Prostatic Biopsies: Experience of the Urology Department of CHU HASSAN II of Fez about 200 Cases
Alaoui mhammedi N*, Mosatafa Ahssaini, Soufiane Mellas, Jalal Eddine El Ammari, Mohamed Fadl Tazi, Jamal Mohammed El Fassi and Hassan MY Farih
Department of Urology, CHU HASSAN II, FES, Morocco
Received Date: 12/04/2023; Published Date: 24/07/2023
*Corresponding author: Alaoui mhammedi Nabil, Department of Urology, CHU HASSAN II, FES, Morocco
Introduction
Prostate cancer is a significant public health issue, with an estimated incidence of 2,332 cases per year in Morocco, ranking as the second most prevalent cancer type after lung cancer. Prostate biopsy is recommended when an abnormality is found during a digital rectal exam or if the PSA level is elevated. Ultrasound technology is used to guide biopsies towards suspicious zones, allowing for precise mapping. This study aims to evaluate the technique, results, and complications of prostate biopsy at the University Hospital of Fez's urology department.
Materials and Methods
This is a retrospective descriptive study of a series of 200 cases of prostate biopsies, collected at the Urology Department at the University Hospital of Fez over a period of 3 years from 2013 to 2016, including inpatients and outpatients.
Inclusion criteria:
- Patients who are candidates for prostate biopsy in the urology department at the university hospital of Fez over a 3-year period from 2013 to 2016.
- Patients with a justified indication for biopsy: a PSA level higher than 4 ng/ml or an abnormal digital rectal examination.
Exclusion criteria:
- Patients with a contraindication to prostate biopsy (uncorrected coagulation abnormality, untreated urinary tract infection...).
- Patients with an incomplete file.
Statistical analysis: To conduct this study, the data found were grouped and numerized in a Microsoft Excel table and processed by SPSS version 25 software.
Results
The mean age of the patients was 69.74 years, with extremes ranging from 47 to 93 years.
Six patients (3%) had a history of benign prostatic hypertrophy (BPH), 4.6% had undergone transurethral resection of the prostate (TURP), 1.5% had undergone a previous biopsy which came back negative.
Urinary signs were the most frequent circumstance of discovery with 88.5% (177 cases), followed by chance discovery with 11% (22 cases) and lastly general signs with only one case (0.5%). The number of patients with obstructive signs (Dysuria, drip micturition) was 46, i.e. 23% and that of patients with irritative signs (Pollakiuria, mictional burns) was 2 patients, i.e. 1%. On the other hand, 71 patients (36%) had obstructive and irritative signs (TUBA). Twelve patients (6%) had presented with URI.
The digital rectal examination (DRE), the non-essential examination estimating the weight and consistency of the prostate, showed an average weight of 49.91 grams, and a soft consistency in 46 cases, hard in 58 cases, nodular in 71 cases, firm in 13 patients.
Para-clinical examinations based on the determination of prostate specific antigen (PSAt), the results of which were as follows a PSAt level between 4 and 10 ng/ml in 86 cases (43%), in 32 cases (16,30%) a level between 10 and 20 ng/ml, and in 68 cases (34,20) levels higher than 20 ng/ml and only 14 patients (6,50%) had a PSAt level lower than 4ng/ml; and the ultrasound (suprapubic/endorectal) analyzing the aspect, the size of the prostate and guiding the biopsies, this one showed us a heterogeneous aspect (40%), homogeneous (28,3%), nodular (30%), with an average prostatic volume of 69,85cc going from 30 to 138 cc
The results of our biopsies were in favor of adenocarcinoma (ADK) of the prostate in 50.5% of cases with a gleason score of 8(4+4) and 6(3+3) representing 13.5% and 12.5% respectively; and benign prostatic hypertrophy (BPH) in 44.9%, with only one case of small cell neuroendocrine adenocarcinoma.
