Antibacterial Agents: Knowledge and Attitudes of Sudanese College of Medicine Undergraduates
Abdelwahid Ali Abdelwahid Mohamed1, Mohammed Ahmed Ibrahim Ahmed2,*, Gwahir Ebrahim Osman IbnIdriss3,Areej Ali Ahmed1,#, Ali Hussain Alsadig1,#, Israa Muhammed1,#, Hanaa Atif Elfaki1,#, Mohamed Ahmed1,#, Ahmed Mohamed Ebnouf1,#, Nahla Ahmed Mohammed Abdelrahman4, Sohep Abdalla Osman5 and Isam Eldeen Eltayeb Osman Ali6
1Assistant professor of Microbiology, El-Razi University, Faculty of Medicine, Khartoum, Sudan
2Assistant professor of Microbiology, Nile Valley University, Faculty of Medicine, Sudan
3Assistant professor of Internal Medicine, National University, Faculty of Medicine, Sudan
1,#House officer of Medicine and Surgery, El-Razi University, Faculty of Medicine, Khartoum, Sudan
4Assistant professor of Biochemistry, Nile Valley University, Faculty of Medicine, Sudan
5Assistant professor of Internal Medicine, Endocrinologist, Elsheikh Abdallah Elbadri University-Faculty of Medicine, Sudan
6Assistant professor of Internal Medicine, Cardiologist, Ministry of Health, Sudan
Received Date: 24/05/2023; Published Date: 19/09/2023
*Corresponding author: Dr. Mohammed Ahmed Ibrahim Ahmed, Assistant professor of Microbiology, Nile Valley University, Faculty of Medicine, Medical officer, Atbara, Sudan
Abstract
Background: Animal and human health depend on antimicrobials. Following the introduction of a new antimicrobial agent, drug resistance to that antimicrobial agent emerges. Evidence demonstrates that the public is crucial to the challenge, expansion, and spread of antibacterial resistance. This study aimed to assess the knowledge, attitudes, and practices of medical students of El-Razi University regarding antimicrobial use and resistance.
Study objective: The intention of this study was to recognize the medical students at El-Razi University's awareness, perceptions, and practices regarding the use and resistance of antibiotics 2022.
Methods: On 292 randomly chosen medical students, a cross-sectional descriptive study using a pretested semi-structured questionnaire was conducted from October to November 2022. The statistics were explored using the chi-square and descriptive tests, and results were presented on tables.
Result: A total of 292 participants filled out the questionnaire and handed it back, granting us a 100% response rate. The respondents' median age was 24 years. Sixty-one percent (178) of the respondents were women, and 81.2% of them were Sudanese (237). All of the participants were undergrads in medicine. The statistical analysis also realized a positive link between respondents' awareness of antimicrobial attitudes and resistance. Around 83.6% of participants are knowledgeable of antimicrobial resistance (244). Approximately 85.3% (249) agreed that one of the major contributing factors to the emergence of bacterial organisms resistant to drugs is antibacterial misuse. Of the participants, about 34.4% (100) claimed to use antibiotics with a medical recommendation, while about 59.6% (174) accepted purchasing medications from a pharmacy without a prescription.
Conclusion: Antimicrobial resistance and its mishandling in diverse fields were issues on which participants' attitudes and awareness were better than average, but there is still much opportunity for improvement.
Keywords: Antimicrobial Resistance; Khartoum; Sudan
Introduction
Antimicrobial resistance, according to the World Health Organization, is the ability of microorganisms to withstand the effects of antibiotics that have been used to treat their infections. Standard treatments are habitually ineffective when microorganisms develop resistance to antibiotics, and in some cases, no medicines provide an effective treatment. Treatments consequently fail. Antibiotics, antivirals, antifungals, and antiparasitic are different forms of antimicrobials that are drugs used to prevent and treat infections in humans, animals, and plants [1]. Worldwide, resistant bacteria and other microbes are also rapidly emerging, jeopardizing the effectiveness of antibiotics, which have revolutionized medicine and prevented millions of deaths [2]. The protection and significance of many emergencies’ medical procedures, such as operations, organ transplants, etc (Success is measured by a drug's capacity to prevent pathogenic bacteria from developing resistance) [3,4]. Any type of microbe can become resistant to medication. Antibiotic, antifungal, antiviral, and parasite resistance are consequences [5].
