A Histopathological Study of Upper GI Endoscopic Biopsy Specimens in Relation to Endoscopic Findings in North Bengal Population
Rupsha Dutta1, Sirshendu Pal2,* and Samrat Dutta3
1Assistant Professor, Department of Pathology, North Bengal Medical College and Hospital, India
2Senior Consultant Physician, Department of Medicine, Mitra’s Multispeciality Hospital, India
3Associate Professor, Department of Radiotherapy, North Bengal Medical College and Hospital, India
Received Date: 01/06/2023; Published Date: 06/10/2023
*Corresponding author: Sirshendu Pal, Senior Consultant Physician, Department of Medicine, Mitra’s Multispeciality Hospital, Siliguri, India
Abstract
The study was undertaken to compare the endoscopic and histopathological findings of upper GI lesions in North Bengal population. A total of 60 cases referred for upper GI endoscopy and biopsy were included in the study. The endoscopic findings were compared with the histopathological findings and on the basis of the histopathological diagnosis the lesions were characterized into neoplastic and non-neoplastic ones. The mean age of patients was 53.08 years. Male female ratio was 2.33:1. 80% of the lesions were in the stomach. Of the total 60 cases, 25 cases (41.67%) were non-neoplastic and 32 cases (53.33%) were neoplastic. Among the neoplastic, 3 cases (5%) were placed in the pre-malignant group and 29 cases (48.33%) in the malignant category. Gastritis was the commonest non-neoplastic lesion (52%) while gastric adenocarcinoma (75.86%) was the predominant malignant lesion. H. pylori could be demonstrated in 30.77% cases of gastritis. Gastritis and gastric polyp detection by endoscopy had high specificity but low sensitivity. For esophageal carcinoma, chronic duodenitis, tuberculosis of duodenum and duodenal ulcer, endoscopy had very high sensitivity and specificity. However, esophageal candidiasis and gastric lymphoma could not be diagnosed well with endoscopy. Occurrence of intestinal type of adenocarcinoma increased with age and the relation was statistically significant (p ≤ 0.002). There was significant association of gastric adenocarcinoma with urban residence (p ≤ 0.033), male sex (p ≤ 0.026) and tobacco addiction (p ≤ 0.033). Overall, in our study, the histopathological diagnosis corroborated the endoscopic diagnosis in 50 i.e 83.3% cases.
Keywords: Endoscopy; Biopsy; Gastritis; Gastric adenocarcinoma
Introduction
The upper GI tract is difficult to visualize. The development of fiberoptic endoscopes with cameras, monitors and video recorders have made data recordable, verifiable and comparable with similar findings in different patients. Endoscopic biopsy has made easy the histologic diagnosis of conditions like infections, erosions, inflammations, vascular abnormalities, peptic ulcers and malignancies. In fact, endoscopic biopsy has become mandatory for all lesions which are chronic and predisposed to malignancy.
The lining epithelium of the esophagus is non-keratinized stratified squamous in nature with mucus glands in its walls. The upper third contains striated muscles, the lower third contains smooth muscles and the middle third a mixture of the two [1]. Squamous papillomas are the most common benign esophageal epithelial neoplasms [2,3]. Leiomyomas, although the most common benign tumor of the esophagus seldom poses a clinical problem and appears as circumscribed mural masses or may even form pedunculated polyps [4]. Squamous cell carcinoma accounts for most cases of esophageal carcinoma worldwide [5]. The vast majority of gastric cancers are adenocarcinomas. Occasionally adenosquamous carcinomas [6] or pure squamous cell carcinomas are encountered. [7].
Common gastric complaints are usually due to gastritis and peptic ulcer disease [8]. An important association of chronic gastritis is with chronic infection by the bacillus Helicobacter pylori. The link was discovered in 1983 when the bacterium was called Campylobacter pyloridis [9]. Persons infected with H. pylori are at increased risk for the development of peptic ulcer disease, possibly gastric cancer [10] and gastric MALT lymphoma. There are very few references comparing endoscopic and biopsy findings of upper GI lesions in North Bengal population. The present study would therefore help in better diagnosis and management of such patients in North Bengal.
Aims and Objectives
- To study descriptions of gross pathology of the upper GI tract as described by endoscopists.
- To compare the endoscopic and histopathological findings of the upper GI tract lesions and to see whether these correspond.
- To help in the early detection of malignancies.
Materials and Methods
The study was conducted at North Bengal Medical College, Sushrutanagar, Darjeeling over a period of 1 year from July 2018 to June 2019.
Study Type:
It was a hospital based; cross-sectional, observational study based on evaluation of upper GI endoscopic biopsy specimens.
