Auditing of Contraception used in Ashmoun-Menoufia, Egypt
Elkotb Hassan Elkotb, Ayman Elsayed El Ashmawy, Rehab Belal Mohamed and Mohamed Zaeim Hafez*
1Obstetrics and Gynecology department, Faculty of Medicine, Al Azhar University (Assuit), Egypt
2Physiology department, Faculty of Medicine, Al Azhar University (Assuit), Egypt
Received Date: 07/09/2023; Published Date: 07/02/2024
*Corresponding author: Dr. Mohamed Zaeim, Obstetrics and Gynecology Department, Faculty of Medicine, Physiology Department, Al Azhar University (Assuit), Egypt
Abstract
Introduction: Contraception is defined as the intentional prevention of conception using various devices, sexual practices, chemicals, drugs, or surgical procedures. Thus, any device or act whose purpose is to prevent a woman from becoming pregnant can be considered as a contraceptive [1].
Objectives: The aim of this study is to compare the real situation in family planning clinics with selected practice recommendations for contraceptive use for WHO.
Subjects and Methods: An observational study was carried out in the family planning clinic at Ashmoun General hospital according to WHO recommendations for contraceptive use.
Results: The study included 4000 women; The mean age of the studied women was 31.9±4.2 years. Multipara women were about 90.1% according to type of contraception use (IUD) 41.2%, COCs 30.6%, Progestin-only injectables 15.2%, POPs 8.1%, Implants.3.2%, and Monthly injectables 1.7%.
Keywords: Contraception; IUD; COCs; Monthly injectables
Introduction
Family planning (FP) is a vital primary Healthcare intervention that saves lives of mothers and infants, empowers women, and supports their choices regarding their health, public life, and additional education. In addition, FP is considered as a short-term intervention to limit population growth and manage overpopulation problems [2].
Worldwide in 2017, about 63% of women in reproductive age (15-49Y) were using some form of contraceptives, with a prevalence above 70% in most developed countries. In developing countries, there were 214 million women in need to avoid pregnancy, while they were not using any modern contraceptive method (i.e., unmet need for FP). This huge number may be due to unavailable services, information, or lack of support from partners or community. Globally, the prevalence of unmet need for FP was 12% in 2017, and the rate was higher in Africa reaching 22% [3].
The Selected practice recommendations for contraceptive use (SPR) of WHO provides guidance regarding “how” to use contraceptive methods safely and effectively. The goal of these recommendations is to improve access to, and quality of, family planning services by providing policymakers, decision-makers and programme managers [4].
Contraceptive methods are often classified as either modern which are barrier methods such as male and female condoms, diaphragm, cervical cap and sponge; hormonal contraceptives that include oral, injectable, transdermal, vaginal ring, and implants; intrauterine device (IUD) or traditional which are rhythm method (periodic abstinence), withdrawal (coitus interruptus), fertility awareness-based methods and the lactational amenorrhea method [5].
Egypt is the most populated country in the Middle East and the third most populated country in Africa. Since 1990, there was gradual decrease in the Total Fertility Rate (TFR) in Egypt from 4.1 children per woman in 1991 to 3.0 in 2008, but unexpectedly, it increased to 3.5 during 2014 [6].
Egypt did not achieve Millennium Development Goals (MDG) 2015 target which was aiming at a contraceptive rate of 70% to achieve TFR of 2.1 children per woman by the year 2017. According to the United Nations Development Program in 2015, CPR ranged from 59% to 60%, during the previous 10 years with significant geographical differences [7].
Family planning service quality has been studied widely as an important target for improvement to increase acceptance and utilization of FP service. Training healthcare providers to provide a client-centered FP service including expanded contraceptive method choices and comprehensive effective accurate counselling is an important aspect of improving the quality of the service, which undoubtedly, improve clients’ satisfaction [8].
Egyptian Government provides contraceptive methods through Health Units services with very low price in Urban and Rural areas. The CPR varies widely across Egypt regions. It is reported that Urban women were more likely to be using contraceptives than rural women [6]. Different forms of birth control have different potential side effects. Not all, or even most, users will experience side effects from a method. The less effective the method, the greater the risk of the side-effects associated with pregnancy [9]. Minimal or no other side effects are possible with coitus interruptus, fertility awareness-based and lactational amenorrhea method [10].
