (cleaning, digging, lifting and carrying materials, etc.). Skill Level 2 (Group 2) involved the performance of tasks such as operating machinery and electronic equipment, maintenance and repair of machinery and electronic equipment, driving vehicles, etc. (bus drivers, butchers, dressmakers, hairdressers, etc.), while occupations at Skill Level 3 (Group 3) involved the performance of complex technical and practical tasks requiring an extensive body of factual, technical and procedural knowledge in a specialized field (shop managers, computer support technicians, commercial sales representatives, etc.). Occupations at Skill Level 4 (Group 4) involved the performance of tasks that require complex problem-solving, decision-making and creativity based on an extensive body of theoretical and factual knowledge in a specialized field (sales and marketing managers, medical practitioners, computer systems analysts, etc.) [7].
The third part of the questionnaires included questions on chronic diseases of the study subjects diagnosed by physician and their treatment.
The fourth part of the questionnaire included questions on the sick leaves in the past 12 months. Sick leave was defined as absence of work for more than two consecutive days not caused by injury [8]. Based on the sick leave duration, study subjects were classified in two groups: ones with sick leave lasting less and more than 15 days. In addition, study subjects with sick leave episode in the past 12 months were classified by the condition leading to work absence (lung disease, cardiometabolic disease, osteomuscular disease, gastrointestinal disease and other condition).
Lung function measurements included baseline (pre-bronchodilator) spirometry which was performed in all study subjects and post-bronchodilator spirometry, which was performed in subjects with value of the ratio between Forced Expiratory Volume in 1 second (FEV1) and Forced Vital Capacity (FVC) less than 0.70.
The baseline spirometry, including measures of FVC, FEV1, FEV1/FVC, and maximal expiratory flow at 75%, 50%, 25%, and 25-75% of FVC (MEF75, MEF50, MEF25, and MEF25-75, respectively), was performed by spirometer Ganshorn SanoScope LF8 (Ganshorn Medizin Electronic GmbH, Germany) with recording the best result from three measurements the values of FEV1 of which were within 5% of each other. The results of spirometry were expressed as percentages of the predicted values according to the actual recommendations of ERS and ATS. The post-bronchodilator spirometry was performed according to the actual recommendations, i.e., spirometric measurements were performed 20 minutes after administration of 400 mg salbutamol by metered dose inhaler through spacer. Fixed airflow narrowing characteristic for COPD was considered if post-bronchodilator FEV1/FVC remained less than 0.70. In addition, based on the post-bronchodilator FEV1 value, i.e. on the airway limitation severity, COPD was classified as mild, moderate, severe and very severe (GOLD 1-4) [9- 11].
Statistical analysis
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 11.0 for Windows. Continuous variables were expressed as mean values with Standard Deviation (SD), and the nominal variables as numbers and percentages. Due to the aim of the study for analyses of the data we used univariate statistical models for testing the differences in prevalence and comparison of the means. Study variables were checked for normality by the Kolmogorov–Smirnov and Shapiro–Wilk W tests, and normal data distribution was detected. Chi-square test (or Fisher’s exact test where appropriate) was used for testing difference in the prevalence. Comparison of spirometric measurements was performed by independent-samples T-test. A P-value less than 0.05 was considered as statistically significant.
Results
Table 1 is shown the demographic and other characteristics of the study subjects.
Table 1: Characteristics of the study subjects.