Study Population:
Patients attending the Surgery OPD with complaints localized to the upper GI tract referred for upper GI endoscopy and biopsy during the study period were selected.
Sample Size:
A total of 60 patients were selected after applying all the inclusion and exclusion criteria.
Inclusion Criteria:
- Only adult patients of either sex were considered due to lack of pediatric endoscopy facilities.
- All endoscopic procedures were carried out on awake, conscious and cooperative patients.
- Those patients were considered whose complete history and clinical data were available.
Exclusion Criteria:
- Patients with possibility of organ perforation.
- Patients who had severe cardio-respiratory problems or those with a poor general condition.
- Patients with gross skeletal deformity like severe kyphosis or scoliosis.
- Pregnant patients.
- Complete history and clinical data were lacking.
- Cases where the patient’s consent was not available.
For each patient a thorough history was taken and clinical examination done and filled up in a predesigned and pretested standard proforma. The endoscopic procedures were done with Fuzinon Fiberscope (FG-1Z). All suspicious areas were photographed and biopsied. The endoscopic biopsy specimens were subjected to histopathological examinations in the department of Pathology of North Bengal Medical College. After fixation and processing, sections were stained with Hematoxylin and eosin. Some sections were further stained by special stain PAS for fungus. Some were stained with ZN stain where tubercular etiology was suspected. Modified Giemsa stain was done for Helicobacter pylori.
For analysis all the data were entered in Microsoft Excel 2007 data sheet. Epi Info soft ware version 7 was used to calculate Chi-square for linear trend. Depending on the sample size, Chi- square test of association or the Freeman- Halton extension of Fisher exact probability test was used. To compare the endoscopic diagnosis with histopathologic diagnosis, criterion referenced validity study was done. Standard epidemiological indices for assessing validity of measures- sensitivity, specificity, positive predictive value and negative predictive values- were determined for the endoscopic diagnosis in comparison with the reference standard.
Results and Analysis
In our study group patients ranged from a minimum of 19 years to a maximum of 83 years with a mean age of 53.08 years. Majority of the patients were in the age group of 51-60 years. Male Female ratio was 2.33:1. Maximum number of males was seen in the age group of 61-70 years and females in 31-40 years. Mean age of male patients was 57.05 years and in females it was 43.83 years. Mean age in the non-neoplastic group was 49.64 while the mean age in the neoplastic group was 54.96 years. Maximum number of malignant lesions was in the 61-70 years age group while the non-neoplastic lesions were most common in the 51-60 years age group. 43.33% had rural background while urban cases contributed 56.67%.
Most lesions (80%) were located in the stomach. Of the total 60 cases of upper GI endoscopic biopsy specimens, 3 were categorized as non-specific as repeat biopsy was advised. 25 cases (41.67%) were categorized as non-neoplastic and 32 cases (53.33%) as neoplastic. Neoplastic cases were further sub-classified and 3 cases (5%) were placed in the pre-malignant neoplastic category and 29 cases (48.33%) were classified as malignant neoplastic.
Gastritis was the commonest non-neoplastic lesion accounting for 52% cases followed by gastric ulcer. Majority of patients with gastritis were in the age group of 51-60 years. Gastric adenocarcinoma constituted the largest proportion (75.86%) of malignancies. Majority of the non-neoplastic (76%) and neoplastic (82.76%) lesions were in the stomach. Male predominance was found both in neoplastic and non-neoplastic lesions.
H.pylori could be demonstrated in 30.77% cases of gastritis, 33.33% cases of gastric ulcer and upto 50% cases of duodenal ulcer.
80% cases of esophageal carcinoma were of squamous cell variety and the most common site was distal third of esophagus. Maximum number cases of gastric adenocarcinoma (82.60%) were found in the prepyloric and antral region of the stomach. Intestinal type of adenocarcinoma constituted 60.87% cases while diffuse type of adenocarcinoma constituted 39.13% cases. Males constituted 56.52% of gastric adenocarcinoma cases while females constituted 43.48% cases. Male female ratio was 1.3:1 for gastric adenocarcinoma. Most of gastric adenocarcinoma patients were from urban areas (73.91%). Males predominated in both urban and rural areas. Maximum number of gastric adenocarcinoma cases occurred in the 61-70 years age group. Most number of diffuse types of gastric adenocarcinoma cases occurred in the 31-40 years age group while intestinal type of gastric adenocarcinoma occurred in the 61-70 years age group. Thus, it is evident that intestinal type of adenocarcinoma is increasing with age and the relation is statistically significant (p≤0.002). Males predominantly presented with intestinal variety of adenocarcinoma (78.57%) in comparison to females (21.43%) in whom the diffuse variety was more common. This was statistically significant (p≤0.026). A significant association was present between adenocarcinoma and urban residence (p ≤ 0.033). There was a significant association between gastric adenocarcinoma and tobacco addiction (p≤ 0.034). However, there was no significant association between gastric adenocarcinoma and alcohol intake.
