Epidemiological Profile of Myocardial Infarction with Non-Significant Stenosis of Coronary Arteries (MINOCA)
Moussaoui F*, Bali-Tabet R and Meziane Tani A
Departement of Cardiology, CHU of Tlemcen, Algeria
Received Date: 12/07/2023; Published Date: 05/12/2023
*Corresponding author: Moussaoui F, Departement of Cardiology, CHU of Tlemcen, Algeria
Abstract
Background: Myocardial infarction with non-obstructive coronary arteries (MINOCA) remains a puzzling clinical entity characterized by clinical evidence of myocardial infarction (MI) with normal or near-normal coronary arteries on angiography (stenosis <50 %).
This pathology is poorly understood, several studies are underway for a better understanding of this disease. The aim of our work was to review the literature and assess the epidemiology, clinical features, prognosis and etiologies of MINOCA.
Methods: Descriptive, prospective study, spread over a period of 36 months from January 2018 to December 2020 involving a total number of 585 patients undergoing coronary angiography at the cardiology department of CHU Tlemcen, for a reason for acute myocardial ischemia.
We defined the patients as having acute myocardial ischemia with obstructive coronary artery disease (MI-CAD) if there was revascularization or plaque ≥ 50% and as having MINOCA if there was <50% obstruction or a mechanism without plaque. Patients who received thrombolytics before angiography were excluded.
We studied the epidemiological, clinical and prognostic profile of the MINOCA population then compared them to patients with obstructive coronary artery disease and finally we established an etiological analysis of the MINOCA population.
Results: The number of MINOCA cases in our sample of 585 AMI patients was 10.25% vs. 525 (89.74%) cases of AMI-CO, it was more common in men (78.3% vs. 21, 7%; odds ratio at 3.61) and in the youngest patients.
MINOCA patients were more likely to be without traditional cardiac risk factors (7.9% vs. 2.1%; P <0.001) but more predisposed to non-traditional risk factors than AMI-CO patients (3.7% against 1.8%; P = 0.026). Smoking is the only traditional risk factor frequent in the MINOCA population versus MI-CAD (P at 0.001).
Depression, stress, drug addiction, DVT history and autoimmune disease history are more frequent in the MINOCA population versus MI-CAD (P <0.05)
STEMI are more found in the MINOCA population versus MI-CAD (P = 0.000)
In terms of prognosis, the MINOCA population had a better prognosis: less risk of recurrence than the MI-CAD population 6.7% versus 10.45% (P = 0.03) also less mortality 0% versus 4.6% (P = 0.007).
Conclusion: The patients with MINOCA were more men, smokers, depressed, stressed, drug addicts with hypercoagulable states compared to patients with obstructive coronary artery disease (MI- CAD) however they had a better quality of life and a good prognosis.
Introduction
The term "acute myocardial infarction" (AMI), which is used to describe a heart attack. When there are signs of heart muscle injury and necrosis in a context consistent with myocardial ischemia, the diagnosis of AMI is made [1-4]. There are two main categories of AMI: STEMI and non-STEMI. STEMI is used to describe patients with persistent chest pain and ST-segment elevation, while non-STEMI refers to patients without ST-segment elevation. AMI can also be classified into different types based on the cause and prognosis. One such type is "myocardial infarction with non-obstructive coronary arteries" (MINOCA), which occurs in the absence of significant coronary stenosis. This type of AMI was first described over 75 years ago and has been confirmed in several large studies, with up to 14% of AMI cases being MINOCA [5-8]. This type of AMI represents a diagnostic and therapeutic challenge, as many patients are discharged without a clear explanation for their symptoms [9-12].
Epidemiology
The prevalence of MINOCA (Myocardial Infarction with Non-Obstructive Coronary Arteries) in patients with MI (Myocardial Infarction) ranges from 1-15% depending on the studied population [9,10,13]. Studies such as ACTION Registry-GWTG, ANZACS-QI trials, COAPT, MINOCA-TR registry, GENESIS-PRAXY trials, and ORPKI registry have reported a MINOCA prevalence of 5.9%, 10.8%, 5.8%, 6.7%, 8.2%, and 7.8% respectively [14-17]. The NZACS-QI registry reported a higher MINOCA prevalence of 15% in the New Zealand population [18].