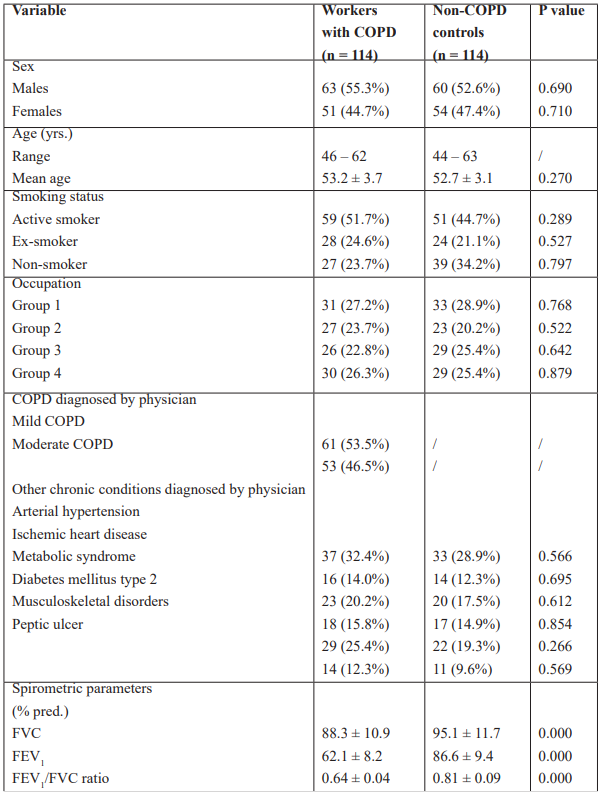
COPD: chronic obstructive pulmonary disease; FEV1: forced expiratory volume in 1 second; FVC: forced vital capacity; % pred.: % of the predicted value; yrs: years.
Difference between self-reported sick leave episodes frequency in the past 12 months in workers with COPD (51/114) and non-COPD controls (23/114) was statistically significant (44.7% vs. 20.1%; P = 0.004) (Figure 1). Two episodes of sick leave were reported by 7 workers with COPD (6.1%), whereas in the non-COPD controls no one worker reported more than one episode of sick leave in the past 12 months.
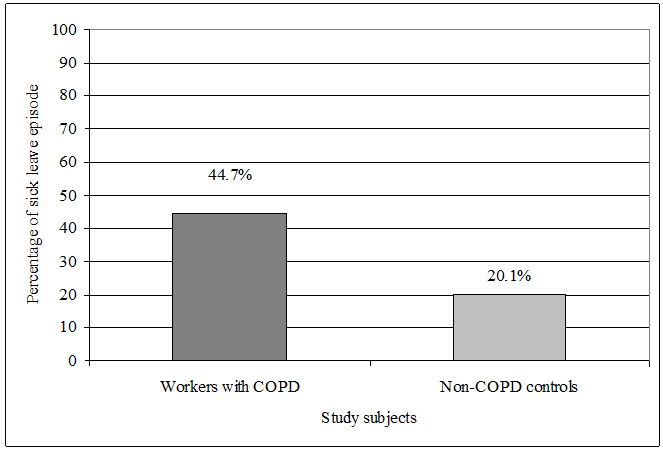
Figure 1: Frequency of the sick leave episodes in workers with COPD and non-COPD controls.
There was not significant difference between males and females in regard to the frequency of the sick leave episodes in both workers with COPD and non-COPD controls (28/63 44.4% vs. 23/51 45.1%; P = 0.965, and 13/60 21.7% vs. 10/54 18.7%; P = 0.733, respectively). The frequency of sick leave episodes was significantly higher in both males and females with COPD than its frequency in non-COPD males and females (28/63 44.4% vs. 13/60 21.7%; P = 0.046, and 23/51 45.1% vs. 10/54 18.7%; P = 0.034, respectively) (Figure 2).
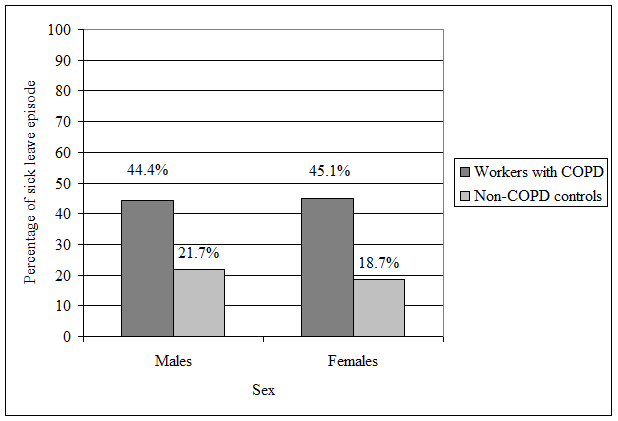
Figure 2: Sex distribution of sick leave episodes in workers with COPD and non-COPD controls.