Criterion-reference validity taking histopathology as gold standard showed that the sensitivity of endoscopic diagnosis was very high for certain lesions like Barrett’s esophagus, esophageal carcinoma, gastric carcinoma, gastric ulcer, chronic duodenitis and tuberculosis of the duodenum while in other cases like gastric polyp and gastritis, the sensitivity was low and the specificity high.
Table 1: Distribution of Non-Neoplastic Lesions as Diagnosed by Histopathological Examination.

In the present study, it was observed that gastritis was the commonest non-neoplastic lesion accounting for 52% cases. The next predominant lesion was gastric ulcer.
Table 2: Distribution of Malignant Lesions as Diagnosed by Histopathological Examination.
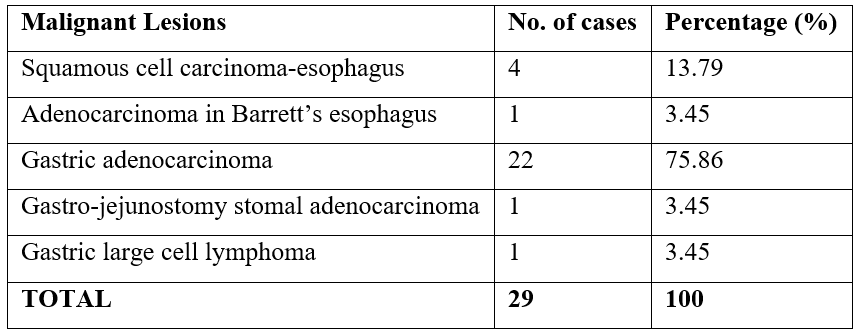
In the present study, it was observed that gastric adenocarcinoma constituted the largest proportion (75.86%) of malignant lesions.
Discussion
Age Distribution:
In our study age range of patients varied from 19-83 years with a mean of 53.08 years and S.D of 15.07. Sultana et al [11] in their study on 105 cases in Bangla Desh, showed the mean age to be 54.66 years and the age-range to be 28-90 years. Sandhya Panjeta Gulia et al [12] in their study on 192 patients at Puducherry, India reported the age range to be within 19-75 years. In the study conducted by Sulieman M et al [13] on 1607 cases in Saudi Arabia, the mean age was 48.5 years, S.D was 18 and the age range 15-100 years. Thus, the mean age in our study was closest to that conducted by Sultana et al.
Sex Distribution:
In the present study, out of 60 patients, 42 were male and 18 females. Male female ratio was 2.33:1. In the study conducted by Sultana et al [11] on 105 cases, 76 were male (72.3%) and 29 were female (27.6%). Male female ratio was 2.6:1. Hussein Youssif Adam et al [14] found a male predominance in their study with males constituting 57% and females 43%. In all these studies including ours, there was a male predominance. This may be due to the fact that males have a better access to health care facilities than females. Also, males are more addicted to tobacco, alcohol, etc which predispose them to various GI pathologies. Moreover, males also face a more hostile environment outside compared to the congenial atmosphere at home experienced by females. These stressful situations may lead to acid peptic disorders.
Rural – Urban Distribution:
Rural cases constituted 43.33% of the study population whereas urban cases constituted 56.67%. Out of 26 cases from rural areas 20 were male and 6 were female whereas out of 34 urban cases 22 were male and 12 females. Thus, urban people are more health conscious and have better access to health care facilities. Rural females are less stressed, consume less fast-food products, have a high fiber diet and have less access to health care facilities, thus contributing the least number of cases.
Anatomic Distribution of Lesions:
Most lesions (80%) were located in the stomach. Hussein Youssif Adam et al [14] also found maximum number of lesions in the stomach as did Sandhya Panjeta Gulia et al [12] who found stomach accounted for 84.89% cases.
Categorization of Lesions according to Nature:
In our study 25 cases (41.67%) were non-neoplastic while 32 cases (53.33%) were neoplastic. 3 cases were categorized as non-specific lesions and re-biopsy suggested. The study by Sultana et al [11] had 59% neoplastic lesions and 40% non-neoplastic lesions and 1% was normal. P. Karthic et al [15] reported 50% as non-neoplastic and 44% as neoplastic while 6% were normal. In the study by Nafees a Qureshi et al [16] 58% cases were non-neoplastic and 32% were neoplastic while 10% were normal.
Neoplastic lesions were the majority in our study similar to the study by Sultana et al [11]. However, this was contrary to the findings of most of the studies. The primary cause of this discrepancy was that we selected cases where biopsy was done and biopsy is usually done where malignancy is suspected. Moreover, we mostly dealt with referred cases.
