“To Observe the Navicular, Drop in High Heel and Non- High Heel Footwear Users’’
Purnima Kumari1,*, Priyanka Kumari1 and Shahiduz Zafar2
1Research Scholar Department of Physiotherapy, Galgotias University, India
2Professor Department of Physiotherapy, SMAS Galgotias University, India
Received Date: 20/06/2023; Published Date: 10/11/2023
*Corresponding author: Purnima Kumari, Research Scholar Department of Physiotherapy, Galgotias University, Greater Noida, U.P, India
Abstract
Introduction: Navicular drop is described as subtraction of peak of navicular tuberosity from floor in neutral position of subtalar and peak of navicular tuberosity from floor in weight bearing position. It is a very important component in diagnosis of pronated foot.
Methodology: The current study is a comparative observational study. For this purpose, 300 collegiate students of both genders, out of which 150 were high heel users and 150 were non high heel users between age of 18-35 years from Galgotias University who fit into the inclusion criteria were selected according to our convenience. All subjects involved in this study by their own consent. Their navicular drop was measured using business card, ruler, removable marker, pencil etc. same way as described in Navicular Drop Test which has been used by Brody in his studies. Foot pain was also measured in the current study with help of numeric pain rating scale (NPRS).
Results: 13.33% of total high heel users found to have navicular drop and 4.66% of total non- high heel user found to have navicular drop. Therefore, we can say that navicular drop is more in high heel users as compared to non- high heel users.
Conclusion: It is concluded that navicular drop in high heel footwear user is more than navicular drop in non-high heel footwear user. Pain is more in subjects who use high heel footwear for more than 5 days in a week.
Keywords: Navicular Drop; Foot Arch; High Heel Footwear; Non- High Heel Footwear; Foot Pain; NPRS; MLA; LLA
Introduction
The subtraction of navicular tuberosity’s height in two positions from the ground gives us measurement of navicular drop that is we subtract height of navicular tuberosity in weight bearing position from height when foot is in subtalar neutral and keeping in mind that both heights are measured from ground. It was reported that the mainly young collegiate students, runners, kathak dancers have navicular drop [1-3]. It was also reported that players with a higher body weight, BMI, Q-angle, genu recurvatum, tibial torsion angle, and total leg length are thought to have higher navicular drop [4]. It was also seen that people who are overweight have navicular drop [5]. An NDRT less than 9mm and more than 2mm was found in 93.8% of population while NDLT was less than 9mm and larger than 2mm in 96.4% of the population [6].
From earlier times, people wear shoes with high heel to make them appear more taller than what they are in real. As per data of Medical Association of America which deals with Podiatrics,39-69% females choose to go with high heels. Out of 100%, 40% females use high heels on daily basis in their routine either they go for office or for shopping [7]. 37.5 % of women who wore high heels complaint of foot pain, according to the study done by Mehnaaz Sameera et.al., high heel makes the person appear taller, wiser, and more confident [8]. It was reported, putting shoes with a high heel for extended period of time is thought to cause chronic pain and abnormalities [9]. When the person wears high heels, their hips and spine are out of alignment, putting more pressure on their knees and feet [8]. Every single foot can be characterised as feet that are under pronated or have a foot with increased arch (the foot’s longitudinal arch present on medial side of foot is raised higher than the normal is called supinated foot), foot that is pronated or has a low-arch (longitudinal arch located medially is decreased more than the normal is called pronated foot), or normal arched, depending on the MLA structure [10]. According to the study done by Ashok Aenumulapalli et.al. a foot is considered as flexible flat foot if ND greater or equal to 10mm. Flexible flat foot affects 12.8% of males and 14.4% of females [11].
Navicular bone’s internal structural arrangement
The most significant bone out of seven bones that comprise ankles and foot’s tarsus is our navicular bone. Its location is medial side of foot, near to cuboid bone, prior to the talus head, and behind the cuneiform bones. It's one of the midfoot's five bones [2,12]. Structure of navicular bone is shaped pyriform, tiny in size and having uneven surface [13]. It has a concave posterior surface with two inconspicuous ridges which are attached with bones called cuneiform which are 3 in number. [12]. An external bump like appearance projecting at medial surface which lies inferiorly which is typically easy to palpate directly anterior to the medial malleolus is termed as navicular tuberosity [12]. An articular complex termed as subtalar is made by talocalcaneonavicular joint which is also famous as acetabulum pedis [14]. It is named so because of having some similar properties as that of joint called ball and socket [14]. Morphological structures that support skeleton are comprised of surface of navicular bone which provides attachment site to talus head and lies posteriorly, as well as surface of calcaneus which provides site of attachment for talar surface which lies medial and frontal side [14].
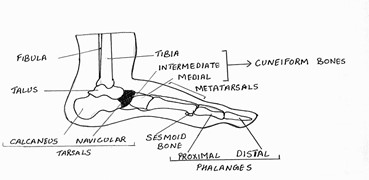
Figure 1: Representing Human Navicular Bone along with its surrounding structures.