Aim of the work
- Evaluate and compare the real situation in family planning clinics with selected practice recommendations for contraceptive use for
- Know the obstacles of applying selected practice recommendations for contraceptive use for WHO.
- How to help the state to improve the level of family planning
- To determine the level of knowledge of women about contraceptive
Patients and Methods
Study design: A cross-sectional healthcare center-based study
Location of the study: The study was conducted in Ashmoun General Hospital, Egypt. Women who are visiting family planning clinic in Ashmoun Hospital seeking for contraception use.
Patients are classified according to WHO contraceptive eligibility criteria as
follow:
Category 1: A condition for which there is no restriction for the use of the contraceptive method.
Category 2: A condition where the advantages of using the method generally outweigh the theoretical or proven risks.
Category 3: A condition where the theoretical or proven risks usually outweigh the advantages of using the method.
Category 4: A condition which represents an unacceptable health risk if the contraceptive method is used.
All participants were applied to history taking as recommended in WHO guidelines; personal history ,family history, medical and drug history, examination of the client; general, abdominal, pelvic, breast, genital examination and cancer cervix screening, investigations as recommended in WHO guidelines as blood pressure examination, haemoglobin test, STI and HIV screening lab tests, auditing of contraceptive methods selection in these conditions: post-partum , post-abortion ,breast-feeding , adolescence < 20 years old, above 40 years, smoking, diabetes, obesity, hypertension, liver disease, heart disease, DVT, cancer cervix, breast cancer , nullipara, PID, STI, uterine fibroid, autoimmune disease and emergency contraception.
Regarding examinations and tests that may be considered before initiation of contraceptives, the following classification was used in differentiating the applicability of the various examinations and tests:
Class A = the examination or test is essential and mandatory in all circumstances for safe and effective use of the contraceptive method.
Class B = the examination or test contributes substantially to safe and effective use, but implementation may be considered within the public health and/or service context. The risk of not performing the examination or test should be balanced against the benefits of making the contraceptive method available.
Class C = the examination or test does not contribute substantially to safe and effective use of the contraceptive method.
These classifications focus on the relationship of the examinations or tests to safe initiation of a contraceptive method.
Ethical Considerations
- Approval of ethical committee in the university was obtained before the
- Full informed consent was taken from the parents.
- Privacy of participants and confidentiality of the data were
- The patient has the right to withdraw from the study at any
- The authors declared that there is no conflict of interest or any financial support regarding the study or publication.
Statistical Analysis
Statistical Package for Social Science (SPSS v20) was used after transforming the data from Excel 2013 sheet. Categorical variables were presented by number and percent.
Results
A total of 4000 randomly selected women were included in the study.
Table 1: Patients Demographic and clinical characteristics, (Total N=4000).
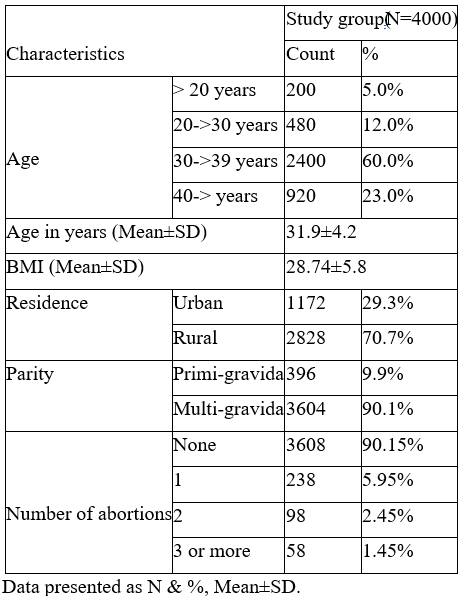
Table 1 showing the age of the studied women with mean age equal to 31.9±4.2 years., the mean BMI was 28.74±5.8. More than 70.7 % of the studied came from rural residence, multi-gravida was 90.1% whereas more than 90% of studied women have no history of abortion.