Non-neoplastic Lesions by Histopathology:
In our study, gastritis the major non-neoplastic lesion accounted for 52% cases. 12% cases were of gastric ulcer. Gastric polyps, duodenal ulcer and tuberculosis of duodenum each constituted 8% of cases. Esophageal candidiasis, Menetrier’s disease and chronic duodenitis each constituted 4% of cases. In the study by Sultana et al [11] the most common non-neoplastic lesion was gastritis which constituted 84.78% of non-neoplastic lesions. Shaheen A. Bhatty et al [17] also had the most common non-neoplastic lesion as gastritis. Our finding of gastritis being the major non-neoplastic lesion was consistent with the studies of Sultana et al [11] and Bhatty et al [17].
Malignant Lesions by Histopathology:
In our study, there were 5 cases of esophageal carcinoma, 22 cases of gastric adenocarcinoma, 1case of gastr-jejunostomy stomal adenocarcinoma and 1 case of gastric lymphoma. In the study by Sandhya Panjeta Gulia et al [12] out of 192 cases of endoscopic biopsy, 12 cases had malignant neoplastic lesions of which 9 were gastric adenocarcinoma. P. Karthic et al [15] in the study on 100 patients found 44 cases to have neoplastic malignant lesions of which 42 were of gastric adenocarcinoma. Thus, our study matched the studies of Sandhya Panjeta Gulia et al [12] and P.Karthic et al [15].
Anatomical Distribution of Non-neoplastic Lesions:
Majority of non-neoplastic lesions (76%) were located in the stomach followed by lesions in the duodenum and esophagus respectively. Sandhya Panjeta Gulia et al [12] found most (153/168) of the non-neoplastic lesions to be located in the stomach followed by lesions in the esophagus and duodenum respectively. Hussein Youssif Adam et al [14] also found the stomach lesions to be the commonest non-neoplastic lesions followed by esophagus and duodenum. The findings of our study corroborate with the other studies showing stomach as the commonest site.
Anatomical Distribution of Malignant Lesions:
Maximum number of malignant lesions (24/29) was found in the stomach followed by the esophagus. No malignant lesion was found in the duodenum. Gastric malignancy accounted for 40 % of all cases. Sandhya Panjeta Gulia et al [12] in the study on 192 cases found 10 cases of stomach malignancy and 2 cases of esophageal malignancy. There was no case of malignancy in the duodenum. P. Karthic et al [15] reported 44 cases of gastric carcinoma among 100 patients (44%). No cases of esophageal or duodenal carcinoma were reported. Shaheen A. Bhatty et al [17] reported 49 cases of esophageal carcinoma and 20 cases of gastric carcinoma among 1046 cases. The findings of our study were similar to the studies of Sandhya Panjeta Gulia et al [12] and P. Karthic et al [15]. In all studies no malignant lesion was found in the duodenum.
There was male predominance in both neoplastic and non-neoplastic lesions.
Age Distribution of Neoplastic and Non-neoplastic Lesions:
Malignant lesions were maximum in the 61-70 years age group while non-neoplastic lesions were maximum in the 51-60 years age group. Mean age in the non-neoplastic group was 49.64 years while that in the neoplastic group was 54.96 years. In the study by P. Karthic et al [15] most of the malignant neoplastic lesions were in the 51-70 years age group.
Age and Sex Distribution of cases with Gastritis:
Majority of the patients with gastritis were in the 51-60 years age group. Minimum age was 19 years and mean age 49 years. Males were predominant. In the study by Tzeng et al [18] the mean age was 53.1+ 10.5 years while for Roar Johnsen et al [19] it was 60-69 years and for Atisook K et al [20] it was 31-60 years. Thus, the mean age of our patients was close to the study by Tzeng et al [18].
Distribution of Helicobacter pylori in non-neoplastic lesions:
H. pylori could be demonstrated in 30.77% of gastritis, 33.33% of gastric ulcers and 50% of duodenal ulcers. Shaheen A. Bhatty et al [17] found H. pylori in 37.3% of gastritis while Seed Afzal et al [21] in 70.2% cases and Hamamatul Bushra Khan et al [22] in 81% cases. Our study was close to the study by Shaheen A. Bhatty et al [17] while others had a much higher percentage. Our low positivity may be due to the frequent use of H2 blockers, proton pump inhibitors and antibiotics. Moreover, we used only modified Giemsa stain to demonstrate H. pylori.