Attachments and articulations of the navicular bone
The medial sole ligament which is also famous as the spring ligament and the lateral ligament which is a part of the bifurcated ligament support these bones. [14]. The tibialis posterior tendon is the navicular's only muscle connection [1,13]. The posterior tibialis muscles help keep the navicular bone stable [15]. The tendon extends downwards to enter the canal which is located in depth of the posterior part of the tibia [13]. There are many ligaments that attach to the foot bone which is pyriform shaped and named as navicular. There is an inferior connection to navicular bone by the ligament known as plantar calcaneonavicular [14]. Even most of the researches are not clear about the anatomy and morphology of this ligament but this is one of those ligaments which provides a good sort of connection to calcaneus and navicular bone and talar head is supported by the socket formed by this ligament [16]. Borders located on anteromedial aspect of sustentaculum tali on the talus bone give rise to the superomedial calcaneonavicular ligament [17]. Here onwards, it runs in dorsolateral aspect of navicular bone’s posterior portion and links tibial tendon which lies posteriorly [17]. Coronoid’s fossa superior segment which lies on frontal aspect of sustentaculum tali, gives rise to the inferior calcaneonavicular ligament [16]. It is inserted just next to the point where insertion position of calcaneonavicular ligament is located [16].
Function of the ligaments and associated structures of the navicular bone
The principal stabilisers which maintain the stability of medial longitudinal arch of foot in static condition are ligaments popularly famous as calcaneonavicular [17]. Bifurcate ligament is mainly contributed by ligaments called lateral calcaneonavicular and medial calcaneocuboid and bifurcate ligament is shaped as tissue as alphabet letter Y [18]. The lateral calcaneonavicular ligament arises anteromedially from the sinus tarsi, which is positioned lateral to that articular surface of talus which is at the anterior side [17]. These fibres combine to produce a strong band that aids in lateral foot stability [17]. The navicular is frequently referred to as quoin of longitudinal arch of foot which lies medially because of the positioning that is on top aspect of arch and character of keeping foot arch in place [19]. Tarsals, metatarsals, ligaments, and tendons make up the foot’s arches [20]. They assist in balancing the body’s weight while standing and walking, as well as acting as shock absorbers [11].
Pathophysiology of navicular bone
There are several types of clinical disorders which directly involve navicular bone [18]. Navicular is prone to stress fractures, which can result in Navicular stress syndrome. Müller Weiss syndrome is an osteonecrosis of the navicular bone that develops spontaneously in adults and may be detected radiographically [21]. The anomaly known as Accessory Navicular Bone is one of the most prevalent associations [18]. The navicular is also utilised therapeutically in the Navicular Drop Test, which can be used to assess foot pronation [18]. Because it is located on the medial side of the tarsus, between the talus behind it and the cuneiform bones in front, the height of the navicular bone is important in maintaining the integrity of MLA [11]. Excessive navicular mobility puts patient at greater risk of injuries to medial side of the shin as well as knee [3].
Navicular Drop Test
Brody initially introduced the Navicular Drop Test (NDT) in year 1982 to evaluate extent of pronation present in runner’s foot [23]. Static evaluation tool that calculates the change in position of bony prominence present on navicular surface that is tuberosity of navicular from foot position when subtalar joint is in neutral condition to a position when there is weight bearing on foot and the subject is in standing posture [24]. Subject is informed to stand with loading foot by body weight, also keep his or her foot in a neutral posture of the subtalar joint ("talar head congruent") [25]. Measure the distance between the most prominent region of the navicular tuberosity and the supporting surface (floor or step) [26]. After the patient has relaxed, use a ruler to calculate the quantity of navicular expedition in sagittal plane [26]. Alternatively, the test can be done backwards, measuring from a relaxed state to talar neutral in a standing position [26]. Many physicians prefer to conduct this examination by recording beginning and termination points using a business card put at inner side of foot for measuring the difference using a plastic ruler [26]. The NDT is used to assess MLA function, which is important when examining individuals with overuse injuries [3]. NDT is widely utilised in clinical practice and has no limitations in terms of space or expenses [27].

Figure 2: Showing Navicular height measurement in sub talar neutral position.
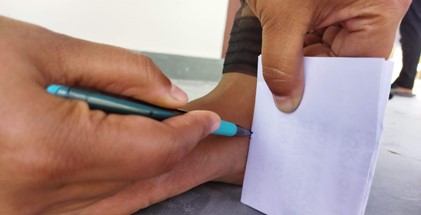
Figure 3: Representing Navicular height measurement in weight bearing position.
Effects of navicular drop
Navicular drop is defined by presence of a swollen, reddish bony protrusion medially and significant discomfort in middle of foot. Because of structural abnormalities and atrophy of the muscles that support the arch, navicular drop occurs [1]. ACL, MTSS and patellofemoral pain syndrome have all been linked to abnormal navicular drop. Excessive navicular drop was also linked to plantar intrinsic muscle fatigue, according to another study [1]. Navicular drop was used to assess foot pronation in a clinical setting [1]. Navicular drop is a chronic disease characterised by insufficient MLA support and excessive subtalar joint pronation [28,29]. The navicular drop has been considered as the best metric for determining foot pronation [4]. The usual navicular drop range is 5 to 9mm, with values below 4mm indicating an increased arch and values above 10mm indicating a decreased arch [30].
Bone structures, ligaments, and extrinsic and muscles which are present deep inside foot, all work together and govern MLA. Weakness in gluteus maximus causes hip joint to internally rotate and the foot to pronate, resulting in foot abnormalities [31]. Due to additional stresses on the arches, a higher BMI combined with poor musculature can cause the foot arches to collapse [32,33].