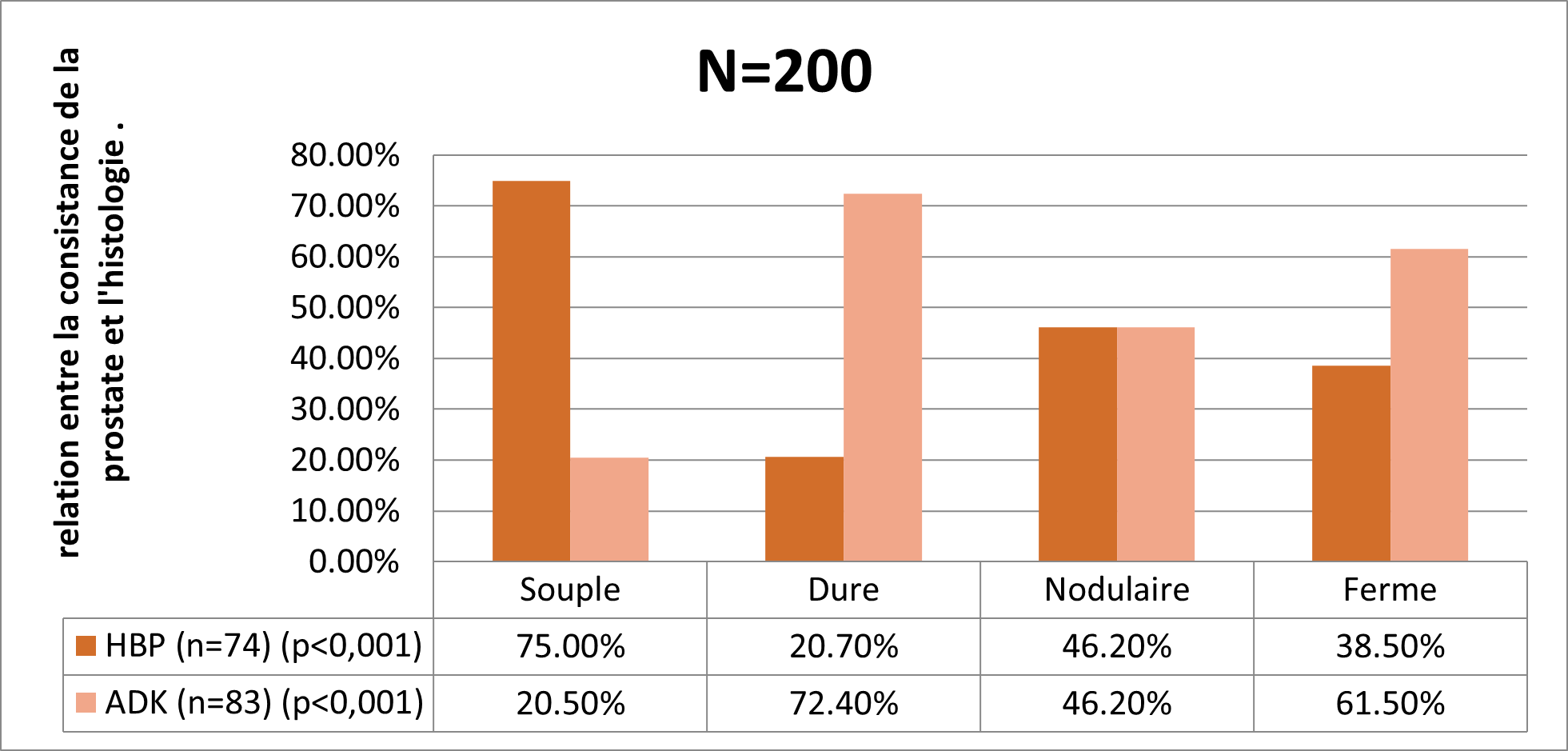
Prostate ADK is significantly related to the consistency of the prostate expressed by digital rectal examination. It goes from 72.4% in case of hard consistency to 61.5% in case of firm consistency. The same observation applies to BPH which is also significantly related to consistency, from 75% in case of soft consistency to 20.7% in case of hard consistency (Graph 1).
The prevalence of ADK increases with the PSA value, from 17% for PSA <4 to 91% for PSA >20. While BPH decreases with PSA value, from 75% for PSA <4 to 8.1% for PSA >20 (Graph 2).