Antimicrobial resistance was primarily responsible for 1.27 million fatalities globally in 2019.One in five children under five died from antimicrobial resistance, and antimicrobial resistance may have been a major consideration in five million deaths [6] Antimicrobial resistance thus has pessimistic implications for both the health and economic sectors in both developed and developing countries [7]. A condition in which the body becomes more susceptible to disease and then treatment becomes challenging as pathogens develop immunity to the frequently taken antimicrobial drugs often results from the resistance developing naturally over time, typically through genetic changes derived from subpar infection control practices, neglected use of antimicrobials, and persistent rejection of warnings about overuse of medications [8] and self-medication as a result of the expensive healthcare system [9], which relates to clinical negligence on the part of medical staff. Other attributes encompass intensive agricultural use, epidemics, disinfectants, healthcare systems because of excessive antimicrobial use during those times, environmental pollution, improper disposal of unused or expired medications, and a lack of knowledge, initiatives, and awareness regarding best practices that can result in excessive or inappropriate use [10].
Regrettably, the negligent use of these medications is ending their miraculous effects. Due to the increased number of hospitalizations around the world, often in Sudan, the rapid development of resistance is to blame for thousands of deaths and economic difficulties [11]. The majority of medications, including antibiotics and antimalarials, can be purchased at neighborhood pharmacies in Sudan without a prescription, though there are laws that classify medications as either prescription-only or appropriate for over-the-counter sale [12]. The seriousness of the problem is demonstrated by the numerous studies conducted in Sudan that have encountered elevated incidences of the emergence of resistant strains in a variety of pathogens.
Evidence showed that 3rd generation cephalosporin resistance was present in 90% to 100% of Enterobacteriaceae isolates in Ibn Sine Hospital during the Sudanese years 2008 to 2010, 78% and 80% of E. coli and K pneumonia, respectively, were ESBL producers, 51% of Staph aureus was MRSA, and the prevalence of vancomycin-resistant enterococcus ranged from 21% in Soba Hospital to 33% at the National Health Laboratory [11].
Methodology
Study design, area, and population:
Between October and November 2022, a cross-sectional descriptive study involving 292 members of Elrazi University's medical faculty took place. Elrazi University was established in 2001 on 35,000 square meters in Al-Azhari Town (Square 2) in Khartoum State. There are currently eight colleges there, and 1264 students are enrolled in the medical school.
Data collection technique:
Gathers information using self-administered structured questionnaires that the author pre-tested and created with particular objectives. Statistics on respondents' personal characteristics, knowledge of antibiotics, and familiarity with particular medications, like those used to treat malaria, were gathered using the questionnaire. The data were examined using the social sciences statistical package (SPSS version 21).
Ethical Consideration:
The Department of Community Medicine at Elrazi University awarded their authorization. The medical students' consent was obtained after they were notified of the study's aims and asked to answer a questionnaire. The questionnaire will not contain any participant identities or other data that could be used to identify them. To protect their privacy and confidentiality, each participant will receive an anonymous questionnaire. The questionnaire is made to be finished quickly so that it won't take up too much of the respondents' time.
Result
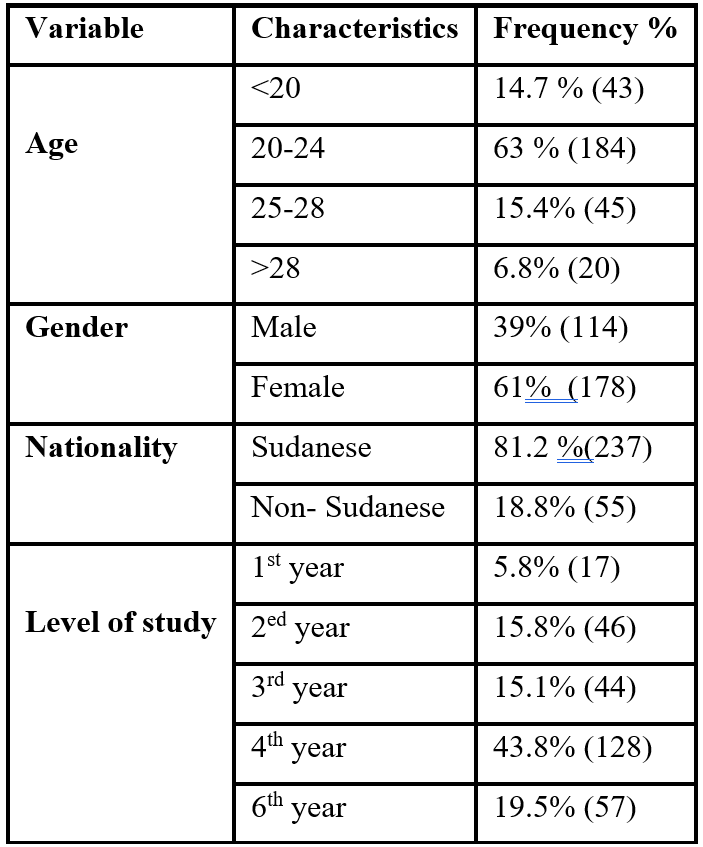
A total of 292 participants completed the questionnaire and returned it, making the response rate 100%. The respondents' average age was 24 years. 61% (178) of the respondents were female, and 81.2% of them were Sudanese (237) (Table 1).