The role and construction of longitudinal arch that is located medially (MLA), is influenced by navicular posture, assumed to be a threat for tear [4]. The MLA may deteriorate as a result of increasing pronation caused by ligament laxity and recurrent stressors [22]. Hallux valgus is caused by fall down of MLA and an overly pronation in foot [34,35]. Pronation, a condition in which people stand or walk with their feet on side of ground rather than flat on the ground [36]. Obesity cause pronation, which causes our heels to point outwards and our ankles to be closed together [36]. A positive NDT was also reported to be suggestive of plantar intrinsic muscle exhaustion [37]. Patients with a history of ACL tears have been observed to have excessive navicular drop, which is likely make prone people to shin splints and MTSS [1]. Excessive arch deformation, as evaluated by navicular drop, is connected to a number of lower extremity overuse injuries including MTSS and patellofemoral pain syndrome [38-41]. It was documented that sprinters with a low navicular drop had higher number of injuries in ankle, fifth metatarsals fractures caused due to stress, and rubbing syndrome of iliotibial band [42]. It may also aid in identifying those with patellofemoral pain syndrome who might benefit from prefabricated orthotics and reduced exercise [42]. NDT may also be useful in evaluating individuals with lower extremity overuse complaints [16]. The NDT should be used in concert with other methods as part of a comprehensive lower extremity examination [43]. Inconsistent reliability is present due to complexities of palpation of navicular tuberosity and sub-talar joint as well as % bearing of weight on the lower limb [44]. To address some of these difficulties, other version of examination exists like as one that uses a single leg stance relaxed posture, navicular drop test in sit-to-stand (SSNDT), and navicular drop test in dynamic posture (DNDT) [44].
Aim and Objective of the study
1.The aim of the study is to study about navicular drop in high heel user and non- high heel user.
2.The main objective of this research is to observe navicular drop in high heel user as compared to non- high heel user.
3.To see the impact of wearing high heel on foot arch
Hypothesis of research: There is a significant difference in navicular drop between high heel and non-high heel footwear users.
Null Hypothesis: There is no significant difference in navicular drop between high heel and non-high heel footwear users.
Method and Materials
This study included a comparative observational study assessing comparison between navicular drop in high heel and non-high heel footwear users. The subjects were selected according to the convenience and a total of 300 subjects enrolled in undergraduate and postgraduate programmes at Galgotias University, Greater Noida involved in this study. The subjects included male and female of age 18-35 years. The subjects were divided in two groups i.e., Group A and Group B (150 subjects in each group). Group A subjects were high heel footwear users who use high heel more than 3 inches for more than 5 days in a week and Group B subjects were non high heel footwear users. The study strictly excluded the subjects with any foot deformity, neuromuscular complication, any recent injury of leg, fracture of tarsal and meta tarsal bone, diabetic, CVA, abnormal thyroid, lymphedema. The study duration was 6-7 weeks.
Procedure
We First of all, we explained about our study to the students and discussed the complications of using high heel footwear to the collegiate students to match the trend going on in our society. The subjects were made aware about the importance of our study, approach, aims and data required for the study purpose and after that we have taken the consent from the subjects who were willing to participate in the study. The data used in this study is demographic data which includes name, age, gender, occupation, weight, height and BMI. All these data were collected using data collection forms. They were asked about whether they use high heel footwear or non-high heel footwear. If they were high heel user then they were asked about the duration for which they use high heel. They were asked about their pain status either they feel pain or not after using high heel footwear. If they feel pain then pain was measured using Numerical Pain Rating Scale.
After taking these details, each participant was asked to remove his/her footwear and socks.
Then participants were asked to stand erect on even floor. The navicular tuberosity height from the floor was measured in two different position using scale, pen and index card. One measurement was made when the subject was bearing weight and the other one was taken in sub talar neutral position.
After this, using the two mentioned above measurements, we calculated the navicular drop in each participant using the Brody’s method of navicular drop measurement and recorded the data obtained in this measurement.
Results
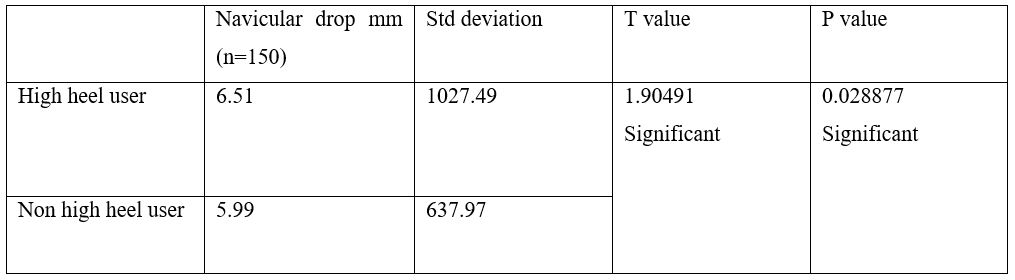
The data obtained in the measurement of navicular drop has been studied and analysed properly using statistical data analysis tool. The comparative data has been obtained using one tailed T test. Data for high heel users(n=150) and non-high heel users(n=150) have been separately analysed accurately.