Table 2: Type of contraception used among studied cases.
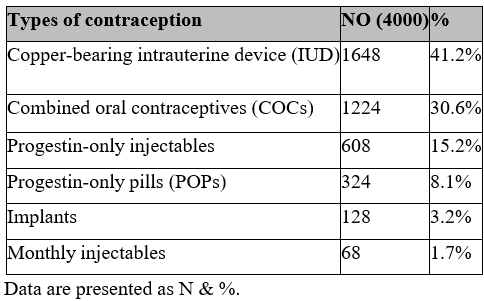
Table 2 showing different types of contraception used whereas Copper-bearing intrauterine device (IUD) was 41.2%, Combined oral contraceptives (COCs) 30.6% Progestin-only injectables was 15.2%, Progestin-only pills (POPs) was 8.1%, Implants was 3.2% and Monthly injectables was 1.7%
Table 3: Causes of discontinuation of different contraceptive methods used in the study, Total N=402.
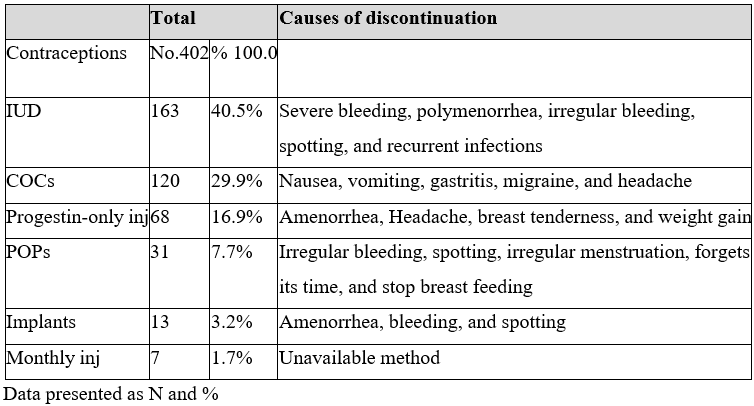
Table 3 demonstrate different causes of discontinuation of different contraceptive methods, among 4000 women only 402 (10.05%) of the studied women discontinued devices used in the study.
Among IUD users 163 (40.5%) women discontinued the contraception due to severe bleeding, polymenorrhagia, irregular bleeding, spotting, and recurrent infections COCs 120 (29.9%) women due nausea, vomiting, gastritis, migraine, and headache, Progestin-only inj 68 (16.9%) due to amenorrhea, headache, breast tenderness, and weight gain POPs 31 (7.7%) women due to irregular bleeding, spotting, irregular menstruation, forgets its time, and stop breast feeding, implants 13 (3.2%) women due amenorrhea, bleeding, and spotting, whereas monthly inj only 7(1.7%) women due to unavailability.
Table 4: Comparison between contraceptive current users and discontinuation by background characteristics, women’s attitudes, and social norms.

Table 4 provides a comparison between the current users and nonusers of contraceptive methods according to women’s background characteristics. As Table 4 indicates, there are statistically significant differences in the proportion of women who reported the current use of contraceptive methods in relation to various demographic factors. Significant differences were observed between users and nonusers of contraceptives according to women’s age, age at marriage, and years of education. The means of these variables were significantly higher among the current users of contraception than nonusers. Further, the proportions of users were significantly higher among women who were employed; lived in urban regions. Religion, whether women were Muslims or Christians, was not significantly associated with the use of contraception (p=0.061).
Table 5: Comparison between contraceptive current users and nonusers by background characteristics, women’s attitudes, and social norms.
