Demographic and histopathological variation of ameloblastoma: A clinico-histological study
Hafiza shahzadi Maryam1,*, Sibghatullah2, Sehrish3, Khushbakht Khanzada Rajput4, Aiman Ajmeer5 and Ezzah Bibi6
1Department of Pathology, Peshawar Medical college, Pakistan
2Department of Pathology, Frontier medical college, Pakistan
3Department of Pathology, Ayub Medical college, Pakistan
4Department of Pathology, Pakistan institute of medical sciences (PIMS), Pakistan
Received Date: 28/04/2023; Published Date: 15/08/2023
*Corresponding author: Hafiza Shahzadi Maryam, Department of pathology, Frontier Medical College, Abbottabad, Pakistan
Abstract
Ameloblastoma is a benign tumor that displays slow growth and aggressive behavior with a high rate of recurrence.
Aims: The aim of the study was to determine the demographic and histopathological variations of ameloblastoma in northern Pakistani population by retrospectively comparing and assess diagnosed cases of ameloblastoma using different parameters.
Materials and Methods: Histopathologically already diagnosed cases of ameloblastoma were retrieved from past records of the Department of Pathology. Totally, 74 cases were isolated from previous 5 years record. The patients were divided according to (a) gender, (b) age group, (c) site of the lesion and (d) histopathological types. These findings were compared with those available in the literature. This is retrospective study, mean and standard deviation was calculated.
Results: Among 74 patients, 37 (50%) were male and 37 (50%) were female. A maximum number of cases (62 of 74) of ameloblastoma were found in the third to fifth decades of life. Mandible was commonly involved (63 cases out of 74), Follicular variety was found in 66% followed by plexiform 16% follow by unicystic 14% then achantomatous 3 % and mixed 1%. The age range was 34.97 + 15.55
Conclusions: This data may serve as baseline information on occurrence of various histopathological types of ameloblastoma in northern Pakistani population and helps comparing it with other similar studies conducted in different geographic population.
Keywords: Ameloblastoma; Demography; Histopathological; Follicular
Introduction
Ameloblastoma is an odontogenic tumour with variable histological patterns and clinical characteristics [1]. Cystic lesions that occur in the jaw bones and been classified in distinct ways according to different bases, e.g., embryologic origin, etiology, clinical and morphological features. A true or epithelial cyst is defined as a cavity which is entirely or partially bordered by an epithelium lining containing fluid or semi-fluid material is referred to as a true or epithelial cyst. The World Health Organization (WHO) has classified the epithelial cysts in jaw into odontogenic and non-odontogenic cysts [2,3]. The relative frequency of mandible to maxilla is reported to be varying from 80 – 20% to 99 –1%. In the mandible majority of ameloblastomas are found in the molar ramus region. The worldwide occurrence of ameloblastoma is 0.5 cases per million people per year [4]. The association of ameloblastoma with odontoma is well established and accepted, but the consensus group did not find it justified to separate them as a unit, they reappear as ameloblastomas [5].
The most widely used classification, based on clinical, radiological and morphological criteria divided ameloblastoma into the following categories [6], Solid ameloblastoma, Unicystic ameloblastoma, Desmoplastic ameloblastoma, Peripheral ameloblastoma, Malignant ameloblastoma.
Although the WHO classification offered useful guidelines for management, there is a lack of accurate terminology that restricts its diagnostic use 5 A more current classification of odontogenic tumors, including ameloblastoma, has recently been proposed [6]. Thus, the word 'multicystic' adds little meaning except misperception to the word solid multicystic ameloblastoma. Therefore, traditional lesions should merely be called conventional ameloblastoma' and the word solid/ multicystic should be eliminated. In addition, the preponderance of plexiform ameloblastoma in the posterior maxilla is not a justification for distinguishing it as different entity since it is still a recognizable site of incidence for traditional ameloblastoma, and can therefore be regarded as a histological category of traditional ameloblastoma. It was also suggested that the distinctive radiographic characteristics of demoplastic ameloblastoma, distinct from other histological types / subtypes, should be a feature of demoplasia [7] As such, desmoplastic ameloblastoma should clearly be noted for its distinct radiographic and clinical appearance.
The most prevalent ameloblastoma is the solid / multicystic / conventional form, which accounts for around 91 percent of all cases of ameloblastoma. It's growing slowly and it's taking a benign path. Histologically, solid / multicystic / conventional ameloblastoma has two separate histological patterns: follicular and plexiform. The follicular type shows proliferating epithelial odontogenic cells organized in islands, while the plexiform type shows epithelial cells arranged in continuous anastomosing row. It is not rare for an ameloblastoma to exhibit all histological trends. In addition to these two histological forms, cystic, granular, acanthomatous, spindle cell, basal cell, clear cell and other microscopic subtypes have been identified.Unicystic ameloblastoma is the second most prevalent ameloblastoma and accounts for approximately 5–15 percent of all cases [8]. It is most often found in younger patients with an average age of 26.1 years, and its primary site is the posterior mandible, often present as an asymptomatic swelling [9].