Definitions
The diagnosis of Myocardial Infarction with Non-Obstructive Coronary Arteries (MINOCA) is made in patients with a heart attack who meet the following criteria [19]:
1. Myocardial Infarction:
- There must be evidence of an increase or decrease in cardiac troponin levels with at least one value above the 99th percentile upper reference limit
- Clinical evidence supporting the diagnosis of a heart attack, including symptoms of ischemic heart disease, new electrocardiographic changes, pathological Q waves, evidence of loss of viable myocardium, or evidence of a coronary thrombus
2. Non-Obstructive Coronary Arteries:
- The angiography must show no obstructive disease (no stenosis greater than or equal to 50%) in any major epicardial vessel
- This includes patients with normal coronary arteries, mild luminal irregularities, or moderate coronary atherosclerotic lesions
No Alternative Diagnosis:
- The diagnosis must rule out alternative causes such as sepsis, pulmonary embolism, or myocarditis
Specific Causes o Minoca
- Atherosclerotic causes of myocardial necrosis
1. Plaque instability: Approximately 40% of MINOCA is caused by plaque rupture.1, plaque rupture and erosion are suspected in MINOCA patients with signs of coronary atherosclerosis on angiography: plaques causing stenoses <50%, authors here recommend that, if available, OCT or IVUS imaging be performed in these patients
-
- Non-atherosclerotic causes of myocardial necrosis
1. Epicardial coronary vasospasm: Found in 16 to 74% of patients.2 An intracoronary stimulation test is needed to diagnose coronary artery spasm. Ergonovine or acetylcholine (ACh) is generally used to stimulate coronary artery spasm. Coronary provocation tests are not systematically performed, as they are considered potentially Otherwise performed post-discharge (up to 6 weeks after an MI)
2. Coronary microvascular dysfunction: Can be detected in 30 to 50%.3 The coronary microcirculation (vessels <0.5mm in diameter) is not easily visualized on Microvascular dysfunction can potentially contribute to the pathogenesis of MINOCA
3. Coronary embolism/thrombosis: A coronary thrombosis or embolism leads to MINOCA if it is suspected. Thrombophilia screening yields positive results in about 14%.
4. Spontaneous coronary artery dissection (SCAD): Is a relatively rare non- atherosclerotic mechanism of MI; however, it is a frequent cause of MI in women under 50.
5. Inadequacy between supply and demand: Type 2 myocardial infarction in MINOCA patients is posed when a plausible cause exists (for example, tachycardia, anemia, hypotension, thyrotoxicosis)
Prognosis
The prognosis of patients with MINOCA depends on the underlying cause and is currently under active investigation. Most studies have shown that MINOCA patients have better outcomes than their counterparts with obstructive coronary artery disease [9,10].
Study Design: Study Protocol
Background:
Atherosclerosis is the most important etiology of acute myocardial ischemia, which manifests as significant coronary stenosis during coronary angiography. However, there is an entity that does not have significant coronary stenosis as seen on coronary angiography (healthy coronary network or location of a stenosis of less than 50%), known in the literature by the name MINOCA (myocardial infarction with non-obstructive coronary arteries), with a prevalence of between 6% and 14% of patients with acute myocardial infarction (AMI) [10,11]:
- What is the frequency of this entity in the population of AMI patients hospitalized in the cardiology department at the CHU of Tlemcen?
- What is the epidemiological, clinical profile and prognosis of this MINOCA population?
- Do these patients differ from those who have obstructive coronary artery disease?
- What are the mechanisms of this MINOCA pathology?
Objectives:
The study aims to:
- Describe the epidemiological, clinical and prognostic characteristics of patients with myocardial infarction without significant stenosis of coronary arteries.
- Compare the epidemiological, clinical, and prognostic characteristics of this population with those with obstructive coronary artery disease.
- Determine the causes of this MINOCA
Population and Methods
Study type: Observational, descriptive, prospective, monocentric, progressive recruitment study.
Study population
Inclusion criteria:
The inclusion criteria for the study are as follows:
- Patients presenting with symptoms compatible with acute myocardial infarction (AMI) based on universal AMI criteria
- Coronary arteries without significant stenosis as defined by the absence of ≥50% stenosis in the responsible coronary artery
- No clinically apparent specific cause for the clinical presentation. The universal AMI criteria include:
- Detection of an increase or decrease in cardiac troponin levels with at least one value above the 99th percentile reference limit
- Clinical evidence supporting the infarction, as shown by at least one of the following:
1. Symptoms of myocardial ischemia
2. New ischemic electrocardiographic changes
3. Development of pathological Q waves
4. Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality in a pattern consistent with an ischemic cause
5. Identification of a coronary thrombus by angiography or
Exclusion Criteria:
- Cases of tako-tsubo or evident myocarditis at admission
Exclusion Criteria:
- Patients who received thrombolytics before the coronary angiography was performed
Recruitment location and period:
- Subjects were recruited in a progressive manner at the coronary angiography unit of the cardiology department at the CHU Tlemcen.
- We included all patients hospitalized for ACS from throughout the Tlemcen
- The work took place over a three-year period from January 2018 to December
Parametres and study protocols
Methods
This is a descriptive, single-center, prospective, observational study conducted in the cardiology department of CHU Tlemcen over a period of 36 months from January 1, 2018 to December 31, 2020. A questionnaire was completed for each patient. The variables studied were collected from pre-coronary angiography forms and medical records of the patients using a data collection. The follow-up of these patients was performed through physical exams and telephone conversations.
Statistical analysis: Data analysis was performed using the SPSS software.
