Flexible Sigmoidoscopy vs Whole Colon Imaging in Patients Presenting with Left Sided Colorectal Symptoms
Drew S Magowan1,* and Jeremy Williamson2
1Specialty Trainee in General Surgery (IST) – Year 2 Royal Gwent Hospital, Newport
2Consultant Colorectal Surgeon Royal Gwent Hospital, UK
Received Date: 05/04/2023; Published Date: 14/07/2023
*Corresponding author: Drew S Magowan, MBChB(hons), MRCS, Specialty Trainee in General Surgery (IST) – Year 2 Royal Gwent Hospital, UK
Abstract
Background: ACPGBI guidelines recommend flexible sigmoidoscopy (FS) only in patients presenting with a rectal mass or blood per rectum without change in bowel habit. Several studies have suggested FS for all left-sided symptoms, including change in bowel habit, in the absence of anaemia or palpable abdominal mass.
Objective: We aimed to examine the risk of missed pathology by such frequent use of FS over whole colon imaging (WCI).
Design: Retrospective review of WCI using CT colonograms and correlation with clinical notes.
Settings: Review of digital imaging, reports and clinical notes.
Patients (Materials) and Methods: Retrospective review was undertaken of 100 consecutive CT-colonograms between 01/10/2018 and 01/01/2019. Findings, age, signs and symptoms were recorded.
Main Outcome Measures: Primary outcome was incidence of significant non-left-sided pathology, both colonic and extra-colonic. Secondary outcome was incidence of left-sided symptoms. These groups were compared to reveal those with pathology which would have been missed by FS alone.
Sample Size: 100 patients.
Results: Median age was 75. 61% had left-sided symptoms without anaemia or mass, 39% had anaemia, no patients had a palpable abdominal mass. 44% had significant left-sided pathology. 20% had significant non-left-sided pathology, of which 20% would have qualified for FS as per the ACPGBI guidelines and 55% would have qualified for FS if done for all patients symptomatic without anaemia or mass. There would have been no cancers missed in the ACPGBI group and one cancer missed in the second group.
Conclusions: ACPGBI guidelines resulted in less missed pathology when compared against those suggesting FS for symptomatic patients without anaemia or abdominal mass.
Keywords: Colorectal; Cancer, Endoscopy; Guidelines; Investigations; Surgery
Introduction
There has been some recent debate regarding the selection of Whole Colon Imaging (WCI) versus flexible sigmoidoscopy (FS) in patients being investigated for “left sided” colorectal symptoms. Current guidelines from the Association of Coloproctology of Great Britain and Ireland (ACPGBI) continue to recommend FS as a first line investigation only in those patients presenting with a palpable rectal mass or Blood per Rectum (BPR) without change in bowel habit (CIBH) [1]. WCI is recommended in patients presenting with CIBH, with or without BPR, as well as those presenting with an abdominal mass or anaemia (men <110g/L, women <100g/L).
However, several studies have suggested FS alone may be sufficiently sensitive regarding the diagnosis of colorectal cancer when patients present with a range of “left sided” symptoms such as BPR, CIBH, tenesmus, left iliac fossa mass or rectal mass [2-4]. It was suggested in a recent large prospective cohort study that FS should suffice in patients presenting with BPR or CIBH, without anaemia or an abdominal mass [2]. Establishing the best investigation for these patients is important, with 900,000 Optical Colonoscopies (OC) and 500,000 FSs carried out annually in the UK; and approximately 47,000 and 21,000 patients awaiting OC and FS respectively at any given time [5,6]. With the use of CT colonography (CTC) ever-increasing, the number of patients undergoing WCI may be substantially higher than the OC numbers alone.
Regarding WCI, multiple studies have shown comparable sensitivity of CTC versus OC in the diagnosis of colorectal cancer [7,8]. Our aim was to examine the incidence of significant pathology during WCI which may be missed by FS alone in patients who present with “left sided” symptoms.
Methods
Retrospective review was undertaken of 100 consecutive CTCs carried out between 01/10/2018 and 01/01/2019 at the Royal Gwent Hospital, Newport, United Kingdom. A record was made of the CTC findings, along with patient age and symptoms including CIBH, BPR, abdominal mass on examination, abdominal pain, and anaemia. CIBH was separated into loose stool or constipation predominant. Anaemia was defined as <13g/dL for men and <12g/dL for women. Primary outcome measure was the incidence of significant non-“left sided” pathology, both colonic and extra-colonic. Secondary outcome measure was the incidence of “left sided” symptoms. These two groups were compared to reveal those patients with pathology which would have been missed by flexible sigmoidoscopy alone. “Left sided” pathology was defined as any finding within the colon at, or distal to, the splenic flexure. “Left sided” symptoms were defined as any combination of CIBH, BPR or lower abdominal pain, without anaemia or abdominal mass on examination.