13.33% of total high heel users found to have navicular drop. 4.66% of total non-high heel user found to have navicular drop. The results are very clear and showed that there is a significant effect of high heel footwear on navicular drop. Age and BMI have a significant role in navicular drop. BMI with mean value 22.17 kg/m2 have a great significant impact on navicular drop. Subjects with mean age 23.21 years have more navicular drop. Therefore, we can say that navicular drop is more in high heel user than non-high heel user.
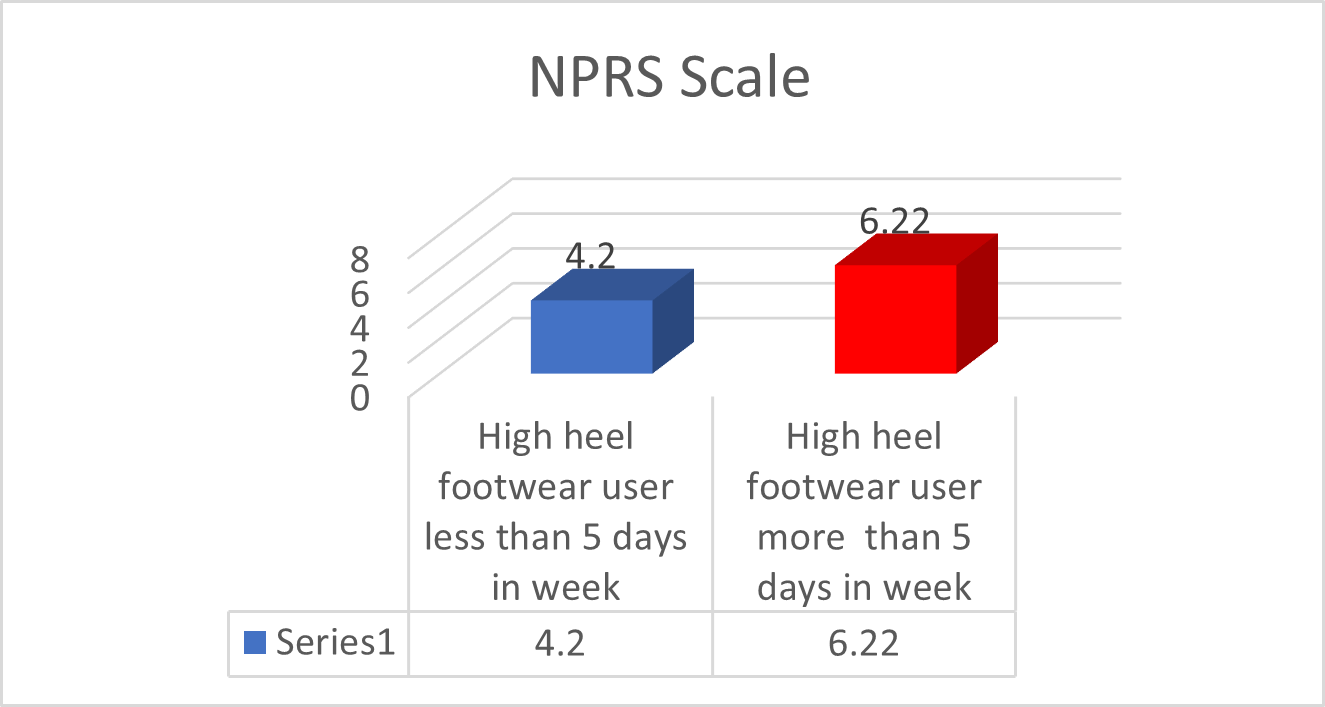
Pain is also linked with use of high heel as we have found 22 out of 150 subjects using high heel footwear complaining of severe pain. These are the subjects who used high heel for more than 5 days in a week. So, it can be said that pain is also associated with duration of high heel use. The subjects who used high heel for more than 5 days a week felt more pain than those who used high heel for less than a week.
Table 1 shows the analysis of demographic data of both the groups i.e., Group A and Group B related to age, weight, height and BMI.
Table 2 shows the analysis of navicular drop difference in the two groups i.e., Group A and Group B and shows a clear result of the p value being less than .05 and henceforth we can accept the alternate hypothesis that there is a significant effect of high heel footwear on navicular drop.
Graph no-1 shows comparative difference of navicular drop in both the groups i.e., Group A and Group B.
Graph no-2 shows comparative difference between pain between high heel users for more than 5 days in a week and high heel users for less than 5 days in a week.
Table 1: Showing demographic data such as age, weight, height & BMI has been analysed using T Test (Demographic data analysis).