Study Results
The Frequency of Minoca: Figure 1
60 cases of MINOCA out of 585 cases of AMI >>>> So 10.25%
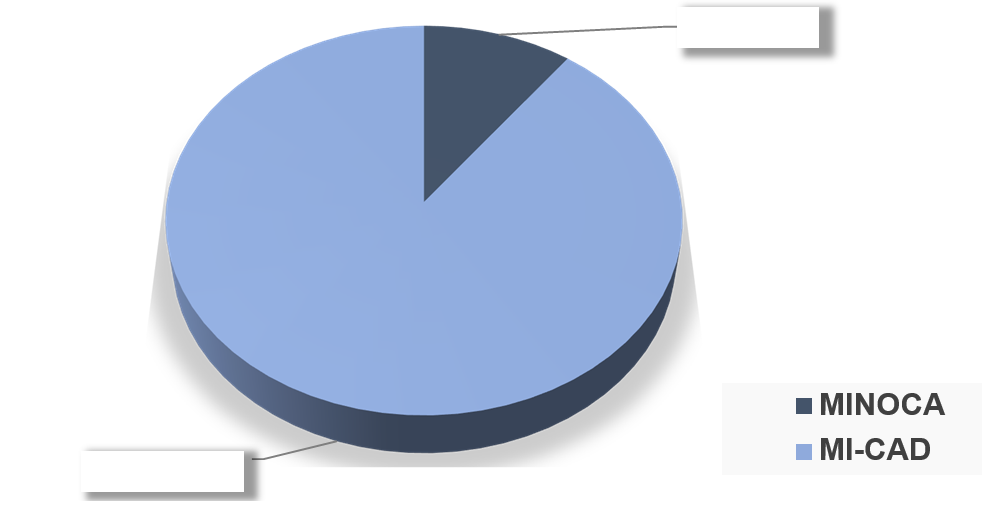
Figure 1: Comparative analytical study of the minoca population with the acute myocardial ischemia with obstructive coronary arteries (mi-cad) population.
Gender distribution MINOCA versus MI-CAD: Figure 2
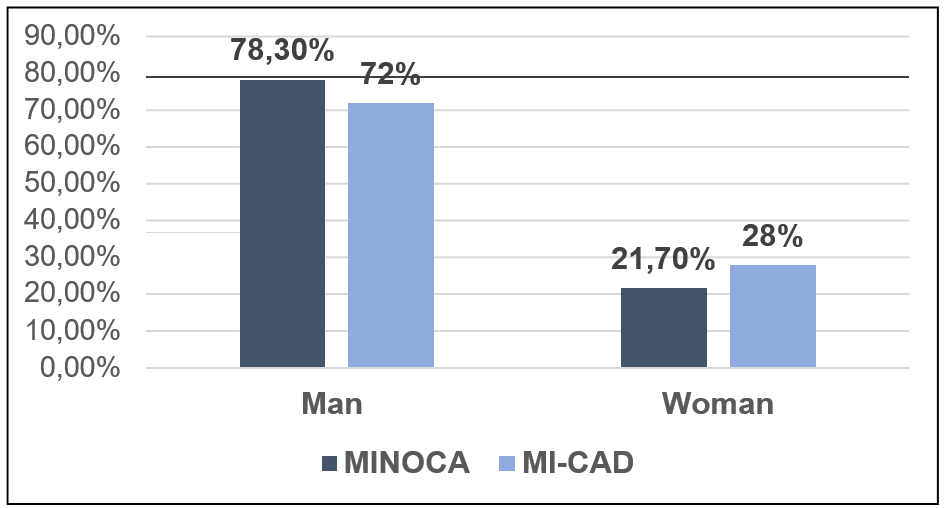
Figure 2: No significant difference was found between the MINOCA and MI-CAD population based on gender (P=0.297).
Breakdown by mean age MINOCA versus MI-CAD: Figure 3
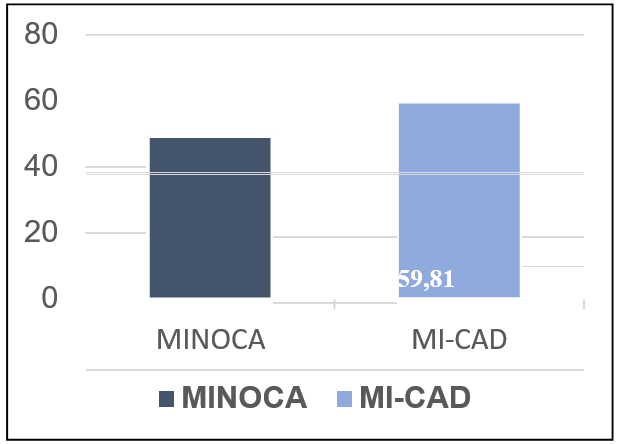
Figure 3: No significant difference was found between the MINOCA and MI-CAD populations based on gender (P=0.297). The MINOCA population was found to be younger compared to the MI- CAD population, with an average age of 49.35 years for MINOCA and 59.81 years for MI- CAD (P = 0.0001).