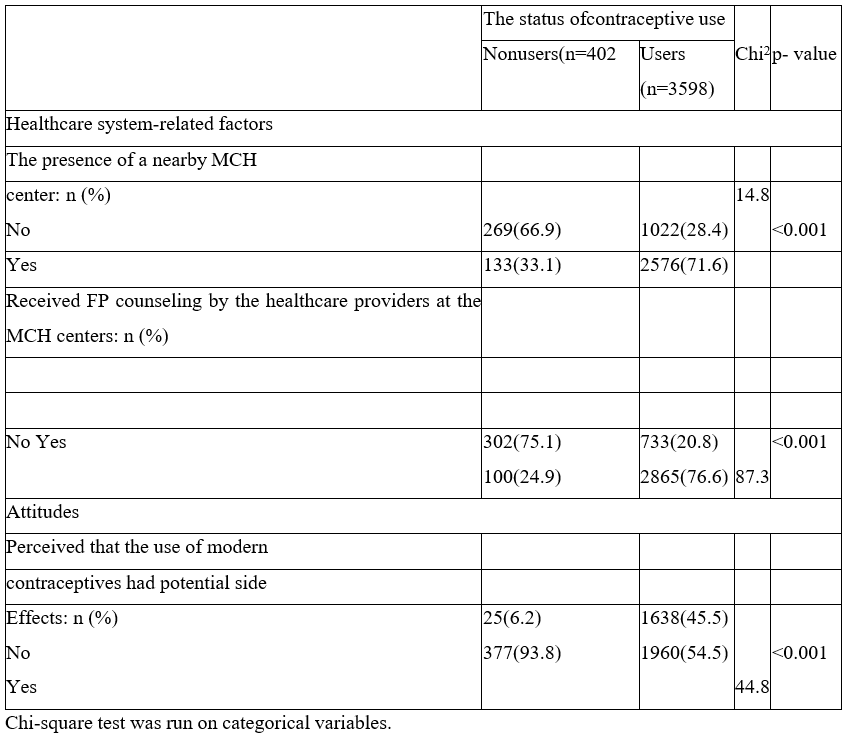
Table 5 demonstrate a comparison between contraceptive current users and nonusers by background characteristics, women’s attitudes, and social norms whereas the presence of a nearby MCH center, received FP counseling by the healthcare providers at the MCH centers, and perceiving that the use of modern contraceptives had potential side Effects were significantly associated with discontinuation of contraceptive methods, P<0.001.
Discussion
The results of this study make it evident that the status of contraceptive use among women in Ashmoun is affected by several factors at the individual, familial and institutional levels. At the individual level, the present. In Egypt, few studies have been conducted to investigate the relationship between women’s attitudes and social norms towards using of contraception [11].
This study also found that other aspects of an individual’s beliefs were significantly associated with the current use of contraceptives. These include women perceptions of potential side effects associated with modern methods and approval of contraceptive use for birth spacing. Not surprisingly, women who had concerns about contraceptive side effects were less likely to be current users. Many researchers have reported that women’s worries about the side effects of contraceptive methods may constrain their use of contraception. For example, a study by [12] demonstrated that one of the main reasons for contraceptive nonuse in southern Nigeria was women’s fears of side effects.
According to the 2008 Egyptian DHS, the users of contraceptive methods stopped using contraception for several reasons, including health concerns, desire for another child, contraceptive failure, and dissatisfaction with the method [13]. Elsewhere, similar findings were also reported [14,15].
Moreover, this study revealed that women’s approval of contraceptive use for birth spacing was one of the significant factors that influenced the current use of contraception. This finding agrees with the results of a study by [11], where a woman’s approval of birth spacing was also found to be a significant factor associated with the use of contraceptives among Egyptian women in the southern region. Similar findings were also reported in the literature [16-18].
In a study by [19], the use of contraceptives among Saudi women was reported to be mainly for birth spacing rather than a desire to limit family size. In Turkey, a woman’s approval of contraception was also observed as an influential variable in increasing the use of different methods versus nonuse [20]. The main reason for disapproval of contraceptive use among Turkish women was the lack of information about FP programs. In Egypt, the results of the 2008 DHS have illustrated that opposition to contraceptive use for birth spacing, either by women or their husbands, was reported to be limited [13].
At the institutional level, this study revealed that women who received FP counseling from healthcare providers at the MCH centers were more likely to be current users of contraception. In fact, the provision of contraception information by healthcare professionals has been supported as an effective way to enhance the use of contraceptive methods among women of childbearing age. Research has shown that providing women with accurate information about contraception and improving their access to necessary health education are fundamental to helping women making fertility decisions [21].