Frequency of sick leave episodes was higher among workers with moderate COPD (29/51; 56.8%) than in the workers with mild COPD (22/51; 43.2%) but the difference was not statistically significant (P = 0.423) (Figure 3).

Figure 3: Sick leave episodes frequency in workers with mild and moderate COPD.
The highest frequency of sick leave episodes in workers with COPD was registered in the Group 1 with no significant difference between other occupation groups. In addition, the frequency of sick leave episodes in non-COPD controls was also similar in all occupation groups. Significantly higher difference of sick leave episodes between workers with COPD and non-COPD controls was found in the Group1 (Table 2).
Table 2: Sick leave episodes frequency in workers with COPD and non-COPD controls classified by occupation group.

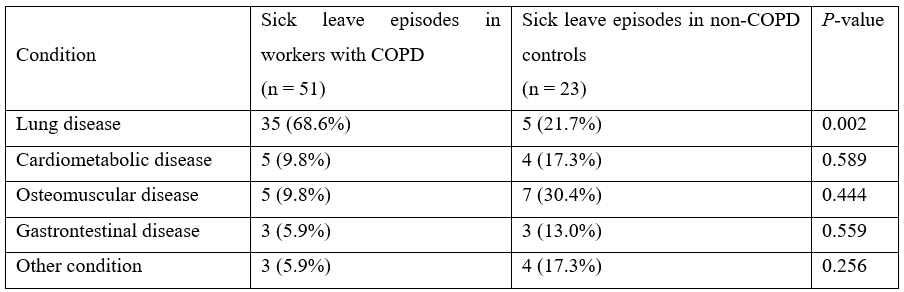
Regarding the condition leading to absence from work, respiratory symptoms, i.e., lung disease, was the frequent cause in workers with COPD, following by cardiometabolic and osteomuscular disease, gastrointestinal disease, and other condition. In the group of non-COPD workers, the most frequent condition leading to sick leave was osteomuscular disease, following by lung disease, cardiometabolic disease, other condition and gastrointestinal disease (Table 3).
Table 3: Conditions leading to work absence in workers with COPD and non-COPD controls.
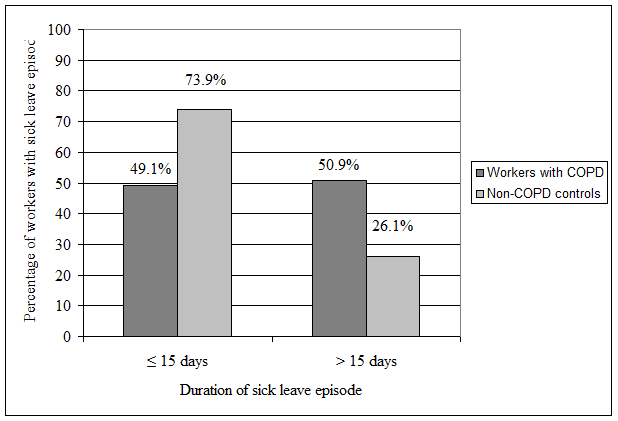
Frequency of sick leave episodes lasting equal or less than 15 days was higher than frequency of sick leave episodes lasting more than 15 days in both workers with COPD and non-COPD controls (50.9% vs. 49.1%, and 73.9% vs. 26.1%, respectively) with statistical significance registered for non-COPD controls (P =0.048). Frequency of sick leave episodes lasting more than 15 days was non-significantly higher in workers with COPD (26/51; 50.9%) than in non-COPD controls (6/23; 26.1%) (P = 0.045) (Figure 4).