Comparison according to the frequency of conventional risk factors between the MINOCA and MI-CAD population: Figure 4

Figure 4
The study found that hypertension was more commonly found in the MI-CAD population compared to the MINOCA population, but the difference was not significant (P=0.066). Diabetes was more frequently found in the MI-CAD population compared to the MINOCA population, and the difference was significant (P=0.023). Dyslipidemia was more commonly found in the MI-CAD population compared to the MINOCA population, but the difference was not significant (P=0.087). Smoking was more frequent in the MINOCA population compared to the MI-CAD population, and the difference was significant (P=0.001). Obesity was more frequently found in the MINOCA population compared to the MI-CAD population, but the difference was not significant (P=0.088). Coronary hereditary was more commonly found in the MI-CAD population compared to the MINOCA population, but the difference was not significant (P=0.164). History of MI was more frequent in the MI-CAD population compared to the MINOCA population, and the difference was significant (P=0.001). History of angina was also more frequent in the MI-CAD population compared to the MINOCA population, and the difference was significant (P=0.008). The study concluded that diabetes, history of MI, and history of angina are more common in the MI-CAD population compared to MINOCA, but smoking is the only risk factor that is more common in the MINOCA population compared to MI-CAD.
Comparison according to the frequency of unconventional risk factors between the MINOCA and MI-CAD population: Figure 5
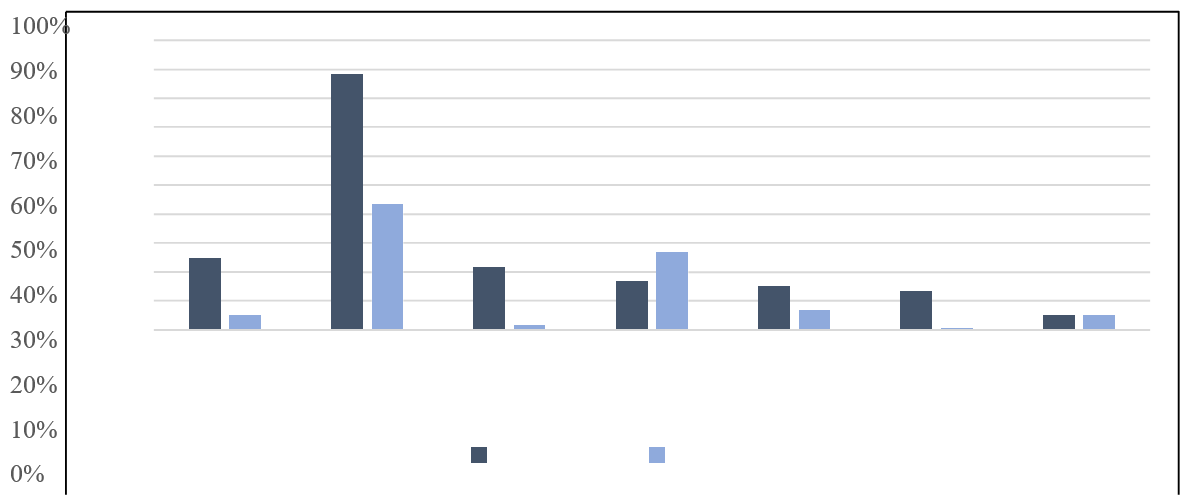
Figure 5: Dépression Stress Drogues Sédentarité ATCD de TVP ATCD de ATCD de maladie auto- Dysthyroïdie immune MINOCA MI-CAD.
Depression, stress, and drug use were found to be more common in the MINOCA population compared to the MI-CAD population with a significant difference (P=0.000). A history of deep vein thrombosis was also found to be more common in the MINOCA population compared to the MI-CAD population with a significant difference (P=0.025). A history of autoimmune disease was also found to be more common in the MINOCA population compared to the MI-CAD population with a significant difference (P=0.000). However, there was no significant difference found in the history of dysthymia between the two populations (P=0.962). A sedentary lifestyle was found to be more common in the MI-CAD population compared to the MINOCA population with a non-significant difference (P=0.088).
The distribution according to the indication of the urgent coronary angiography in MINOCA versus MI-CAD: Figure 6

Figure 6: The NSTEMI are more represented in the MI-CAD population versus MINOCA with a significant difference P=0.000, while STEMI are more commonly found in the MINOCA population versus MI-CAD also with a significant difference P=0.000.
Distribution Based on Prognostic Factors MINOCA vs. MI-CAD
Recurrence: Figure 7
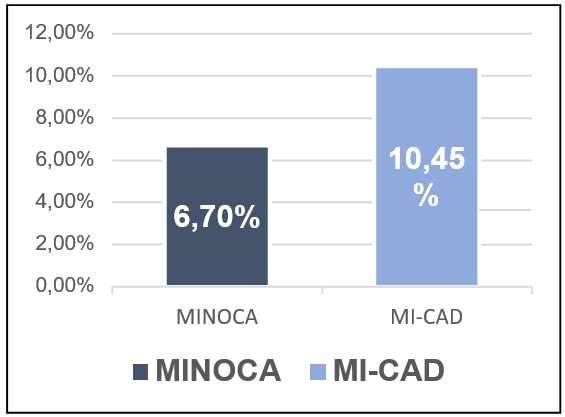
Figure 7: The MINOCA population has a lower risk of recurrence than the MI-CAD population, 6.7% versus 10.45% with a significant difference, P=0.03.