Moreover, authors reported that the lack of appropriate knowledge about contraceptive methods is an underlying factor for women’s anxiety about using contraception [22]. In Thailand, for example, [15] reported that one of the main barriers that impeded women’s use of contraceptives was lack of information about contraception. In Saudi Arabia, a study by [23] has illustrated that health workers played a limited role in providing married women with information about contraception. In Pakistan, a study by [24] also demonstrated that receiving messages from healthcare providers was strongly associated with women’s use of contraception. The study revealed that users of contraceptives were 3.8 times more likely to report having heard about FP from a healthcare provider compared with nonusers [24]. In the literature, repeated structured counseling by healthcare professionals is suggested as an effective approach to improving contraceptive acceptability and continuation [25-39].
Conclusion
In conclusion, women’s contraceptive behavior is embedded in the context of personal beliefs, social norms, and healthcare system-related factors. According to this study, women’s religious beliefs were found to be the strongest factor influencing the current use of contraceptive methods and it is crucial to stress the responsibilities of healthcare providers in increasing the prevalence of contraceptive use by promoting participant awareness in this regard.
References
- Jain R, Muralidhar Contraceptive methods: needs, options, and utilization. The Journal of Obstetrics and Gynecology of India, 2011; 61(6): 626-634.
- World Health WHO | Postpartum family planning: essential for ensuring health of women and their babies [Internet]. WHO? World Health Organization; 2018.
- United Nations Department of Economic and Social World Family Planning 201-Highlights [Internet]. New York; 2017.
- Mohllajee AP, Curtis KM, Flanagan RG, Rinehart W, Gaffield ML, Peterson HB. Keeping up with evidence: a new system for WHO’s evidence-based family planning American journal of preventive medicine, 2015; 28(5): 483-490.
- Obrowski M, Obrowski S. Birth control-current contraception devices and medications: Clinical review. MOJ Womens Health, 2016; 2(1): 22.
- El-Zanaty F, Way A. Egypt Demographic and Health Survey 2014 [Internet]. Cairo, Egypt: Ministry of Health and Population and ICF International;
- United Nations Development Program (UNDP); the Ministry of National Egypt’s Progress towards Millennium Development Goals [Internet]. Cairo; 2015.
- Clark H, RamaRao S, Unthank C, Machiyama K, Thatte N. Family Planning Evidence Brief – Expanding contraceptive Geneva, 2018.
- Skovlund CW, Morch LS, Kessing LV, Lidegaard O. Association of hormonal contraception with JAMA psychiatry, 2016; 73(11): 1154- 1162.
- Kraetschmer K. Medicinal Chemistry as Foundation for Contraception, Birth Control, Family Planning, And Fertility. International journal of Nursing Didactics, 2017; 7(8); 01-07.
- Gharaibeh MK, Oweis A, Shakhatreh FM, Froelicher ES. Factors Associated with Contraceptive Use among Jordanian Muslim Women: Implications for Health and Social Journal of International Women’s Studies, 2011; 12(3): 168-184.
- Omo-Aghoja LO, Omo- Aghoja VW, Aghoja CO, Okonofua FE, et al. Factors Associated with the Knowledge, Practice and Perceptions of Contraception in Rural Southern Ghana Medical Journal, 2009; 43(3): 115-121.
- UNICEF & UNFPA. Egyptian Demographic and Health Survey, 2011.
- D'Souza RM. Factors influencing the use of contraception in an urban slum in Karachi, Journal of Health & Population in Developing Countries, 2003; 1–10.
- Morrison V. Contraceptive Need among Cambodian Refugees in Khao Phlu International Family Planning Perspectives, 2000; 26(4): 188–192.
- Jejeebhoy SJ, Sathar Women’s Autonomy in India and Pakistan: The Influence of Religion and Region. Population and Development Review, 2001; 27(4): 687–712.
- Saleem A, Pasha GR. Women’s reproductive autonomy and barriers to contraceptive use in The European Journal of Contraception and Reproductive Health Care, 2008; 13(1): 83–89.
- Upadhyay UD, Hindin MJ. Do higher status and more autonomous women have longer birth intervals? Results from Cebu, Social Science & Medicine, 2005; 60: 2641–2655.