Distribution and Histologic Types of Esophageal Carcinoma:
80% cases of esophageal carcinoma were of squamous variety. The most common site was the distal third. In the study conducted by A. Alidina et al [23] Squamous cell carcinoma was noted in 81% cases and the most common site was the lower esophagus (52%). Jose Tony et al [24] also reported Squamous cell carcinoma to be the commonest type (71%). Malignancy of the lower third constituted 55.5%. Thus, our study closely matched the other studies.
Distribution and Histologic Types of Gastric Carcinoma:
Out of 60 cases, 23 cases (38.33%) presented with gastric carcinoma. Maximum number of gastric adenocarcinoma (82.6%) was found in the pre-pyloric and antral region. Intestinal type of adenocarcinoma was the predominant type (60.87%) while diffuse type constituted only 39.13% cases. Pavithran K et al [25] also reported the intestinal type to be more common than the diffuse type. Cherian et al [26] reported the commonest site as antrum (67.3%) followed by the body (23.3%). Thus, our study was similar to other studies.
In our study as well as that of Mans et al [27] GI malignancy was more common in the urban population perhaps due to life style changes.

Figure 1
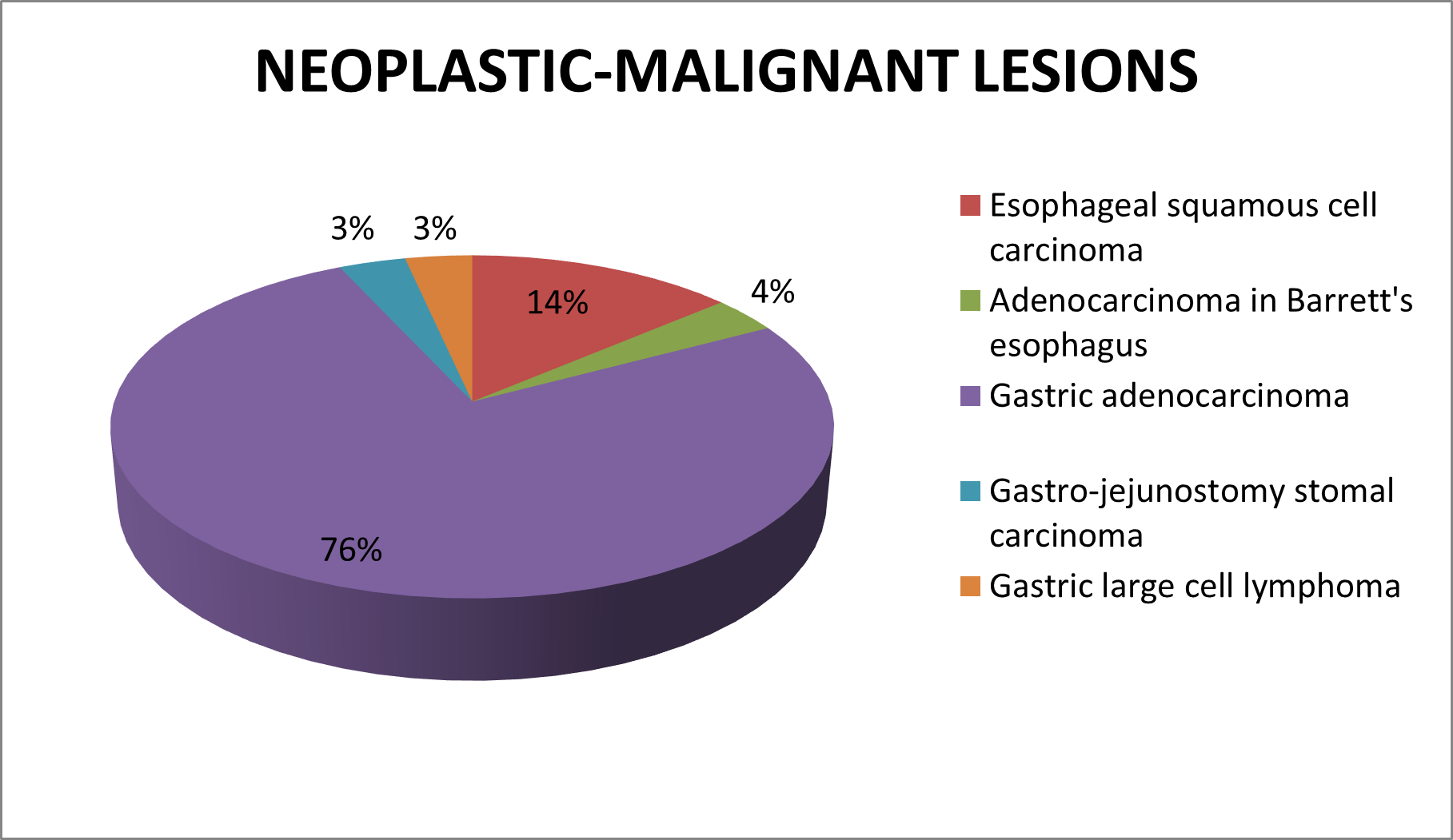
Figure 2
Age Distribution of Gastric Adenocarcinoma:
In our study maximum number of gastric adenocarcinomas occurred in the 61-70 years age group. Diffuse type of adenocarcinoma occurred mostly in the 31-40 years age group while intestinal type in 61-70 years age group. Female predominance was seen in diffuse type of adenocarcinoma as was also observed by Mohar et al [28]. Wu et al [29] showed peak incidence of gastric cancer in the 65-74 years age group. Thus, our findings are similar to other studies.