The return-to-work MINOCA versus MI-CAD: Figure 8
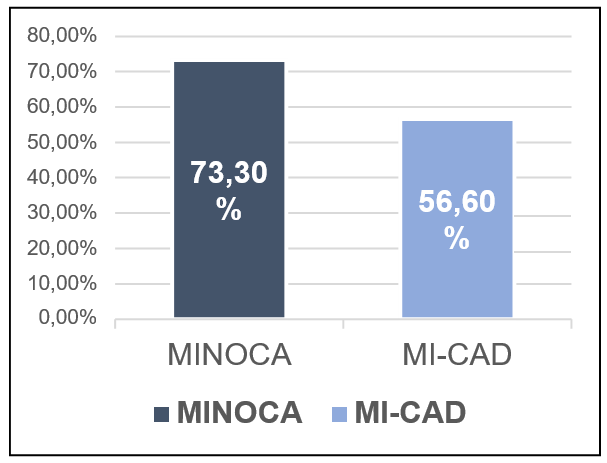
Figure 8: 73.3% of MINOCA patients have returned to work, compared to only 56.6% of MI-CAD patients who have returned to work, with a significant difference, P=0.013.
The mortality: Figure 9
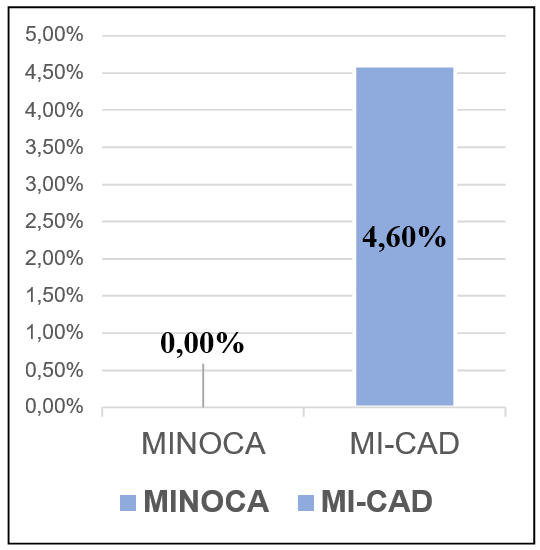
Figure 9: The mortality rate in MI-CAD patients is 4.6% versus 0% in MINOCA patients with a significant difference, P=0.007.
Etiological Study:
An etiological evaluation was performed on 52 patients through a cardiac MRI and a thrombophilia evaluation on 40 patients.
Results: Figure 10
1. Instability of the plaque, embolism, and microvascular dysfunction was found in 33% of patients and was evidenced by focal sub-endocardial ischemia on cardiac
2. Hypercoagulability was found in 10% of patients, with 3 cases of antiphospholipid syndrome, 1 case of protein S and C deficiency, and 2 cases of lupic
3. Vasospasm was found in 3% of patients, with spasms of a coronary artery detected after an intracoronary Risordan injection.
4. Spontaneous dissection of a coronary artery was found in 2% of patients and was evident on coronary angiography with good clinical evolution without any