Table 1: Descriptive data of the study population.
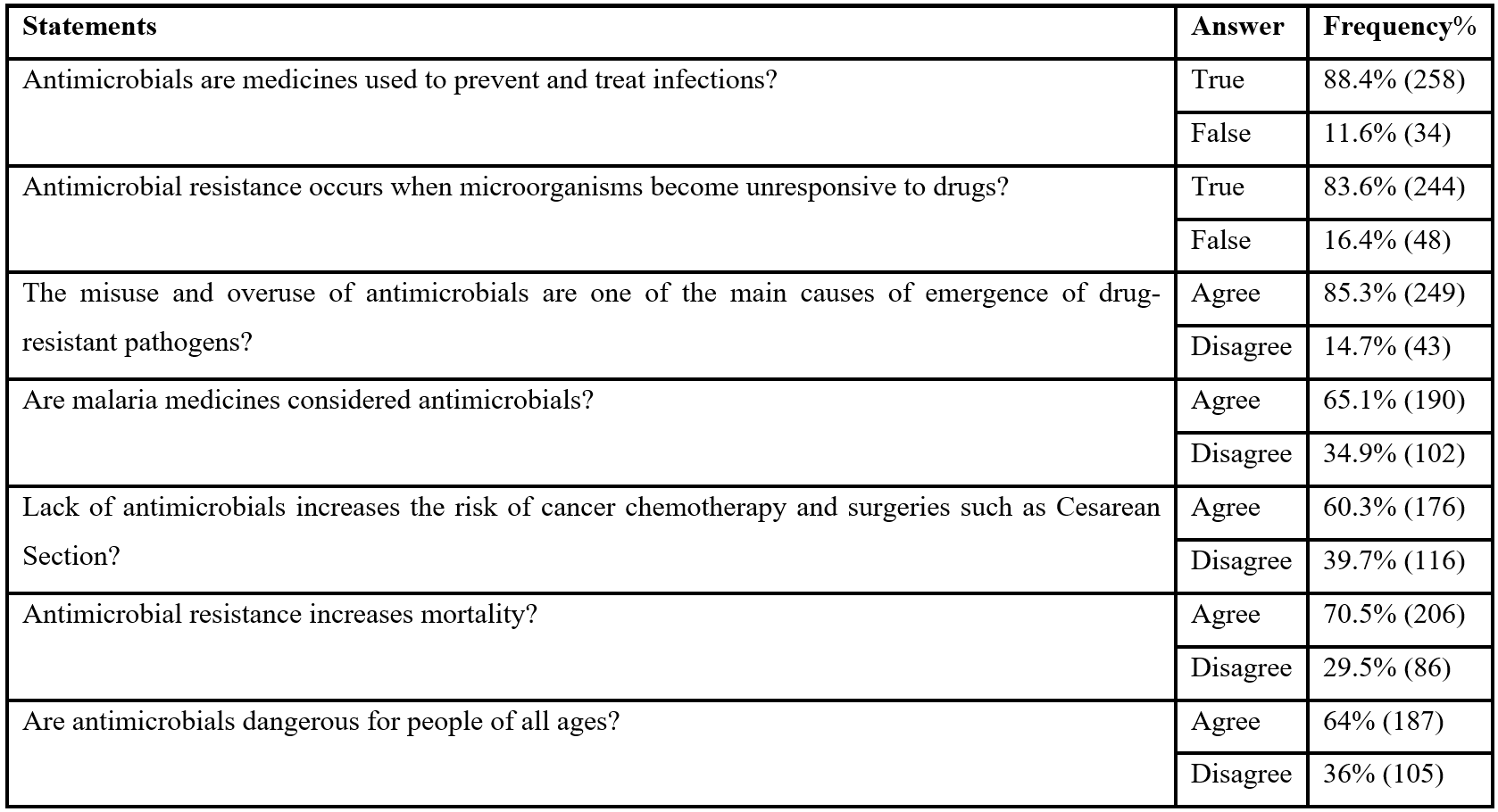
Knowledge of antimicrobial resistance:
88.4% (258) of the respondents were aware of the advantages of antibiotics; 83.6% (244) of them demonstrated knowledge of how microorganisms develop resistance to antibiotics, while 16.4% (48) did not.85.3% (249) concurred that one of the primary causes of the emergence of pathogens with drug resistance is the misuse of antibiotics. 39.7% (116) of the participants did not have a thorough understanding of the negative effects of antimicrobial resistance. 86 out of 29.5% do not believe it can be fatal. 64% (187) were not of the opinion that it can't affect all ages, compared to 36% (105) of participants (Table 2).