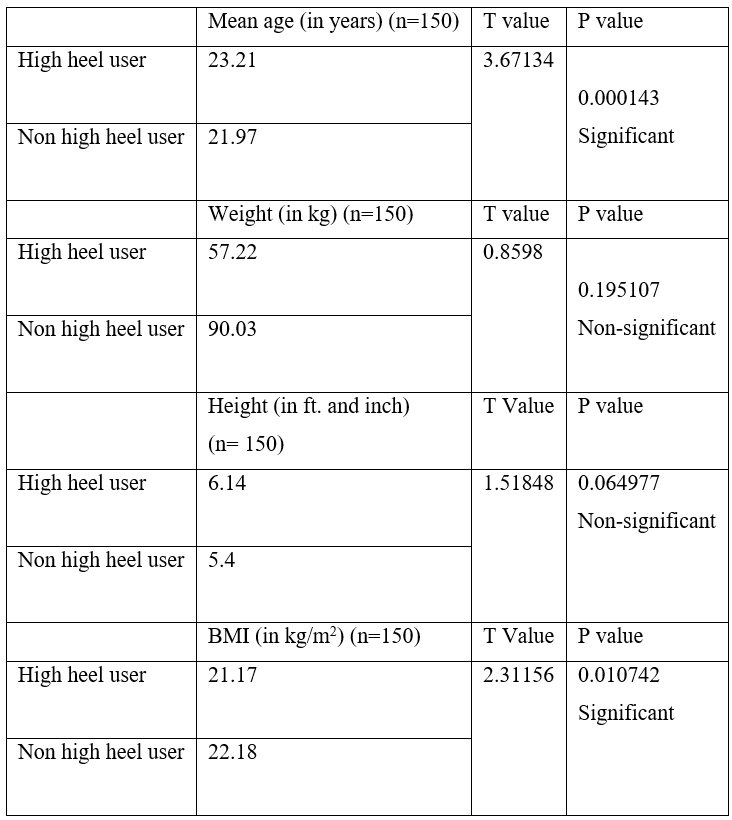
Table 2: Representing navicular drop-in group A (high heel user) and group B (non high heel user) has been analysed using T test.
Graph 1: showing graphical representation of navicular drop in high heel user and non-high heel user.
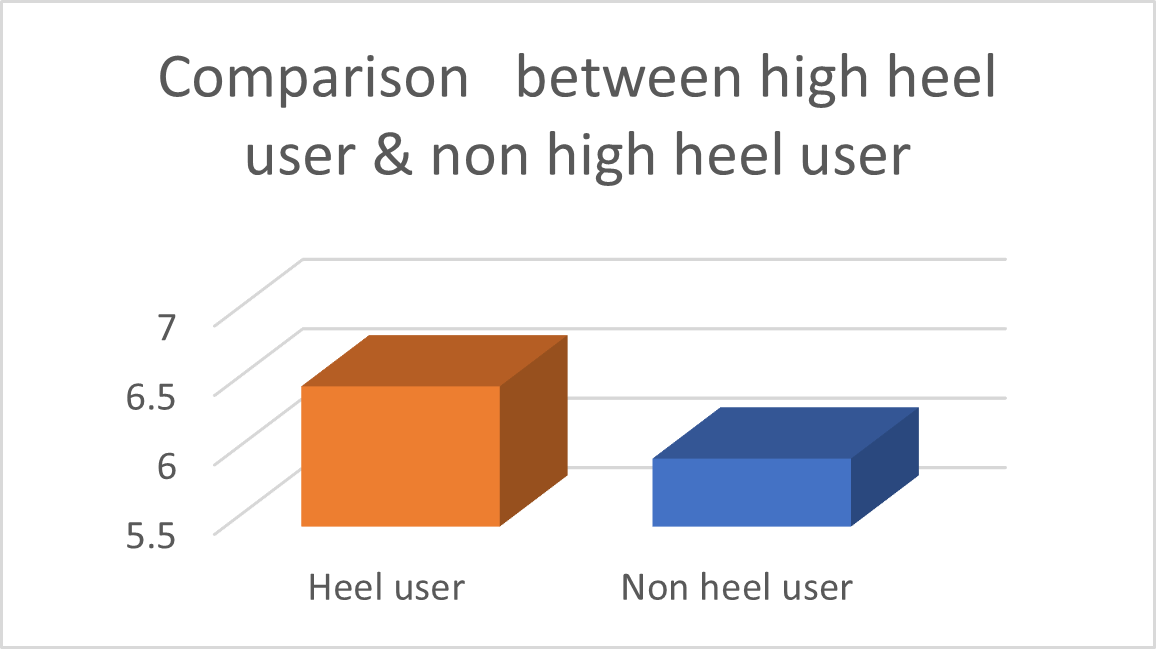
Table 3: Representing pain in high heel users on NPRS scale, (people who use high heels footwear less than 5 days and more than 5 days in week) has been analysed using T test.
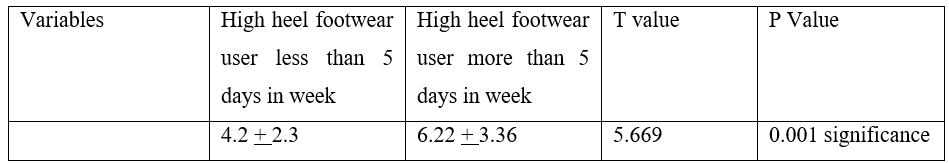
Graph 2: Showing graphical representation of pain in high heel user on NPRS scale, high heel user less than 5 days and more than 5 days in week.
Discussion
The motive of the research was to study about navicular drop in high heel footwear user and non-high heel footwear user. The study was designed to determine whether there is any difference between navicular drop in high heel and non-high heel footwear user. The results disclosed presence of significant difference between navicular drop in high heel and non-high heel footwear user. In this study, various data was analyzed for both the groups in which some data played a significant role and have a great impact on navicular drop. In this current study BMI and age have a great impact on navicular drop in high heel footwear user. Subjects with mean age 23.21 years have more navicular drop. Subjects with mean BMI 21.17 kg/m2 have more navicular drop.