Association of males with Intestinal variety of Gastric Adenocarcinoma:
It was seen that males (78.57%) predominantly presented with intestinal variety in comparison to females (21.43%) and the difference was statistically significant. Mohar et al [28] reported similar findings.
Association of Gastric Adenocarcinoma with Urban Residence:
73.91% cases of gastric adenocarcinoma were associated with urban residence and this association was statistically significant.
Association of Gastric Adenocarcinoma with Tobacco:
We found a statistically significant association of Gastric Adenocarcinoma with tobacco addiction (73.9%). Ponnala et al [30] in their study from Hyderabad also showed a significant association of tobacco with gastric adenocarcinoma.
Association of Gastric Adenocarcinoma with Alcohol:
No significant association was found between gastric adenocarcinoma and alcohol intake (26.09%). P. Karthick et al [15] showed that only 22.73% cases of gastric adenocarcinoma were alcoholic but Ponnala et al [30] showed a significant association.
Comparison between Endoscopic (Provisional) and Histopathological (Final) Diagnosis:
In our study, histopathological diagnosis was considered the gold standard. Esophageal candidiasis and gastric lymphoma could not be diagnosed correctly by endoscopy, suggesting fallacy of endoscopy in detecting such lesions. Gastritis and gastric polyp detection by endoscopy had a very high specificity but low sensitivity while endoscopy had a very high sensitivity and specificity in detecting lesions like esophageal carcinoma, chronic duodenitis, tuberculosis of duodenum and duodenal ulcer, thus having accuracy matching that of histopathologic examination. Upper GI endoscopy proved to be a good screening technique for lesions like gastric adenocarcinoma and gastric ulcer where the sensitivity was very high but histopathology remained the mainstay of final definitive diagnosis. Sultana et al [11] also showed a high sensitivity of endoscopy in detecting gastric carcinoma while a high specificity in detecting gastritis.

Figure 3: (a) Fundal Gastritis (Endoscopic image) (b) Helicobacter pylori gastritis (Modified Giemsa 1000X).
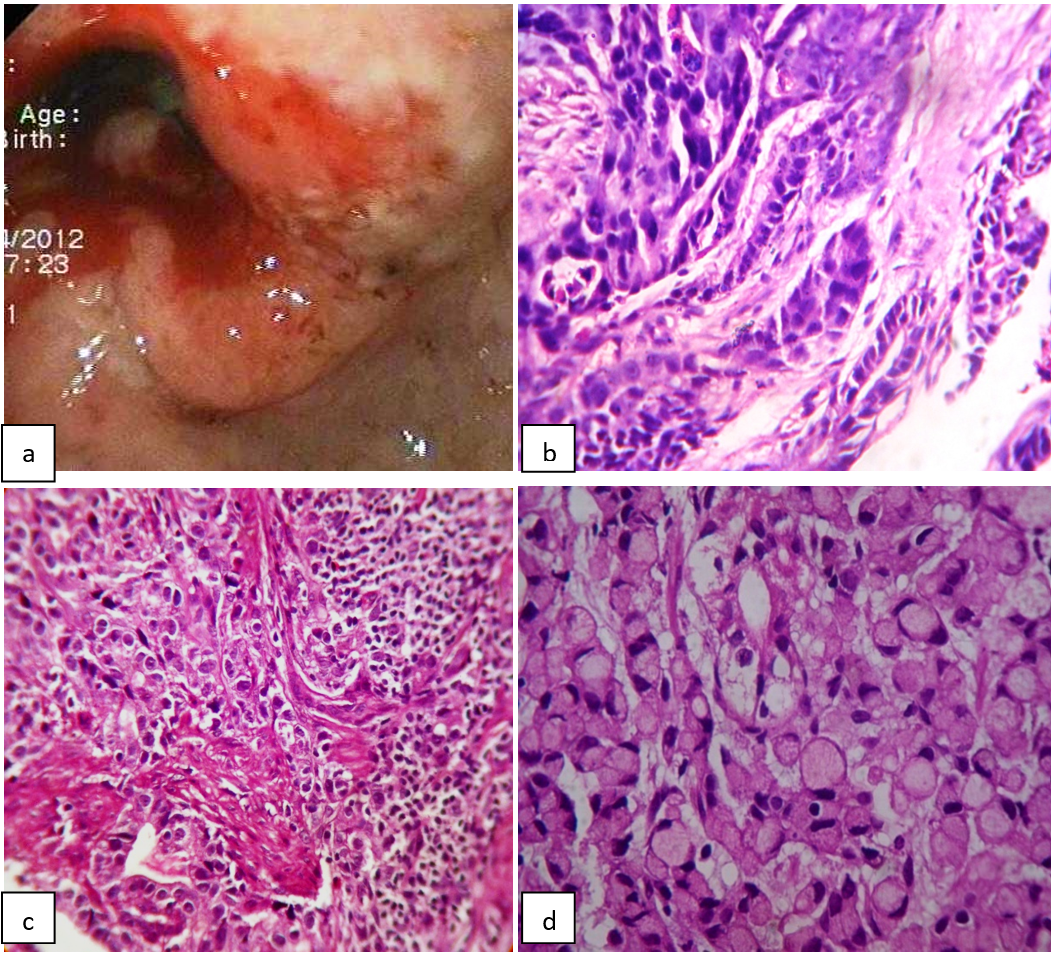
Figure 4: (a)Ulcerated Antral growth? Malignant (Endoscopic Image) (b) Intestinal type of Adenocarcinoma (H&E 400X) (c) Infiltrating Diffuse adenocarcinoma (H&E 400X) (d) Signet Ring type of Adenocarcinoma (H&E 400X).
Conclusion