5. Myocarditis was found in 3% of patients after a cardiac MRI and diagnosis was unclear at the time of inclusion.
6. COVID-19 infection was found in 12% of patients who were diagnosed during the
7. Undetermined diagnoses were found in 37% of patients due to difficulty accessing complementary exams.
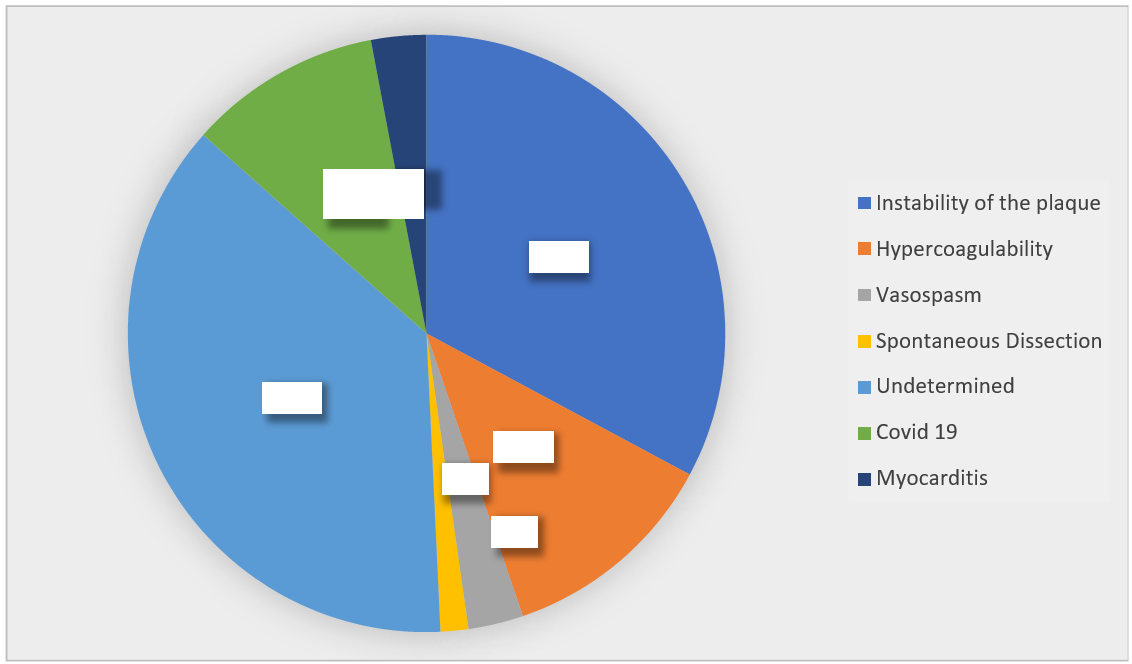
Figure 10
Discussion
Introduction:
In our study, we aimed to compare the characteristics of MINOCA (Myocardial Infarction with Non-Obstructive Coronary Arteries) and MI-CAD (Myocardial Infarction with Obstructive Coronary Arteries) patients and identify any differences between the two groups.
Demographic Data:
In our study, we found that the mean age of MINOCA patients was 57.36 ± 10.26 years, while the mean age of MI-CAD patients was 55.17 ± 9.16 years, with no significant difference between the two groups (P = 0.123).
Traditional Risk Factors:
A systematic review by Pasupathy S et al, including the VIRGO study and other studies, showed that MINOCA patients have a lower prevalence of dyslipidemia compared to their SCA counterparts with obstructive coronary artery disease [10,11]. Other traditional coronary artery disease risk factors, such as hypertension, diabetes, smoking, and a family history of myocardial infarction, are less frequent in MINOCA patients [11].
Non-Conventional Risk Factors:
In our study, we found that depression, stress, drug use, previous DVT and autoimmune disease history were more frequent in the MINOCA population compared to MI-CAD, with a significant difference, but there was no significant difference between the two populations for other factors (sedentary lifestyle and hypothyroidism history).
Previous studies have shown the same results: The VIRGO study showed that MINOCA patients had fewer traditional cardiac risk factors but more often had risk factors such as previous drug use, hypercoagulability syndrome, venous thromboembolism and autoimmune diseases [11]. Daniel M et al reported in a study that anxiety and depression were also frequent in MINOCA patients compared to IMA patients with obstructive coronary artery disease [20,21].
Clinical Presentation:
In our study, we found that NSTEMI (Non-ST Segment Elevation Myocardial Infarction) was more represented in the MI-CAD population compared to MINOCA, with a significant difference (P = 0.000), while STEMI (ST Segment Elevation Myocardial Infarction) was more found in the MINOCA population compared to MI-CAD, also with a significant difference (P = 0.000). However, Pasupathy S et al reported in a systematic review that STEMI and NSTEMI had similar ratios in patients [10].
Prognostic Factors
Recurrence:
In our work, we found a 12-month recurrence rate for the MINOCA population of 6.7%, significantly lower compared to the MI-CAD population of 10.45% with a significant difference P=0.03.
Bainey and al. studied the 1-year composite endpoint of death and/or reinfarction rate in MINOCA patients with angiography without coronary obstruction which were significantly lower than in MINOCA patients presenting stenosis <50% (3.9% and 6.1%, [p = 0.028], respectively).
Mortality:
In our work, we found a 12-month mortality rate for the MINOCA population of 0%, significantly lower compared to the MI-CAD population which was 4.6%, a non-significant difference P=0.007.
Safdar et al. reported similar results: 1 and 12-month mortality of MINOCA and IDM with obstructive coronaropathy [1 month: 1.1% and 1.7% (p = 0.43); 12 months: 0.6% and 2.3% (p
= 0.68), respectively] were found, while Pasupathy et al. reported that mortality rates were significantly lower in the MINOCA group compared to IDM with obstructive coronaropathy [in-hospital: 1.1% and 3.2% (p = 0.001); 12-month 3.5% and 6.7% (p = 0.003), respectively].
Etiologies:
In our work, we found ischemic embolic and plaque instability in 33% (20 patients), hypercoagulability in 10% (6 patients), vasospastic in 03% (02 patients), myocarditis in 03% (02 patients), spontaneous dissection in 02% (01 patients), concomitant Covid-19 infection in 12% (7 patients) while we found no etiologies in 37% (22 patients).