In this study it is found that mild grade of pain is associated with high heel footwear user even if they have no navicular drop. Foot arch is also associated with navicular drop in this study; similar study done by Chaya Garg et.al. in 2014 also found that the navicular drop is more in subjects with low foot arch. But the difference between the studies is that we have observed the navicular drop and its association with foot arch in collegiate high heel and non-high heel footwear user but in the study done by Chaya Garg et.al, the authors also observed this difference in runners and non-runners and found that runners have considerably pronated foot [2].
In this study, it is found that higher BMI also played a significant role in navicular drop and is similar to the study done by Harish S. Krishna et.al in 2018 and the result of both studies showed same results and found that if BMI increases then navicular drop also increases [36] but the only difference between the two studies is that they have found that weight is also affecting the navicular drop significantly but, in our study, weight has no significant effect on navicular drop.
We have used Navicular Drop Measurement Test of Brody to measure the navicular drop in high heel and non-high heel footwear user and this is completely similar to the test used by R.M.B Dilrukshi Rajkaruna et.al. in 2015 and found that NDT is one is the more reliable test to measure navicular drop [20]. According to study done by Muge Kirmizi et.al. (2020) also reported that NDT is more reliable than the other traditional techniques and it can help clinicians and researchers develop clinical strategies for detecting foot position in a more reliable way [58]. Juan Carlos Zuil-Eschobaret et.al. (2018) also found that NDT is a simple, repeatable and valid test [56].
We have measured the navicular drop in standing position similar to Ji-Won Park et.al. (2010) because navicular drop measurement in standing position has higher intra rater and inter-rater reliability than sitting position [61].
As we have noted the constant complain of pain in subjects using high heel footwear for more than 5 days a week similar to the study done by Mehnaaz Sameera Arifuddin et.al. in 2021 that showed that high- heeled footwear can cause damage of the foot architecture, which leads to back and foot pain [8]. Nihar Ranjan Mohanty et.al. (2019) noticed that a higher navicular drop is hypothesized to be associated with athletes who have a higher body weight, BMI, Q-angle, genu recurvatum, tibial torsion and total leg length and we have also found BMI to be associated with navicular drop in this current study [4]. Chun-Ming Yin et.al. (2016) also reported that the usage of high-heeled shoes over a long period of time might cause changes in the arch morphology and we have also noted this in our study that foot arch is associated with navicular drop [48].
As a result, it is very clear that navicular drop is more in high heel footwear users as compared to non-high heel footwear users. And by the end of this study, it proves that its alternate hypothesis is true or accepted.
Conclusion
Therefore, this study resulted into giving a significant effect of high heel footwear on navicular drop of collegiate students.
Limitations of the study
- We could have selected the subjects from different professions so that we can relate high heel use duration with navicular drop.
- We could have measured the dynamic navicular drop in high heel and non-high heel footwear user.
- We could have selected large sample size for this study.
Future scope of the research
- The study can be used to determine the type of footwear we use.
- The study can be used to decide for which group of people should use which type of footwear according to the BMI.
Conflicts of interest -There is no conflict of interest in this study.
Funding: There was no funding from any agency, it was a self-funded study
References
- Malik Manoj Kaur Jaspreet, Punia Sonu, Bhagesh. Navicular Drop Gender Difference Among College Students: A Cross Sectional Study, International Journal of Scientific Research and Review, 2018; 3(4): 40.
- Nikhil Aggarwal, Chhaya Garg, Hameera Bawa. Comparison of foot posture in runners (sprinters) and non- runners in Indian population; the physiotherapy post, 2014; 6(1).
- Shweta Chandan, Savita Tamaria, Davinder Gaur, Charu Chadha, Priyanka Sharma. Cross-Sectional Study of Foot Posture Index, Navicular Drop and Arch Index in Kathak Dancers International Journal of Research & Review, 2018; 5.
- Nihar Ranjan Mohanty, Avinashi Tiwari, Shyamal Koley. Estimation of static navicular its correlation with selected anthropometric and lower extremity anatomical alignment variables in university level female judo player, international journal of physiology, nutrition and physical education; 2019; 4(1): 1331-1336.
- APC Udyamali Pathirana, Watson Arulsingh, Joseph Oliver Raj. Does BMI variation change the height of foot arch in healthy adults: a cross sectional study; The Foot and Ankle Online Journal, 2015; 8(4). DOI:3827/faoj.2015.0804.0003
- Umesh Adhikari, Watson Arulsingh, Ganesh Pai, Joseph Oliver Raj. Normative values of Navicular drop test and the effect of demographic parameters- A cross sectional study; Annals of Biological Research, 2014; 5(7): 40-48.