Table 2: Knowledge of antimicrobial resistance.
Attitudes toward antimicrobial resistance:
Antimicrobial course completion commitment was extremely high. 65.8% (192) of them, but 34.8% (100) of them believe that skipping one or two doses won't have an impact. Regretfully, 59.6% (174) of the participants want to be able to purchase medications from a pharmacy without a prescription, and 34.4% (100) of the participants agreed that antimicrobial drugs could be taken without consulting a doctor. A sizable portion of the participants—a whopping 47% (140)—kept some antimicrobial medications at home in case they were needed, and many of them used them for minor illnesses. 44.2% (129) (Table 3).
Table 3: Attitudes toward antimicrobial resistance.

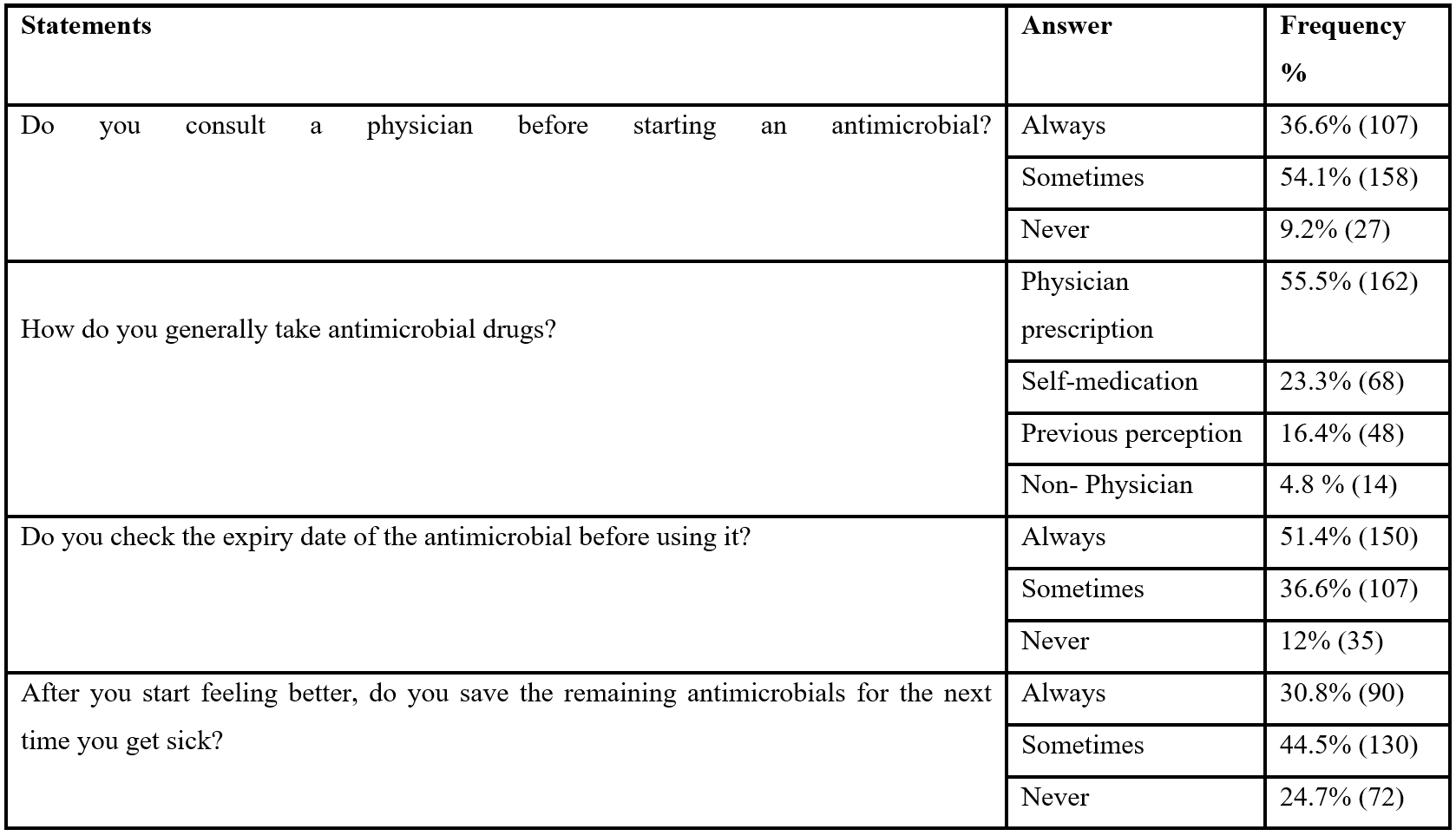
Practice toward antimicrobial resistance:
A significant proportion of participants—36.1% (107) always, 54.1% (158) occasionally, and 9.2% (27) never—began using antimicrobial drugs without first consulting a doctor, 5.8% (14) use non-physician perception, 16.4% (48) use prior perception, 23.3% (68) use self-medication, and 55.5% (162) use prescription drugs from a physician. 51 percent (150) of the participants checked the expiration dates, 12% (48) never did so, and 36.6% (107) occasionally did so. When they start feeling better, some participants save the remaining medication, with 30.8% (90) always doing so, 44.5 (130) occasionally doing so, and 24.7 (72) never doing so (Table 4).
Table 4: Practice toward antimicrobial resistance.
Discussion
Numerous studies have stated that students in medical and non-medical colleges misuse antibiotics, self-medicate, and have inadequate antibacterial agent awareness. In the present study, we noticed that 83.6% (244) of respondents have awareness of how microorganisms develop resistance to antimicrobial drugs, but conversely, a study that was accomplished at the University of Brunei Darussalam (UBD) in 2020 with the intent to assess antibiotic usage and information concerning antibiotics and antimicrobial resistance among undergraduate students.
The study's findings show that while there is a good level of knowledge regarding the utilization of antibiotics, there is still some considerable uncertainty, particularly in the section about when to use antibiotics appropriately for various disease conditions because some individuals do not respond to antibiotic therapy for viral conditions. Contrary to our most recent report, the population of University Brunei Darussalam emerged from both private and public healthcare facilities [13].