Figure 4: Frequency of sick leave episodes by their duration.
Discussion
Although COPD is often considered as a disease of the elderly, a substantial proportion of patients with COPD are at working age, i.e., younger than 65 years, and the disease significantly affects their work ability leading to absence from work or premature retirement [12,13]. Sickness absence is not a simple function of ill health and also includes psychosocial factors and coping behaviors it is a valuable measure to assess the impact of respiratory complaints or other possible predictors of a worker’s capacity. In addition, workers with COPD reported that issues affecting their work ability included work worsening their COPD, problems getting to work, and superiors making negative comments about their disease and not taking it into consideration enough [14]. In a survey of nearly 2,500 patients in Brazil, China, Germany, Turkey, the United States, and the United Kingdom, aged 45–67 years, nearly 40% had retired prematurely because of COPD at an average age of 54 years [15]. As well as leading to stopping working, COPD leads to increased absenteeism and presenteeism (poor work performance when at work) [16,17]. Results of the Confronting COPD survey indicated that more than a third of COPD patients reported that their condition kept them off from working, limited their ability for work or had caused them working time loss in the past year [18,19]. People with COPD are approximately twice as likely to have a short-term disability and more than four times as likely to have long-term disability [20]. In a recent systematic review including 183 studies published in the last 10 years, Rojanasarot et al. indicated that the most common conditions leading to productivity loss and absenteeism was pain due to osteomuscular disorder, followed by cancer, chronic lung disease, cardiometabolic disease, and depression [21].
In the present study we investigated the impact of COPD on work ability of the patients by comparison of frequency and duration of sick leave episodes in workers with COPD and non-COPD controls matched by sex, age and occupation classified by required skill level. Study subjects of examined groups had similar demographic characteristics. The most common comorbidities in workers with COPD were cardiometabolic, musculoskeletal, and gastrointestinal disorders. These disorders were also the most common chronic conditions in non-COPD controls. In both groups there were a large proportion of active smokers indicating poor results of anti-smoking activities that is similar to findings from our previous studies [22,23].
We found significantly higher frequency of sick leave episodes in workers with COPD than in non-COPD controls, i.e., their frequency in workers with COPD was more than twofold higher. Frequency of sick leave episodes in males and females within both examined groups was similar. In addition, frequency of sick leave episodes in both males and females with COPD was significantly higher than its frequency in males and females without COPD. The studies examining the effect of COPD on employment and work productivity are not always consistent and have been conducted in a variety of settings and populations. Similarly, to our findings, results of the study conducted by Rennard et al. including more than 3,000 patients with COPD from nine countries in Europe and North America indicated absence from work in the past year due their disease in 35.7% of them [18]. On the other hand, in a Greek study investigating the disease burden of COPD, almost one-fourth of the participants reported that they had missed work during the past 12 months due to their respiratory symptoms [24].
Despite some studies showed work absence increase related to higher stages of COPD, we found similar frequency of sick leave episodes in workers with mild and moderate COPD [25]. In the present study were not included patients with severe and very severe COPD as according to the actual national legislative these patients are not able for work, i.e., they should be prematurely retired [26,27].
Effects of certain work activities and work exposures on the course of COPD were indicated in a number of studies [8,28,29]. Frequency of sick leave episodes in all occupation groups of workers with COPD was higher than its frequency in occupation groups of non-COPD controls with statistically significant difference for the Group 1. Similar results, i.e., more frequent and more prolonged absence from work due to respiratory disorder (COPD or asthma) in blue collar workers than in white collar workers, were indicated in the longitudinal study conducted by Alexopoulos and Burdorf. Furthermore, they indicated that workers with absence due their chronic lung condition were at higher risk of subsequent sickness absence in the next year [30].