The bulk of unicystic ameloblastomas resemble dental cysts due to their involvement with an unbroken tooth. The WHO classification [10], and the more recent recommendations 7 recognize two major histopathological forms of luminal and mural unicystic ameloblastoma. The luminal version reveals a cystic pattern lined with an ameloblastomatous epithelium that protrudes into the lumen as plexiform proliferations that appear like an intraluminal subtype. The wall variant reveals either the follicular or the plexiform configuration of the epithelial ameloblastomatous cells within the cystic wall. It is not rare for both variants to be found in the same ameloblastoma lesion.
The study was aimed to find such differences in distribution using different demographic parameters of this tumor in Northern Pakistani population and to compare the findings of this study with those available in similar literature.
Materials and Methods
The present study was conducted in the department of Pathology of Peshawar Medical college and Pakistan institute of medical sciences Islamabad. This study consists of 74 cases of ameloblastoma of both genders. The inclusion criteria were cases within specified age group. Exclusion criteria were cases with poor radiographs or with indefinite diagnosis. The protocol was approved from ethical committee of institutional before the commencement of study. General demographic characteristics such as age, gender, name etc. was recorded in case history performa. Other factors such as anatomical location and histopathological type etc. were also recorded. Type of treatment was also recorded. Patients were followed up regularly. Results obtained were tabulated on Microsoft excel sheet and subjected to statistical analysis. P value < 0.05 was considered as statistically significant.
Results
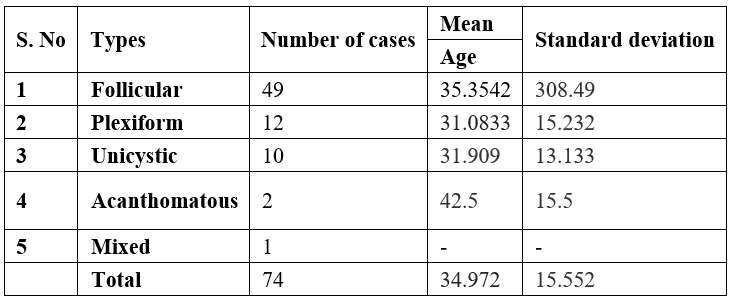
Male patients accounted for 37 (50%) and female patients accounted for 37 (50%), as well as male to female ratio of 1:1. Their age ranged from 5 to 80 years old (table 1), with a mean of 34.9±15.5 years while follicular 35.3±14, plexiform 31.0± 16, unicystic 31.9 ± 8, achanthomatous 42.2 ±15.5 (table 3). Male patients accounted for 15 (40.5%) and female patients accounted for 22 (59.5%).
The mandible was the most common location for tumors, accounting for 85.14 % (63) of all cases,9 cases of maxilla (12.16%), hard plate and alveolar bone 1 case each (1.35%), out of 49 cases follicular ameloblastoma 42 cases of in mandible, 5 in maxilla 1 in hard plate,1 in alveolar bone, maxilla cases, 12 cases of plexiform 9 in mandible, 3 in maxilla, while 10 cases of unicystic 9 in mandible 1 in maxilla, then achanthumatous 2 in mandible and mixed 1 case in mandible (Table 2).