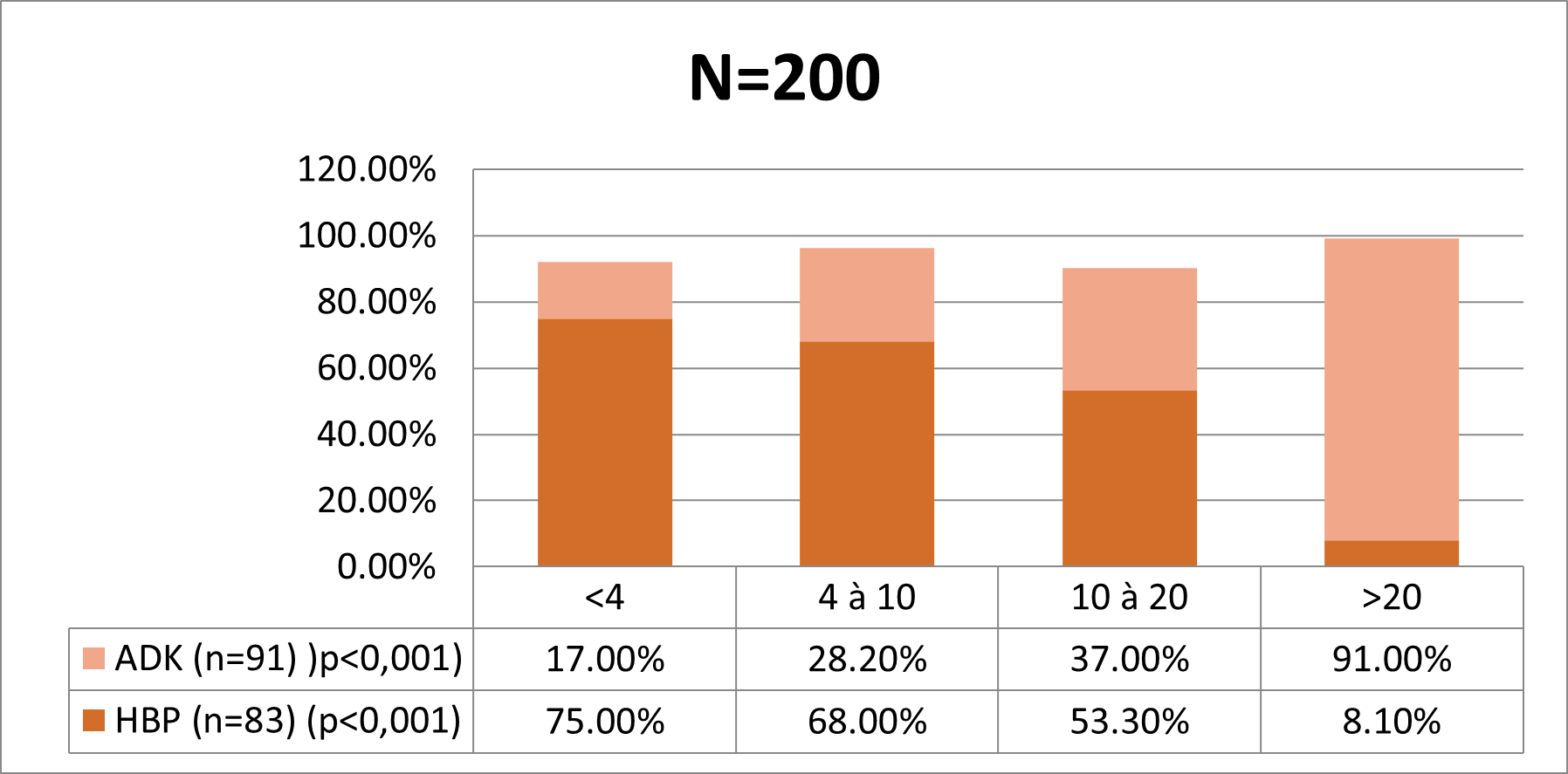
Graph 2: Relationship between PSA level and histology.
Discussion
Early detection of CaP prostate cancer relies on identification of risk factors, digital rectal examination, and PSA testing. The recognized risk factors for CaP are age (constant increase in risk), ethnicity and family history of prostate and breast cancer. Rozet F et al [1,2] report an average age at diagnosis of 70 years, which is consistent with our study.
Far from taking the place of pathological examination, RT is a valuable aid in the diagnosis of BPH or prostate cancer. Most cancers develop in the posterior peripheral zone of the prostate and can therefore be accessed by DRE. A normal DRE does not rule out cancer, 23-45% of cancers do not result in palpable changes. In our series, the prostate was suspicious in 123 cases (72.8%). Cross found 61% of cases and Barthelemy 67% of cases.