Around two-thirds of all sick leave episodes in workers with COPD were due to respiratory complaints (vs. 21.7% in non-COPD workers), while one-third of them were related to their comorbidities. As it was mentioned earlier, it was estimated that exacerbations of COPD, i.e., the acute worsenings of respiratory symptoms, accounted for up to 75% of the direct costs related to COPD [3].
We found significantly higher frequency of sick leave episodes lasting more than 15 days in workers with COPD than in non-COPD controls, i.e., in around a half of the workers with COPD and in around a quarter of the non-COPD controls the sick leave episodes lasted more than 15 days. Findings from other studies that investigated the duration of work absence are somewhat inconsistent. Results from the Greek study mentioned above indicated 10 days as a mean duration of work absence per year. According to the results of the population-based study conducted by Dierick et al., the number of days of the work absence per year was lower in workers with asthma than in workers with COPD (median: 15 days vs. 39 days). In a Swedish retrospective cohort study that included more than 17,000 patients with COPD, Lisspers et al. registered a significant higher mean number of sick days in COPD patients (44.3 days) compared with the sex- and age-matched reference population (30.4 days) [31]. In addition, in their review of the economic burden of COPD on employers and individuals in the United States, Patel et al. estimated the mean duration of sick leave episodes per year in workers with COPD in the range from 1.3 to 19.4 days [4].
Findings of the present study have to be interpreted in the context of its limitations. Cross-sectional analysis based on self-report survey not on objective data collected through health records could have implication on the results obtained and their interpretation. In addition, classification of occupations was based on the skill level required for a given job, not on the workplace exposure, so the impact of certain workplace exposure on the frequency and duration of sick leave episodes could not be assessed. Nevertheless, besides these limitations the present study contributes to the knowledge about impact of COPD on work ability, the aspect of the disease that is still understudied.
Conclusion
In a cross-sectional study investigating the impact of COPD on work ability we found significantly higher frequency and significantly higher duration of sick leave episodes in workers with COPD than in non-COPD controls. Ours findings indicated a need of improvement of the measures of primary and secondary prevention at the workplace in order to maintain work ability of the patients with COPD for as long as possible.
Competing Interests: All authors hereby have declared that no competing interests exist.
Authors Participation: JM and SS participated in data collection, data analysis, and writing all versions of the manuscript. DM, AA, MPR, and DB participated in data collection. All authors read and approved the final version of the manuscript.
References
- Chen S, Kuhn M, Prettner K, et al. The global economic burden of chronic obstructive pulmonary disease for 204 countries and territories in 2020-50: a health-augmented macroeconomic modeling study. Lancet Glob Health, 2023; 11: e1183-1193.
- National Heart, Lung, and Blood Institute. Morbidity and Mortality: 2012 Chart Book on Cardiovascular, Lung and Blood Diseases. Bethesda: National Institute of Health, 2012.
- Toy EL, Galagher TF, Stanley EL, et al. The economic impact of exacerbations of chronic obstructive pulmonary disease and exacerbation definition: a review. COPD, 2010; 7(3): 214-228.
- Patel JG, Nagar SP, Dalal AA. Indirect costs in chronic obstructive pulmonary disease: a review of economic burden on employers and individuals in the United States. Int J Chron Obstruct Pulmon Dis, 2014; 9: 289-300.
- Eisner MD, Iribarren C, Blanc PD, et al. Development of disability in chronic obstructive pulmonary disease: beyond lung function. Thorax, 2011; 66: 108-114.
- World Health Organization. Guidelines for controlling and monitoring the tobbaco epidemic. Geneva: WHO, 1998.
- International Standard Classification of Occupations – ISCO-08/International Labour Office. Geneva: ILO, 2012.
- Boot CRL, Vercoulen JHMM, van der Gulden JWJ, et al. Sick leave in patients with obstructive lung disease is related to psychosocial and work variables rather than to FEV1. Respiratory Medicine, 2005; 99: 1022-1031.
- Pellegrino R, Viegi G, Brusasco V, et al. Interpretative strategies for lung function tests. Eur Respir J 2005; 26(5): 948-968.