We limited ourselves to these results as it was not our main objective of the study and there were several difficulties, including:
Difficult access to some complementary tests such as cardiac MRI and thrombophilia tests. Non-performance of provocation tests for patients (patient refusal)
Unavailability of coronary imaging exams such as IVUS and OCT in our catheterization center.
In the literature, the VIRGO11 study reported a rate of 75% of undetermined etiologies, 20% of spontaneous coronary dissection, 4% of coronary spasm, and 1% of embolization, this also confirms that the etiological evaluation of MINOCA is not easy and remains obscure in the majority of cases.
Conclusion
MINOCA is a common clinical entity among patients with AMI and encompasses numerous etiologies that can be difficult to detect.
The number of MINOCA cases in our sample of 585 AMI patients was 10.25% compared to 89.74% of obstructive coronary artery disease. It was more frequent among men and younger patients. MINOCA patients were more likely to be without traditional cardiac risk factors (7.9% compared to 2.1%; P <0.001), but more prone to nontraditional risk factors than AMI- OCD patients (3.7% compared to 1.8%; P=0.026); smoking was the only frequent traditional risk factor in the MINOCA versus AMI-OCD population (P=0.001).
Depression, stress, drug use, a history of DVT, and a history of autoimmune disease were more frequent in the MINOCA population versus AMI-OCD with a significant difference. These patients were more likely to present as STEMI (P=0.000).
The MINOCA population had a better prognosis:
The majority of MINOCA patients had a good quality of life compared to AMI-OCD patients with a significant difference.
MINOCA patients had a lower risk of recurrence than the AMI-OCD population 6.7% versus 10.45% with a significant difference (P=0.03).
- % of MINOCA patients returned to work, while only 56.6% of AMI-OCD patients did so with a significant difference (P=0.013).
The 12-month mortality rate for the MINOCA population was 0%, significantly lower than the AMI-OCD population, which was around 4.6% (P=0.007, not significant).
The mechanisms of MINOCA in our cohort were varied: ischemic embolic etiology and plaque instability accounted for 33% (20 patients), hypercoagulability in 10% (6 patients),
vasospasm in 3% (2 patients), myocarditis in 3% (2 patients), spontaneous dissection etiology in 2% (1 patient), concurrent COVID-19 infection in 12% (7 patients), and etiologies were not found in 37% (22 patients).
This observation raises some research questions that could improve our understanding of this entity and its characteristics compared to obstructive coronary artery disease and the determination of optimal treatment based on specific cause in the future.
Recommendations
- Quickly address acute myocardial ischemia, especially STEMI and NSTEMI, by widespread use of interventional therapy and rapid access to coronary angiography,
which significantly improves the overall prognosis of coronary disease through early revascularization.
- Familiarize all cardiologists with the term MINOCA, which represents a significant portion of acute myocardial ischemias.
- Fight against cardiovascular risk factors in general and especially against smoking, drug abuse, and consumption of all types of drugs, which are important causes of this
- Detect and properly manage patients with depression, anxiety, and stress through general medical consultations and refer them to psychologists and psychiatrists for follow-up; these are important risk factors for
- Properly manage hypercoagulation states, especially a history of deep vein thrombosis, and search for a thrombophilia that constitutes a risk factor for
- Detect and manage autoimmune diseases, which are also a risk factor for
- Facilitate and generalize access to cardiac MRI in patients with MINOCA: ensure that its cost is covered by the social security system, especially for this
- Facilitate the acquisition and equipment of cardiac catheterization rooms with new coronary imaging tools, especially IVUS and
References
- Niccoli G, Scalone G, Crea Acute myocardial infarction with no obstructive coronary atherosclerosis: mechanisms and management. Eur Heart J, 2015; 36(8): 475–481.
- Agewall S, Beltrame JF, Reynolds HR, Niessner A, Rosano G, on behalf of the WG on Cardiovascular Pharmacotherapy, et al. ESC working group position paper on myocardial infarction with non-obstructive coronary Eur Heart J, 2017; 38(3): 143–153.
- Hartley A, Marshall DC, Salciccioli JD, Sikkel MB, Maruthappu M, Shalhoub Trends in mortality from ischemic heart disease and cerebrovascular disease in Europe: 1980 to 2009. Circulation, 2016; 133(20): 1916–1926.
- Townsend N, Wilson L, Bhatnagar P, Wickramasinghe K, Rayner M, Nichols M. Cardiovascular disease in Europe: epidemiological update Eur Heart J, 2016; 37(42): 3232–3245.
- Miller RD, Burchell HB, Edwards JE. Myocardial infarction with and without acute coronary occlusion: a pathologic AMA Arch Intern Med, 1951; 88: 597–604.
- Gross H, Steinberg WH. Myocardial infarction without significant lesions of coronary arteries. Arch Int Med (Chic), 1939; 64: 249–267.