- Jiang Yinzi Shang, Xiang Geng, Chen Wang, Li Chen, Chao Zhang, Jiazhang Huang Xu Wang, et al. Influences of high-heeled shoe parameters on gait cycle, centre of pressure trajectory, and plantar pressure in young females during treadmill walking; Journal of Orthopaedic Surgery, 2020; 1-9. DOI: 1016/j.gaitpost.2020.07.065
- Saimah Naseer, Ravinder Prakash Babu, Ashok Panjala, Mehnaaz Sameera Arifuddin, Hunaina Manfusa, Ephraim Vikram Rao. Comparison of medial longitudinal arches of the foot by radiographic method in users and nonusers of high-heeled footwear among young women; Journal of the Anatomical Society of India, 2021; 70(4): 226-232.
- Grethe E Borchgrevink, Annja T Viset, Eivind Witso, Berit Schei, Olav A Foss. Does the use of high-heeled shoes lead to fore-foot pathology? A controlled cohort study comprising 197 women; foot and Ankle Surgery, 2016; 22: 239-243; DOI: 1016/j.fas.2015.10.004
- Duaa Alshadli, Albert Chong. correlating foot posture with foot mobility using a high-accuracy foot measurement system. DOI:1109/I2MTC.2019.8827146
- Ashok Aenumulapalli, Manor Mohan Kulkarni, Achleshwar Ramnarain Gandotra. Prevalence of Flexible Flat Foot in Adults: A Cross-sectional Study; Journal of Clinical and Diagnostic Research, 2017; 11(6): AC17-AC20. DOI: 7860/JCDR/2017/26566.10059
- Soames RW. Anatomy and Human Movement E-book; structure and function; Elsevier Health Sciences, 2018.
- Golano P, Farinas O, Saenz I. The anatomy of navicular and periarticular structures. Foot and ankle clinics, 2004; 9(1): 1-23. DOI: 1016/S1083-7515(03)00155-4
- Epeldegui T, Delgado E. Acetabulum pedis. Part I: Talocalcaneonavicular joint socket in normal foot. Journal of paediatric orthopaedics. Part B, 1995; 4(1): 1-10.
- Fredrick Anthony Gardin, David Middlemas, Jenniefer L Williams, Steven Leigh. Navicular drop before and after fatigue of the ankle invertor muscles; International Journal of Athletic Therapy & Training, 2013; 18(6): 36-39. DOI:1123/ijatt.18.6.36
- Prapto D. Dreyer ma anatomy, bony pelvis and lower limb, navicular bone.
- Steginsky B, Vora A. What to do with the spring ligament; foot and ankle clinics, 2017; 22(3): 515-527. DOI: 1016/j.fcl.2017.04.005
- Kafka RM, Aveytuwa IL, Choi PJ, DiLandro AC, Tubbs Rs, Loukas M, et al. Anatomico-radiological study of the bifurcate ligament of the foot with clinical significance. Cureus, 2019; 11(1). DOI: 7759/cureus.3847
- Neumann DA. Kinesiology of the musculoskeletal system- e- book: foundations for rehabilitation. Elsevier health, 2013.
- Dilrukshi Rajakaruna MB, Watson Arulsingh, Joseph Oliver Raj, Mukesh Sinha. A studied to corelate clinically validated normalised truncated Navicular height to Brody’s Navicular drop test in characterising medial arch of foot. BMR medicine, 2015; 1(1): 1-7.
- Samin M, Moukafddam HA, Smitaman. Imaging of Muller-Weiss syndrome: a review of clinical presentation and imaging spectrum. American Journal of Roentgenolgy, 2016; 207(2): W8-W18. DOI: 2214/AJR.15.15843
- KI Seok Nam, Jung Won Kwon, OH-Yun Kwon. The Relationship between Activity of Abductor Hallucis and Navicular Drop in One –leg Standing Position; Journal of Physical Therapy Science, 2012; 24: 1103-1106.
- Brody TM. Techniques in the evaluation and treatment of the injured runner; Journal of Orthopaedic Clinics of North America, 1982; 13: 541-558. https://doi.org/10.1016/S0030-5898(20)30252-2
- Vinicombe A, Raspovic A, Menz HB. Reliability of navicular displacement measure as a clinical indicator of foot posture. Journal of American Podiatrics Medical Association, 2001; 91: 262-268. DOI:7547/87507315-91-5-262
- Zoran Z Sarcevica, Andreja P Tepavcevic. Association between abductor hallucis abductor force and navicular drop index, a predictive correlational study; Journal of Paediatric Orthopaedics B, 2021; 30: 484–487. DOI: 1097/BPB.0000000000000840
- Menz HB. Alternative techniques for the clinical assessment of foot pronation; Journal of American Podiatrics Medical Association, 1998; 88(36): 119-29. DOI: 7547/87507315-88-3-119
- So-yeon Kim, Jung-eun Yoo, Da-hyum Woo, Bo-young Jung, Bo-ram Choi. Inter and Intra-Rater Reliability of Navicular Drop Tests Position; Journal of Korean Physical Therapy Science, 2019; 26(1): 9-14.
- Nam KS, Kwon JW, Kwon OY. The relationship between activity of abductor hallucis and navicular drop in the one-leg standing position; Journal of physical therapy science, 2012; 24: 1103-1106.