- Culver BH, Graham BL, Coates AL, et al. Recommendations for Standardized Pulmonary Function Report. An Official American Thoracic Society Technical Statement. Am J Respir Crit Care Med, 2017; 196(11): 1463-1472.
- Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease, 2023.
- Minov J, Stoleski S. Chronic obstructive airways diseases: Where are we now? Open Respir Med J, 2015; 9 (1): 37-38.
- Halpin D. Chronic obstructive pulmonary disease and work: Is it time to stop? Am J Respir Crit Care Med, 2019; 200: 1195-1207.
- Kremer AM, Pal TM, van Keimpema AR. Employment and disability for work in patients with COPD: a cross-sectional study among Dutch patients. Int Arch Occup Environ Health, 2006; 80: 78–86.
- Fletcher MJ, Upton J, Taylor-Fishwick J, et al. COPD uncovered: an international survey on the impact of chronic obstructive pulmonary disease [COPD] on a working age population. BMC Public Health, 2011; 11: 612.
- Rai KK, Adab P, Ayres JG, Jordan RE. Systematic review: chronic obstructive pulmonary disease and work-related outcomes. Occup Med, 2018; 68: 99–108.
- Holden L, Scuffham PA, Hilton MF, et al. Which health conditions impact on productivity in working Australians? J Occup Environ Med, 2011; 53: 253–257.
- Rennard S, Decramer M, Calverley PMA, et al. Impact of COPD in North America and Europein 2000: subjects’ perspective of confronting COPD international survey. Eur Respir J, 2002; 20: 799-805.
- Britton M. The burden of COPD in the UK: results from the confronting COPD survey. Respir Med, 2003; 97: S71–S79.
- Darkow T, Kadlubek PJ, Shah H, Phillips AL, Marton JP. A retrospective analysis of disability and its related costs among employees with chronic obstructive pulmonary disease. J Occup Environ Med, 2007; 49: 22–30.
- Rojanasarot S, Bhattacharyya SK, Edwards N. Productivity loss and productivity loss costs to United States employers due to priority conditions: a systematic review. Journal of Medical Economics, 2023; 26(1): 262-270.
- Minov J, Karadzinska-Bislimovska J, Nelovska Z, et al. Smoking among Macedonian workers five years after anti-smoking campaign. Arh Hig Rada Toksikol, 2012; 63: 207-213.
- Minov J, Stoleski S, Stikova E, et al. COPD in a sample of general adult population from the Skopje region. Acad Med J, 2022; 2(1): 47-58.
- Kourlaba GG, Hillas G, Vassilakipoulos T, Maniadakis N. The disease burden of chronic obstructive pulmonary disease in Greece. Int J Chron Obstr Pulm Dis, 2016; 11: 2179–2189.
- Wacker ME. Direct and indirect costs of COPD and its comorbidities: results from the German COSYCONET study. Respir Med, 2016; 111: 39–46.
- Law on Pension and Disability Insurance, 2023.
- Rulebook on the organization, composition and way of working of the Commission for the assessment of work ability, 2023.
- Dierick BJH, Flokstra-de Blok BMJ, van der Molen T, et al. Work absence in patinets with asthma or/and COPD: a population-based study. Primary Care Respiratory Medicine, 2021; 31: 9.
- Minov J. Occupational chronic obstructive pulmonary disorder: prevalence and prevention. Expert Review of Respiratory Medicine, DOI: 10.1080/17476348.2021.2011722.
- Alexopoulos EC, Burdorf A. Prognostic factors for respiratory sickness absence and return to work among blue collar workers and office personnel. Occup Environ Med, 2001; 58: 246–252.
- Lisspers KK, Larsson K, Johansson G, et al. Economic burden of COPD in a swedish cohort: the ARCTIC study. Int J Chron Obstr Pulm Dis, 2018; 13: 275–285.