In our report, we unearthed that 85.3% (249) agreed that one of the chief reasons that drug-resistant pathogens arise is attributable to the improper use of antibiotics. Likewise, devotion to completing the antibiotic regimen was remarkably increased (65.8% / 192), but 34.8% (100) of them assumed that ditching one or two doses wouldn't have major implications. Whilst the majority of those who participated were cognizant of the use of antibiotics and formations of awareness and good practices, their outcomes from a cross-sectional, anonymous online survey that sought to assess these aspects indicated that respondents had negative perceptions toward antibiotic use despite the reality that they broadly had optimistic information and concepts [14].
55.5% (162) of the respondents in our study used medicines that were ordered by their doctors. Participants use antimicrobials that were previously prescribed to them and self-medicate. To figure out the incidence of self-medication with antibacterial agents and/or antimalarial drugs among university graduates in Sudan, an explanatory cross-sectional study was conducted, they implied that, summarizing, students who belonged to the age group 21 or older were substantially more inclined to self-medicate with antibiotics or antimalarials than those aged 20 or younger, and that self-medication with these drugs is relatively common among undergraduate university students in Khartoum State.Our outcomes underscore the significance of emerging strategies to encourage the responsible use of antibiotics and antimicrobials [12].
Conclusion
Antimicrobial resistance and its misuse in varied fields were issues on which participants had better knowledge and attitudes; notwithstanding, there is still much more to be accomplished.
Recommendation
Focusing on the results presented in this research, the authority may enact strict controls to prohibit the distribution and purchase of antimicrobial drugs without a legitimate prescription from a medical professional, in addition to boosting awareness of the proper use of antimicrobials among purchasers, healthcare professionals, and the general public through social media posts, TV, radio, messages, workshops, and extensive educational campaigns.