Approximately 70% of total serum PSA circulates as bound to blood proteins and 30% as free form. The free form increases in benign prostatic hypertrophy (BPH). The bound form increases in the case of cancer. The free/total PSA ratio decreases in the case of cancer: a low ratio < 15% is correlated with the presence of cancer. PSA levels are correlated with the evolution of the tumor mass [3-5].
The most commonly used PSA cut-off value for cancer diagnosis is 4 ng/mL. When the PSA is between 4 and 10 ng/mL, 70% of diagnosed cancers are localized. A PSA of more than 30 ng/mL is a sign of locally advanced prostate cancer with a high probability of local lymph node metastasis. A PSA level above 100 ng/mL is a marker of locally and distantly advanced prostate cancer with a high probability of bone metastases.
We can say that our results concerning the PSA level in patients with positive prostate biopsies were identical to the literature.
Cancer was detected in 73 of 332 men (22%) with PSA levels between 2.6 and 4.0 ng/ml. Smith et al reported an overall cancer detection rate of 27% in men with PSA levels between 2.6 and 4.0 ng/ml . In contrast to these results, Carter et al. found a minimal difference (2% to 4%) in the probability of detecting curable cancer at PSA levels between 2.5 and 6.0 ng/ml for all age groups .
Biopsy is generally well tolerated, with a low risk of major complications. However, minor complications such as pain and bleeding are common. In the European Rotterdam Study (ERSPC), a randomized prostate cancer screening study, hematuria greater than 3 d was observed in 22.6% of men and correlated with prostate (r = 0.096; p <0.001) and transition zone volumes (r = 0.076; p <0.001) [6,7]. Others have also found an increase in hematuria with greater prostate volume. The reported rate of hematospermia varied considerably among studies (1.1 to 93%). This variation may reflect cultural issues, social stigma, or differing perceptions of importance, as well as differences in data collection between studies. The rate of rectal bleeding varied between 1.3% and 45% across studies. Fewer rectal bleeds were reported in the ERSPC study (1.3%) and there was no correlation with other recorded parameters [7]. Rosario et al. suggested that rectal bleeding was more common than previously reported (36.8%), but only 2.5% found it to be a major or moderate problem [8]. Infection is a well-established risk of transrectal ultrasound-guided biopsy, and in the United Kingdom, out of 72,500 biopsies, 2.15 to 3.6% were readmitted with infectious complications.
Conclusion
Prostate biopsy is a crucial diagnostic procedure for prostate cancer, typically indicated for an abnormal digital rectal exam or a PSA level greater than 4.0 ng/ml. Some authors have suggested lowering the PSA threshold to 2.5 ng/ml, but this is not widely accepted. This study, which evaluated 200 cases of prostate biopsies, found that the recommendations for biopsy indications, approach, antibiotic prophylaxis, and the standard scheme of 12 biopsies were generally followed.
References
- International Agency for Research on Cancer (IARC), Section of Cancer Surveillance. Fact sheets Morocco. GLOBOCAN,
- Rozet F, et al. Recommandations franc ̧aises du Comité de Cancérologie de l’AFU pour le cancer de la prostate - actualisation 2018—2020: cancer de la prostate. Prog Urol, 2018; 28(16): 890-902. DOI: 10.1016/j.purol.2018.08.011
- Boissier R. The prostate specific antigen (PSA). Service d’urologie et transplantation rénale. CHU Conception. Marseille, France.
- Boissier R. L’antigène spécifique de la prostate ou PSA. Service d’urologie et transplantation rénale. CHU Conception. Marseille, France,
- Institut de biologie clinique. Université libre de Bruxelles: PSA – (ANTIGENE PROSTATIQUE SPECIFIQUE) – PSA total et Rapport PSA libre/PSA total.
- Rozet F, et al. Recommandations franc ̧aises du Comité de Cancérologie de l’AFU pour le cancer de la prostate - actualisation 2018-2020 : cancer de la prostate. Prog Urol, 2018; 28(16): 890-902. DOI: 10.1016/j.purol.2018.08.011
- van den Heuvel S, Loeb S, Zhu X, Verhagen PC, Schröder FH, Bangma CH, Roobol MJ. Complications of initial prostate biopsy in a European randomized screening trial. Am J Clin Exp Urol, 2013; 1(1): 66-71.
- Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R, et al. Systematic review of complications of prostate biopsy.