Gender Distribution

Types of tumors
Among 74 cases follicular type 49(66%) patients, plexiform 12(16%), unicystic 10(14%) then acanthomatous in 02 (3%) and mix 1 (1%)
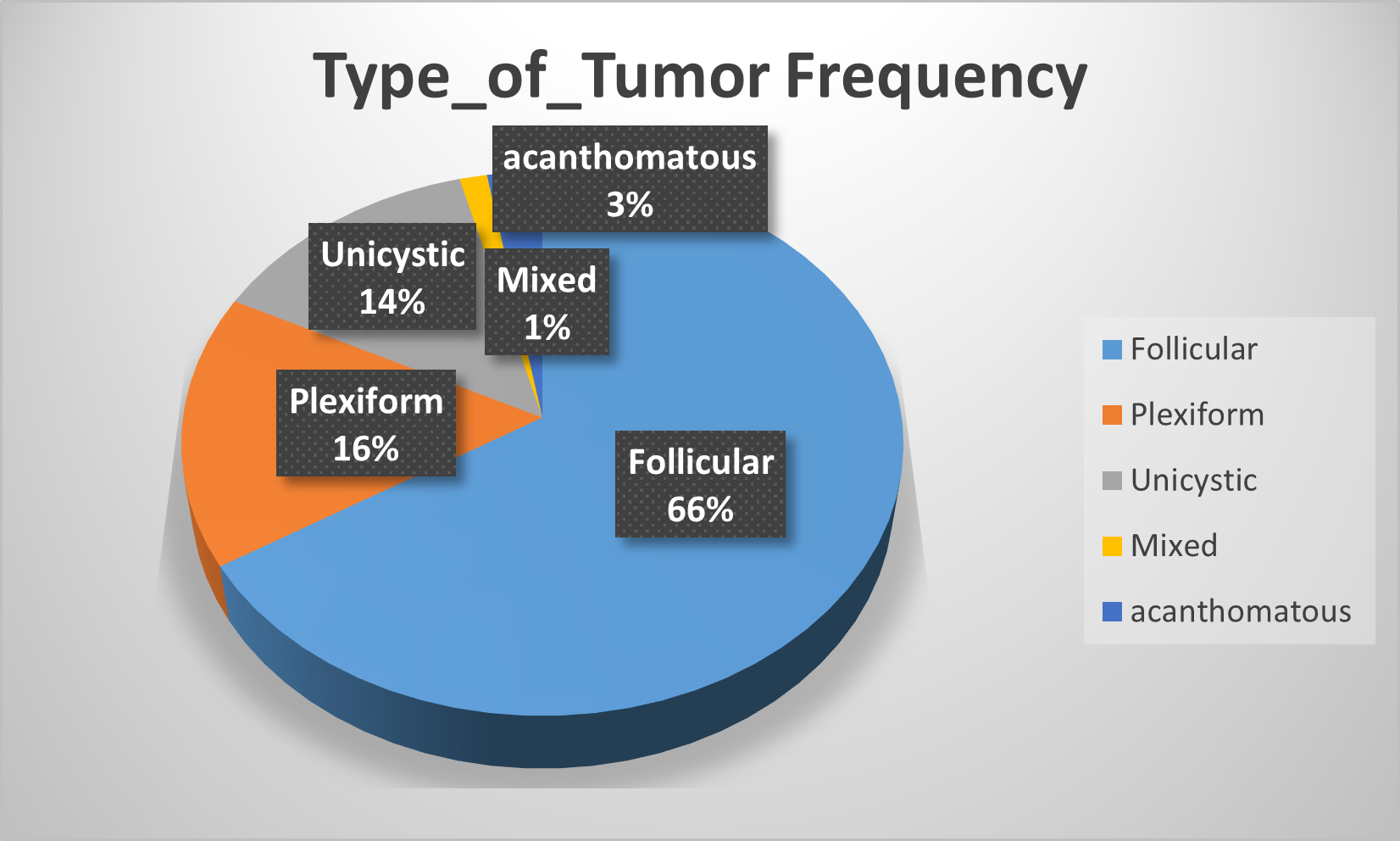
Table 1: Distribution of histological subtypes based upon age of subject.

Table 2: Histological subtypes as per different Anatomical location.

Table 3: Histological types and age of the patient (n=74).
Interpretation & discussion
Ever since the time period “Adamantinoma” was coined by Mallassez, controversy has prevailed as to the most appropriate shape of remedy to save the recurrence of lesion. The time period ameloblastoma become coined by using Ivey and Churchill [4]. Ameloblastomas account for 1% of benign tumors and cysts of the jaw prevalence is expected to be 0. Five instances consistent with million individual years worldwide [11]. Historically, Ameloblastoma has been recognized for over a century and a half. Its early detection is likely due to its frequency, persistent local development, and capacity to generate noticeable deformity prior to major debilitation. Recurrence, particularly following conservative therapy, has greatly raised awareness of this lesion [12].
In the present study, out of 74 cases, males were 37 and females were 37 Which is According to several studies, there was equal gender distribution of 50 (50%) male and 50 (50%) female with a ratio of 1:1. 16, (in Nigeria), Ameloblastoma occurs with equal frequency in men and women [13-15], while slightly different from that in studies in Malaysia, South Korea, and China (male-to-female ratio 1.4:1) [17-19].