- Khraif RM. Fertility in Saudi Arabia: levels and determinants. A paper presented at XXIV General Population Conference: Salvador – Brazil, 2021.
- Alpu O¨, Fidan On the use of contraceptive methods among married women in Turkey. The European Journal of Contraception and Reproductive Health Care, 2006; 11(3): 228–236.
- Breaking the Contraceptive Barrier: Techniques for Effective Contraceptive Consultations. Association of Reproductive Health Professionals, Washington, DC, 2008.
- Arora N, Choudhary S, Raghunandan C. Young women opting for tubal sterilization in rural India: Reasons and implications. Journal of Obstetrics and Gynaecology, 2010; 30(2): 175–178.
- Al-Sheeha Awareness and Use of Contraceptives Among Saudi Women Attending Primary Care Centers in Al-Qassim. International Journal of Health Sciences, 2010; 4(1): 11-21.
- Fikree FF, Khan A, Kadir MM, Sajan F, Rahbar MH. What Influences Contraceptive Use Among Young Women in Urban Squatter Settlements of Karachi, Pakistan? International Family Planning Perspectives, 2001; 27(3), 130-136.
- Goonewardene M. Strategies to improve adherence and acceptability of hormonal methods for contraception: RHL commentary. The WHO Reproductive Health Library; Geneva, 2011.
- Bankole A, Singh S. Couples’ fertility and contraceptive decision- making in developing countries: hearing the man’s voice. International Family Planning Perspectives, 1998; 24(1): 15–24.
- Casterline JB, Sather ZA, Haque Obstacles to Contraceptive use in Pakistan: A study in Punjab. Studies in Family Planning, 2001; 32(2): 95-105.
- Chandhick N, Dhillon BS, Kambo I, Saxena NC. Contraceptive knowledge, practices, and utilization of services in the rural areas of India (an ICMR task force study). Indian J Med Sci, 2003; 57(7): 303-310.
- Dahal GP, Padmadas SS, Hinde PR. Fertility-limiting behavior and contraceptive choice among men in International Family Planning Perspectives, 2008; 34(1): 6-14.
- Fantahun M. Comparative study of the characteristics of family planning service users and non-users in northwest Ethiopia. Afr J Reprod Health, 2006; 10(1): 62-
- Gordon Women’s Education and Modern Contraceptive Use in Ethiopia. International Journal of Education, 2011; 3(1: E9). ISSN 1948-5476.
- Kaggwa EB, Diop N, Storey JD. The role of individual and community normative factors: A multilevel analysis of contraceptive use among women in union in Mali. International Family Planning Perspectives, 2008; 34(2): 79-88.
- Mahmood N, Ringheim Knowledge, Approval and Communication about Family Planning as Correlates of Desired Fertility among Spouses in Pakistan. International Family Planning Perspectives, 1997; 23(3): 122-145.
- Ogunjuyigbe PO, Ojofeitimi EO, Liasu Spousal Communication, Changes in Partner Attitude, and Contraceptive Use Among the Yorubas of Southwest Nigeria. Indian Journal of Community Medicine, 2009; 34(2): 112-119.
- Piotrow PT, Kincaid DL, Hindin MJ, Lettenmaier CL, Kuseka I, Silberman T, et al. Changing men’s attitudes and behavior: the Zimbabwe male motivation Studies in Family Planning, 1992; 23(6): 365–375.
- Rahayu R, Utomo I, McDonald P. Contraceptive Use Pattern among Married Women in Indonesia. Paper presented at the International Conference on Family Planning: Research and Best Practices, November 15-18, Kampala, Uganda, 2009.
- Sahin HA, Sahin Reasons for Not Using Family Planning Methods in Eastern Turkey. Eur J Contracept Reprod Health Care, 2003; 8: 11-16.
- Shah MA, Shah NM, Chowdhury RI, Menon I. Unmet need for contraception in Kuwait: issues for health care Social Science and Medicine, 2004; 59: 1573-1580.
- Sunil TS, Pillai VK. An analysis of reproductive health components in International Social Science Review, 2006; 81: 1-2. ISSN: 0278-2308.