- Bahar Kulunkoglu, Yasemim Akkubak, Afra Alkan. Effect of foot posture on foot specific health related quality of life; Journal of Sports Medicine andTherapy, 2018; 3: 017-013. https://dx.doi.org/10.29328/journal.jsmt.1001022
- Mansour Eslami, Mohsen Damavandi, Reed Ferber. Association of Navicular Drop and Selected Lower-Limb Biomechanical Measures during the Stance Phase of Running; Journal of Applied Biomechanics, 2014; 30: 250-254. DOI: 1123/jab.2011-0162
- Young-Mi Goo, Tae-Ho Kim, Jin-Yong Lim; The effects of gluteus maximus and abductor hallucis strengthening exercises for four weeks on navicular drop and lower extremity muscle activity during gait with flatfoot; The Journal of Physical Therapy Science, 2016; 8: 911–915. DOI: 1589/jpts.28.911
- Manish Kumar, Divya Sanghi, Pratiksha Arya, Jyoti Kataria. a correlational between navicular drop and quadriceps angle amongst normal and overweight middle –aged individuals; bioscience biotechnology research communications, 2021; 14(2): 891-896. DOI:http://dx.doi.org/10.21786/bbrc/14.2.68
- Choughala A, Phanse V, Khanna E, Panda. Screening of body mass index and functional flatfoot in adult: an observational study. International journal of physiotherapy research, 2015; 3(3): 1037-1041.
- Perera A, Mason L, Stephens M. The pathogenesis of hallux valgus; The Journal of Bone and Joint Surgery, 2011; 93: 1650-1961. DOI: 2106/JBJS.H.01630
- Steinberg N, Finestone A, Noff M, Zeev A, Dar G. Relationship between lower extremity alignment and hallux valgus in women. Foot & ankle international, 2013. https://doi.org/10.1177/1071100713478407.
- Harish S Krishna, Jazeel NM, Riyas Basheer, Madhuripu Srejisha PK, Dainy Varghese. Correlation of Body Mass Index with Navicular Height in Youngs; International Journal of Information Research and Review, 2018; 5(8): 5659-566.
- Hadlee DL, Leonard JL, Hart JM, Ingersoll CD, Hertel J. Fatigue of the plantar intrinsic foot muscles increases navicular drop. Journal of Electromyography Kinesiology, 2008; 18: 420-425. DOI: 1016/j.jelekin.2006.11.004
- Newman P, Witchalis J, Waddington G, Adams R. Risk factors associated with medial tibial stress syndrome in runners: a systematic review and meta-analysis.; Journal of Sports Medicine, 2013; 4: 229– 241. DOI: 2147/OAJSM.S39331
- Reinking MF, Austin TM, Richter RR, Krieger MM. Medial tibial stress syndrome in active individuals: a systematic review and meta-analysis of risk factors; Sports Health, 2017; 29(3): 252–261. DOI: 1177/1941738116673299
- Hamstra-Wright KL, Bliven KCH, Bay C. Risk factors for medial tibial stress syndrome in physically active individuals such as runners and military personnel: a systematic review and meta-analysis. British journal of sports medicine, 2015; 49(6): 362–369. DOI: 1136/bjsports-2014-093462
- Winkelmann ZK, Anderson D, Games KE, Eberman LE. Risk factors for medial tibial stress syndrome in active individuals: an evidence-based review; Journal of athletic training, 2016; 51(12): 1049-1052. https://doi.org/10.4085/1062-6050-51.12.13
- Glyn PE, Weisback PC. Clinical Prediction rules: A physical therapy reference manual. Batson, Jones and Barlett; 2011 Menz HB; Alternative techniques for the clinical assessment of foot pronation; Journal of American Podiatrics Medical Association, 1998; 88: 119-129. DOI: 7547/87507315-88-3-119
- Sell KE, Verity TM, Worrel TW, Pease BJ, Wigglesworth J. Two measurement techniques for assessing subtalar joint positions: a reliability study. Journal of Orthopaedic sports Physical Therapy, 1994; 19: 162-168. DOI: 2519/jospt.1994.19.3.162
- Deng J, Joseph R, Wong CK. Reliability and validity of the sit-to-stand navicular drop test: Do static measures of navicular height relate to the dynamic navicular motion during gait? Journal of Students Physical Therapy Research, 2010; 2: 21-28.
- Muge Kirmizi, Mehmet Alphan Cakiroglu, P Ata Elvan, Ibrahim Engin Simsek, Salih Angin. Reliability of Different Clinical Techniques for Assessing Foot Posture; Journal of Manipulative and Physiological Therapeutics ;2020. DOI: 1016/j.jmpt.2020.02.002
- Juan Carlos Zuil Eschobar, Carmen Belen Martinez Cepa, Jose Antonio Martin Urrialde, Antonia Gomez Conesa. Medial Longitudinal Arch: Accuracy, Reliability, and Correlation Between Navicular Drop Test and Footprint Parameters; Journal of Manipulative and Physiological Therapeutics, 2018; 41(8). DOI: 1016/j.jmpt.2018.04.001
- Ji-Won Park, Jong-Sung Chang, Ki-Seok Nam. Reliability of Navicular Drop Measurements in Standing and Sitting Positions; The Journal Korean Society of Physical Therapy, 2010; 22(6): 29-33.
- Chun-Ming Yin, Xiao Hua Pan, Yu-Xin Sun, Zhi-Bin Chen. Effect of duration of wearing high-heeled shoes on plantar pressure; Human Movement Science, 2016; 49: 196-205. DOI: 10.1016/j.humov.2016.06.005