In the present study the commonest age group of occurrences of ameloblastoma was second and third decade of life (40%) The age range was 34.97 + 15.55. These results were similar to other reported studies literature the commonest affected age group was 11 – 20 years with a mean age of 33.3 year [25], Considering all the 74 cases in the current study, the commonest affected age group was 21 – 30 years with a mean age of 34.9 years. This finding is in agreement those reported in all these studies on ameloblastoma reviewed Tawfik et al., 2010 Egypt 34 cases Mean age: 34.5 years [29], Selvamani M and Kamrujjaman M et al in their studies analyzed 153 and 62 cases and found that the commonest affected age group was 11-20 and 20- 30 years respectively [23,24]. In different studies on cystic jaw lesions by Kamrujjaman M et al [4], Monteiro L et al [7], Rao K et al [8], Urrutia-Nunez S et al [9], Avelar RL et al [10] and Aleem B et al [11], the mean ages were 28.06, 34.0, 42.0, 42.0, 28.9 and 29.6 years respectively.
In this study, the follicular type of ameloblastoma was the most common histologic variant seen in 49 patients, followed by plexiform 12 followed by unicystic 10 then acanthomatous in 02 each, and mix in 1 patient, which is smilar reports from Nigeria, they observe the follicular type of ameloblastoma was the most common histologic variant, followed by the mixed variant [20]. This is similar to the findings of Simon et al.’s study conducted in Tanzania, which found that the follicular type was the most common histopathological pattern, accounting for 51.6%, followed by the plexiform pattern at 23.6% [21], However, a study done by Saghravanian et al. in Iran reported findings contrary to the present study and to several other related prior studies in which the plexiform pattern was the most common histopathological pattern at 46.4% followed by follicular (26.8%) and acanthomatous (7.1%) [22].
The most frequent anatomical location of ameloblastoma was in the mandibular 85.14 % whereas maxillary area was affected in 12.16 %, Hard palate and 35 %, alveolar bone 1.35 % of the cases, This figure is comparable with 87.3 % reported in a KoreanStudy [26], 87.8 % in a Sri Lankan series,16 93.0 % in a US data [27], A study reported in india ,27 cases (81.66%) of intraosseous ameloblastomas were encountered in the mandible [28].
These data may serve as baseline information on occurrence of various histopathological types of ameloblastoma in northern Pakistani population and helps comparing it with other similar studies conducted in different geographic population.
Conclusion
The study results show commonest age for prevalence of ameloblastoma was second and third decades of life, Age ranged from 5 to 80 years old. Male and female ratio being 1:1 mandible was the most affected site. The most common histological variant in this study was follicular ameloblastoma. The age range was 34.97 + 15.55. The mandible was the most common location for tumors, accounting for 85.14 % (63) of all cases 9 cases of maxilla (12.16%), hard plate and alveolar bone 1 case each (1.35%).
Financial support and sponsorship: Nil.
Conflicts of interest: There are no conflicts of interest.
References
- Masaaki, Kawamura, Nobuo, Inoue, Ichizo, Kobayashi, et al. Dredging Method-A New Approach for the Treatment of Ameloblastoma. Asian journal Oral Maxillofacial Surgery, 1991: 3; 81-88.
- Neville BW, Damm DD, Allen CM, Chi AC. Odontogenic cysts and tumors. In: Oral and Maxillofacial Pathology. 4th ed. St Louis: Elsevier, 2016; pp 632–689.
- Giraddi GB, Bimleshwar SC, Singh C, Garg V, Anusha JS. Ameloblastoma-series of 7 treated cases—and review of literature. Arch Oral Sci Res, 2011; 1: 152-155.
- Brown NA, Betz BL. Ameloblastoma: a review of recent molecular pathogenetic discoveries. Biomarkers in cancer, 2015; 7: BIC-S29329.
- Wright JM, Vered M. Update from the 4th edition of the World Health Organization classification of head and neck tumours: odontogenic and maxillofacial bone tumors. Head and neck pathology, 2017; 11: 68-77.
- Rastogi S, Nijhawan S, Modi M, Kumar A, Aslam N, Lstheef F. Radiolucent-radiopaque lesion in the mandible-a nobel diagnostic approach. J Clin Diagn Res, 2010; 4: 2300-2307.
- Wright JM, Odell EW, Speight PM, Takata T. Odontogenic tumors, WHO 2005: where do we go from here?. Head and neck pathology, 2014; 8: 373-382.
- Dhanuthai K, Chantarangsu S, Rojanawatsirivej S, Phattarataratip E, Darling M, Jackson-Boeters L, et al. Ameloblastoma: a multicentric study. Oral surgery, oral medicine, oral pathology and oral radiology, 2012; 113(6): 782-788.
- Bansal S, Desai RS, Shirsat P, Prasad P, Karjodkar F, Andrade N. The occurrence and pattern of ameloblastoma in children and adolescents: an Indian institutional study of 41 years and review of the literature. International journal of oral and maxillofacial surgery, 2015; 44(6): 725-731.