In our study, an attempt was made to compare the endoscopic diagnosis with the histopathologic diagnosis and on the basis of the histopathologic diagnosis, the lesions in the upper GI tract were categorized into neoplastic and non-neoplastic ones. While gastritis was the commonest etiology in the non-neoplastic group, gastric adenocarcinoma was the commonest in the malignant neoplastic one. Prevention of smoking can significantly reduce the development of gastric adenocarcinoma in the North Bengal population. Histopathologic diagnosis corroborated with the endoscopic diagnosis in 83.33% cases. Upper GI endoscopy proved to be a good screening technique for lesions like gastric adenocarcinoma and gastric ulcer where the sensitivity was very high but histopathological examination remained the mainstay of final definitive diagnosis.
Limitations
This was a cross-sectional study conducted in a single institution in North Bengal over a period of 1 year. The study sample was small in comparison to the magnitude of the problem. A multicentric population-based study on a large sample is required for better correlation of results. A prospective long term follow-up study should be conducted to obtain more precise results and validation of conclusions of the present study. Special stains like Warthin Starry, Gimenez or Gram stain was not done for better demonstration of H. pylori. Due to non availability of these stains only modified Giemsa was used. We have also not performed Biopsy Urease test or Anti H. pylori IgG ELISA for demonstration of H. pylori.
References
- De Nardi FG, Riddel RH. The normal esophagus. Am J Surg Pathol, 1991; 15: 296.
- Odze R, Antonioli D, Shocket D, et al. Esophageal squamous papillomas. A clinicopathological study of 38 lesions and analysis for human papilloma virus by the polymerase chain reaction. Am J Surg Pathol, 1993; 17: 803-812.
- Lavergne D, de Villiers EM. Papilloma virus in esophageal papillomas and carcinomas. Int J Cancer, 1999; 80: 681-684.
- Mutrie CJ, Donahue DM, Wain JC, et al. Esophageal leiomyoma: a 40-year experience. Ann Thorac Surg, 2005; 79: 1122- 1125.
- Yerian LM, Goldblum JR. Esophagus. In, Mills SE (ed). Sternberg’s Diagnostic Surgical Pathology. Philadelphia, Lippincott Williams & Wilkins, 2010; 2(5): 1264.
- Mori M, Fakuda T, Enjoji M. Adenosquamous carcinoma of the stomach histogenetic and ultrastructural studies. Gastroenterology, 1987; 92: 1078-1082.
- Ruck P, Wehrman M, Campbell M, et al. Squamous carcinoma of the gastric stump: a case report and review of the literature. Am J Surg Pathol, 1989; 13: 317- 324.
- Sandler RS, et al. The burden of selected digestive diseases in the United States. Gastroenterology, 2002; 122: 1500.
- Moss SF, Sood S. Helicobacter pylori. Curr Opin Infect Dis, 2003; 16: 445.
- Blaser MJ, Atherton JC. Helicobacter pylori persistence: biology and disease. J Clin Invest, 2004; 113: 321.