Acknowledgements: Many thanks and respect to the students of Al-Razi University's Faculty of Medicine for their contributions to the finalization of this research.
Conflict of Interest: Authors declare that there is no conflict of interest.
Financial Support: None declared
References
- World Health Organization. Antimicrobial resistance Fact sheet, 2021.
- Golkar Z, Bagasra O, Pace DG. Bacteriophage therapy: a potential solution for the antibiotic resistance crisis. J Infect Dev Ctries, 2014; 8(2): 129-136. doi: 10.3855/jidc.3573. PMID: 24518621.
- Davies J, Davies D. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev, 2010; 74(3): 417-433. doi: 10.1128/MMBR.00016-10. PMID: 20805405; PMCID: PMC2937522.
- Rossolini GM, Arena F, Pecile P, Pollini S. Update on the antibiotic resistance crisis. Curr Opin Pharmacol, 2014; 18: 56-60. doi: 10.1016/j.coph.2014.09.006. PMID: 25254623.
- Saha M, Sarkar A. Review on Multiple Facets of Drug Resistance: A Rising Challenge in the 21st Century. J Xenobiot, 2021; 11(4): 197-214. doi: 10.3390/jox11040013. PMID: 34940513; PMCID: PMC8708150.
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet, 2022; 399(10325): 629-655. doi: 10.1016/S0140-6736(21)02724-0. Erratum in: Lancet, 2022; 400(10358): 1102. PMID: 35065702; PMCID: PMC8841637.
- Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Ther Adv Drug Saf, 2014; 5(6): 229-241. doi: 10.1177/2042098614554919. PMID: 25436105; PMCID: PMC4232501.
- Nathan C, Cars O. Antibiotic resistance—problems, progress, and prospects. N.
Engl. J. Med, 2014; 371: 1761–1763. - Rather IA, Kim BC, Bajpai VK, Park YH. Self-medication and antibiotic resistance: Crisis, current challenges, and prevention. Saudi J Biol Sci, 2017; 24(4): 808-812. doi: 10.1016/j.sjbs.2017.01.004. PMID: 28490950; PMCID: PMC5415144.
- Iwu CD, Korsten L, Okoh AI. The incidence of antibiotic resistance within and beyond the agricultural ecosystem: A concern for public health. Microbiologyopen, 2020; 9(9): e1035. doi: 10.1002/mbo3.1035. PMID: 32710495; PMCID: PMC7520999.
- Denis K Byarugaba, Donna A Kusemererwa, Aziz A Maij, Charles B Rwabukwali, Connie Cleona Kyarisiima, Eric Wobudeya, et al. The committee coordinated the development of this National Action Plan (NAP) on Antimicrobial Resistance (AMR) with support from the Center for Disease Dynamics, Economics & Policy (CDDEP) under the Global Antibiotic Resistance Partnership (GARP) and the World Health organization Uganda Country office. UNAS undertook this work on behalf of the Ministry of Health (MOH), the Ministry of Agriculture, Animal Industry, and Fisheries (MAAIF), and the Ministry of Water and Environment. 2018-2023, FMOH & MOAR, national action plan on antimicrobial resistance, P.8 & 111.
- Abdelmoneim Awad, Idris B Eltayeb in Sudan. Estimate the prevalence of self-medication with antibiotics and/or antimalarials Self-Medication Practices with Antibiotics and Antimalarials among Sudanese Undergraduate University. Annals of Pharmacotherapy, 2007; 41(7-8). https://doi.org/10.1345/aph.1K068
- Shahpawee NS, Chaw LL, Muharram SH, Goh HP, Hussain Z, Ming LC. University Students’ Antibiotic Use and Knowledge of Antimicrobial Resistance: What Are the Common Myths? Antibiotics,2020; 9: 349. https://doi.org/10.3390/antibiotics9060349
- Alnasser AHA, Al-Tawfiq JA, Ahmed HAA, Alqithami SMH, Alhaddad ZMA, Rabiah ASM, et al. Public knowledge, attitude and practice towards antibiotics use and antimicrobial resistance in Saudi Arabia: A web-based cross-sectional survey. J Public Health Res, 2021; 10(4): 2276. doi: 10.4081/jphr.2021.2276. PMID: 34313091; PMCID: PMC8715265.