- Sciubba J, Eversole L, Slootweg PJ. Ameloblastoma. In World Health organization pathology and genetics of head and neck tumoursIARC Press Lyon, 2005; pp. 283-289.
- Thuckanaickenpalayam Ragunathan Y, Keniyan Kumar S, Janardhanam D, Ravi A, Santhanam V, Ramdas MN. Prevalence and Epidemiological Profile of Ameloblastoma in India: A Systematic Review and Meta-Analyses. Asian Pacific Journal of Cancer Prevention, 2022; 23(11): 3601-3610
- Regezi JA, Sciubba JJ.Text book of Oral pathology: clinical-pathologic correlations.5th addition, 2009; 261.
- Robinson HBG. Ameloblastoma; a survey of three hundred and seventy-nine cases from the literature. Archive Pathology, 1937: 23; 831-843.
- Daramola JO, Ajagbe HA, Oluwasanmi JO. Ameloblastoma of the jaws in Nigerian children: a review of 16 cases. Oral Surgery, 1975: 40; 458-463.
- Small LA, Waldron CA. Ameloblastoma of the jaws .Oral Surgery Oral Medicine Oral Patholog, 1995; 8: 281-287.
- Nwoga MC. Fluid Aspirates of Ameloblastoma: Types, Prevalence, and Prognostic Relevance. International Journal of Medicine and Health Development, 2022; 27(4).
- Hong J, Yun PY, Chung IH, et al. Long-term follow up on recurrence of 305 ameloblastoma cases. Int J Oral Maxillofac Surg, 2007; 36: 283-288.
- Jing W, Xuan M, Lin Y, et al. Odontogenic tumours: a retrospective study of 1642 cases in a Chinese population. Int J Oral Maxillofac Surg, 2007; 36: 20-25.
- Siar CH, Lau SH, Ng KH. Ameloblastoma of the jaws: a retrospective analysis of 340 cases in a Malaysian population. J Oral Maxillofac Surg, 2012; 70: 608-615.
- Ladeinde AL, Ogunlewe MO, Bamgbose BO, Adeyemo WL, Ajayi OF, Arotiba FT, et al. Ameloblastoma: analysis of 207 cases in a Nigerian teaching hospital. Quintessence International-English Edition, 2006; 37(1): 69.
- Simon ENM, Merkx MAW, Vuhahula E, Ngassapa D, Stoelinga PJW. A 4-year prospective study on epidemiology and clinicopathological presentation of odontogenic tumors in Tanzania. Oral Surgery Oral Med Oral Pathol Oral Radiol Endodontol, 2005; 99(5): pp. 598-602.
- Saghravanian N, Salehinejad J, Ghazi N, Shirdel M, Razi M. A 40-year retrospective clinicopathological study of ameloblastoma in Iran,Asian Pac J Cancer Prev APJCP, 2016; 17(2): pp. 619-623.
- Selvamani M, Donoghue M, Basandi PS. Analysis of 153 cases of odontogenic cysts in a South Indian sample population: a retrospective study over a decade. Brazilian oral research, 2012; 26: 330-334. https:// doi.org/10.1590/S1806-83242012005000007
- Kamrujjaman M, Hasan S, Khan AD, Noor H, Hasnat A. Clinicopathological Evaluation of Odontogenic Jaw Cysts. Update Dent. Coll. J, 2015; 30-39.
- Ghosh A, GhartiMagar D, Thapa S, Talwar OP. Histopathological subtypes and demographic profile of Cystic jaw lesions-A hospital-based study. Journal of Pathology of Nepal, 2019; 9(1): 1445-1449.
- Kim SG, Jang HS. Ameloblastoma: a clinical, radiographic, and histopathologic analysis of 71 cases. Oral Surg Oral Med Oral Pathol Oral RadiolEndod, 2001; 91: 649-653.
- Buchner A, Merrell PW, Carpenter WM. Relative frequency of central odontogenictumors: a study of 1,088 cases from Northern California and comparison to studies from other parts of the world. J Oral MaxillofacSurg, 2006; 64: 1343-1352.
- Malik AH, Andrabi SW, Shah AA, Najar AL, Hassan S. Ameloblastoma: a clinicopathological retrospective study. IOSR-JDMS, 2018; 17: 30-32.
- Tawfik MA, Zyada MM. Odontogenic tumors in Dakahlia, Egypt: analysis of 82 cases.Oral Surg Oral Med Oral Pathol Oral Radiol Endod, 2010; 109: e67-73.