- Sultana A, Badruddoza SM, Rahman F. Correlation between Endoscopic and Histological Findings in Different Gastroduodenal Lesion and its Association with Helicobacter pylori. AKMMC J, 2011; 2: 6-10.
- Gulia SP, Chaudhury M, Noorunnisa N, Balakrishnan CD, Balagurunathan K. Interpretation of Upper GI Tract Endoscopic Mucosal Biopsies- A Study Conducted in Teaching Hospital in Puducherry, India. International Journal of Medical and Health Sciences, 2012; 1: 17-24.
- Sulieman M, Al Humayed, Ahmed K. Mohamed Elbagir, Abdelhamid A. Al-Wabel, Yahya A. Argobi. The Changing Pattern of Upper GI Lesions in Southern Saudi Arabia: An Endoscopic Study. The Saudi Journal of Gastroenterology, 2010; 16(1): 35-37.
- Adam HY, Doumi EBA. Upper GI Endoscopy in El Obeid, Western Sudan: Analysis of the first 1150 cases. Sudan JMS, 2008; 3: 91-95.
- Karthick P, Rajachidambaram K, Sowmya TK, Natarajan RM. Incidence of Stomach Carcinoma in patients with Acid-Peptic Disease in Rural Hospital. The Internet Journal of Health, 2012. DOI:10:5580/2a75.
- Qureshi NA, Hallissey MT, Fielding JW. Outcome of Index Upper Gastrointestinal Endoscopy in Patients presenting with Dysphagia in a Tertiary Care Hospital- A 10 years review. BMC Gastroenterology, 2007; 7: 43.
- Bhatty SA, Shaikh NA, Zahir N, Akhter SS, Vaswani AS, Manzoor H. Histopathologic Spectrum of Upper Gastrointestinal Endoscopies. Medical Channel, 2009; 15: 11-14.
- Tzeng JE, Lin YL, Chung SM, Chu YT. Comparison of Four Diagnostic Methods for Helicobacter pylori. Tzu Chi Med J, 2005; 17: 339-343.
- Johnsen R, Bernersen B, Straume B, Forde OH, Bostad L, Burhol PG. Prevalences of endoscopic and histological findings in subjects with and without dyspepsia. BMJ, 1991; 302: 749-752.
- Atisook K, Kachinthorn U, luengrojanakul P, Tanwardee T, Pakdirat P, Puapairoj A. Pubmed: Helicobacter, 2003; 8(2): 132-141.
- Afzal S, Ahmad M, Mubarik A. Morphological spectrum of gastric lesions-endoscopic biopsy findings. Pakistan Armed Forces Medical Journal, 2006; 56: 143-149.
- Khan HB, Umar M, Khurram M. Endoscopic and Histopathological Evaluation of 306 Dyspeptic Patients. Pak J Gastroenterol, 2003; 17: 4-7.
- Alidina A, Gaffar A, Hussain F, Islam M, Vaziri I, Burney I, et al. Survival Data and Prognostic Factors seen in Pakistani Patients with Esophageal Cancer. Annals of Oncology, 2004; 15: 118-122.
- Tony J, Kumar SK, Thomas V. Time trends and pathological profile of carcinoma lower esophagus and gastro-esophageal junction over the last 20 years- an experience from South India.
- Pavithran K, Doval DC, Pandey KK. Epidemiological note: Gastric Cancer in India. Gastric Cancer, 2002; 5: 240-243.
- Cherian JV, Sivaraman R, Muthusamy AK, Venkataraman J. Stomach Carcinoma in the Indian Sub-continent: A 16-year trend. The Saudi Journal of Gastroenterology, 2007; 13: 114-117.
- Mans DRA, Rijkaard E, Dollart J, Belgrave G, Joe A, Matadin R, et al. Difference between Urban and Rural Areas of the Republic of Suriname in the Ethnic and Age Distribution of Cancer- A Retrospective Study from 1980 through 2004. The Open Epidemiology Journal, 2008; 1: 30-35.
- Mohar A, Suchil BL, Hernandez GA, Podolsky RI, Herrera GR, Mora TA, et al. Intestinal type: diffuse type ratio of gastric carcinoma in a Mexican population. J Exp Clin Cancer Res, 1997; 16(2): 189-194.
- Wu CW, Tsay SH, Hsieh MC, Lo SS, Lui WY, P’eng FK. Clinicopathological significance of intestinal and diffuse type of gastric carcinoma in Taiwan Chinese. J Gastroenterol Hepatol, 1996; 11: 1083-1088.
- Ponnala D, Madireddi S. Evaluation of risk factors for gastric cancer. Int J Appl Biol Pharm Technol, 2010; 1; 158-161.