- DeWood MA, Spores J, Notske R, Mouser LT, Burroughs R, Golden MS, et al. Prevalence of total coronary occlusion during the early hours of transmural myocardial N Engl J Med, 1980; 303: 897–902. doi: 10.1056/NEJM198010163031601
- DeWood MA, Stifter WF, Simpson CS, Spores J, Eugster GS, Judge TP, et al. Coronary arteriographic findings soon after non-Qwave myocardial N Engl J Med, 1986; 315: 417–423. doi: 10.1056/NEJM198608143150703
- Smilowitz NR, Mahajan AM, Roe MT, Hellkamp AS, Chiswell K, Gulati M, et al. Mortality of myocardial infarction by sex, age, and obstructive coronary artery disease status in the ACTION Registry-GWTG (Acute Coronary Treatment and Intervention Outcomes Network Registry-Get with the Guidelines). Circ Cardiovasc Qual Outcomes, 2017; 10: e003443. doi: 1161/CIRCOUTCOMES.116.003443
- Pasupathy S, Air T, Dreyer RP, Tavella R, Beltrame JF. Systematic review of patients presenting with suspected myocardial infarction and nonobstructive coronary arteries [published correction appears in 2015; 131: e475]. Circulation, 2015; 131: 861–870. doi: 10.1161/ CIRCULATIONAHA. 114.011201
- Safdar B, Spatz ES, Dreyer RP, Beltrame JF, Lichtman JH, Spertus JA, et al. Presentation, clinical profile, and prognosis of young patients with myocardial infarction with nonobstructive coronary arteries (MINOCA): results from the VIRGO study. J Am Heart Assoc, 2018; 7: e009174. doi: 1161/JAHA.118.009174
- Williams MJ, Barr PR, Lee M, Poppe KK, Kerr AJ. Outcome after myocardial infarction without obstructive coronary artery Heart, 2019; 105(7): 524–530.
- Bainey KR, Welsh RC, Alemayehu W, Westerhout CM, Traboulsi D, Anderson T, et al. Population-level incidence and outcomes of myocardial infarction with non-obstructive coronary arteries (MINOCA): insights from the Alberta contemporary acute coronary syndrome patient’s invasive treatment strategies (COAPT) study. Int J Cardiol, 2018; 264: 12–17.
- Kilic S, Aydın G, Coner A, Doğan Y, Arican Ozluk O, Celik Y, et al. MINOCA-TR. Prevalence and clinical profile of patients with myocardial infarction with non-obstructive coronary arteries in Turkey (MINOCA-TR): A national multi- center, observational Anatol J Cardiol, 2020; 23(3): 176–182.
- Raparelli V, Elharram M, Shimony A, Eisenberg MJ, Cheema AN, Pilote L. Myocardial Infarction with No Obstructive Coronary Artery Disease: Angiographic and Clinical Insights in Patients with Premature Can J Cardiol, 2018; 34(4): 468–476.
- Rakowski T, De Luca G, Siudak Z, Plens K, Dziewierz A, Kleczyński P, et al. Characteristics of patients presenting with myocardial infarction with non-obstructive coronary arteries (MINOCA) in Poland: data from the ORPKI national J Thromb Thrombolysis, 2019; 47(3): 462–466.
- Barr PR, Harrison W, Smyth D, Flynn C, Lee M, Kerr AJ. Myocardial Infarction Without Obstructive Coronary Artery Disease is Not a Benign Condition (ANZACS-QI 10). Heart Lung Circ, 2018; 27(2): 165–174.
- Tamis-Holland JE, Jneid H, Reynolds HR, Agewall S, Brilakis ES, Brown TM, American Heart Association Interventional Cardiovascular Care Committee of the Council on Clinical Cardiology, Council on Cardiovascular and Stroke Nursing, Council on Epidemiology and Prevention, and Council on Quality of Care and Outcomes Research, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Circulation, 2019; 139: e891_e908.
- Daniel M, Agewall S, Berglund F, Caidahl K, Collste O, Ekenb.ck C, et al. Prevalence of Anxiety and Depression Symptoms in Patients with Myocardial Infarction with Non- Obstructive Coronary Am J Med, 2018; 131(9): 1118–1124.
- Daniel M, Agewall S, Caidahl K, Collste O, ck C, Frick M, et al. Effect of Myocardial Infarction with Nonobstructive Coronary Arteries on Physical Capacity and Quality- of-Life. Am J Cardiol, 2017; 120(3): 341–346.
- Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD: the Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). Circulation, 2018; 138: e618–e651. doi: 1161/CIR.0000000000000617.
- Tornvall P, Brolin EB, Caidahl K, et al. The value of anewcardiacmagnetic resonanceimagingprotocol inmyocardial infarctionwith non-obstructive coronary arteries (MINOCA)—a case-control study using historical controls from a previous study with similar inclusion BMC CardiovascDisord, 2017; 17(1): 199.
- Curzen N, Rana O, Nicholas Z, et al. Does routine pressure wire assessment influence management strategy at coronary angiography for diagnosis of chest pain? the RIPCORD Circ CardiovascInterv, 2014; 7(2): 248–255.
- Tamis-Holland JE, Jneid H, Reynolds HR, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Circulation, 2019; 139(18): e891–e908.