Results
100 CTCs were reviewed, as outlined in Figure 1. Median age was 75 years. 44 patients (44%) had “left sided” pathology, 20 patients (20%) had non-“left sided” pathology, 36 patients (36%) had no significant abnormality detected. 61 patients (61%) had “left sided” symptoms without anaemia or mass on examination, 39 patients (39%) had anaemia, no patients had a palpable abdominal mass on examination.
Of those 20 patients found to have non-”left sided” pathology, 16 (80%) would have qualified for WCI as per the ACPGBI guidelines and 4 (20%) would have qualified for FS. If guidelines recommending FS for “left sided” symptoms in the absence of broad-definition anaemia or abdominal mass were applied, 9 (45%) would have qualified for WCI and 11 (55%) would have qualified for FS.
Of the 4 patients with non-“left sided” pathology qualifying for FS under ACPGBI guidelines, significant findings comprised 2 small right-sided adenomatous polyps (<2cm); a 3.7cm AAA; and splenomegaly with multiple non-specific splenic lesions. Of the 11 patients qualifying for FS if guidelines for “left sided” symptoms in the absence of broad-definition anaemia or abdominal mass were applied, significant findings comprised 4 small right- sided adenomatous polyps; 3 cases of right-sided diverticulosis; 2 AAAs of 3.7 and 3.8cms; 1 large simple ovarian cyst; 1 case of multiple liver and splenic lesions of likely benign appearance, possibly sarcoidosis; and a T3N1M0 ileal neuroendocrine tumour which was subsequently resected.
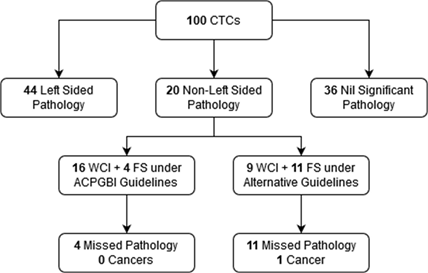
Figure 1
Discussion
Debate continues regarding the appropriate selection of patients for Flexible Sigmoidoscopy (FS) versus Whole Colon Imaging (WCI), either by Optical Colonoscopy (OC) or CT Colonography (CTC). FS is a quicker, less invasive alternative to Optical Colonoscopy (OC) for direct visualization of the colon during investigation of colorectal symptoms, however it will miss pathology proximal to the splenic flexure. OC offers possible visualization of the entire colon, however is a more technically difficult and time-consuming investigation [9]. CTC has been shown to be equally sensitive in the diagnosis of colorectal cancer when compared with OC and is increasingly popular for WCI, however also requires unpleasant bowel preparation and confers a high rate of incidental findings [5,6]. There is some debate concerning the selection criteria for each of these investigations and several recent studies have suggested that FS may be appropriate for patients presenting with “left sided” symptoms in the absence of anaemia or an abdominal mass on examination [2-4].
For example, Thompson et al undertook a prospective study of 16,433 patients over 16 years referred to colorectal clinic. They found that 5.8% had colorectal cancer: 86.2% within the recto-sigmoid colon (“distal”) and 13.8% elsewhere (“proximal”). 96.3% of all referrals had no anaemia or mass – “symptoms only”. 95% of cancers in these “symptoms only” patients were distal; 5% were proximal. FS for “symptoms only” patients missed only1.3% of cancers, suggesting this may be a reasonable option for investigating similar patients [4]. Subsequently, Atkin et al and Cross et al produced a multicentre retrospective study and cohort study respectively by utilising data from 2 randomised controlled trials. They included 7380 patients over the age of 55 referred with possible colorectal cancer to 21 NHS hospitals between 2004- 2007. 73% had change in bowel habit, 38% PR bleeding, 29% abdominal pain and 23% anaemia. 7.5% of patients had colorectal cancer: 77% distal to the splenic flexure, 22% proximal, 1% multifocal. Proximal cancers were diagnosed in 4.8% of patients with anaemia, with or without an abdominal mass. It was noted that a broad anaemia definition of <13 g/dL for men and <12 g/dL for women identified 80% of proximal cancers. Where there was no anaemia or mass: change in bowel habit to looser or more frequent stool, or PR bleeding with or without change in bowel habit yielded only 0.5% incidence of proximal cancer. These low risk “symptoms only” cases made up 41% of the recruited patients. Again, it was suggested that FS alone may safe in these patients [2,3].
However, Herrod et al undertook a systematic review of 7 studies looking at cancer location with “left sided” symptoms. They found that isolated change in bowel habit, with or without rectal bleeding, was a presenting symptom in 73% of left-sided cancers (95% CI 41–96%, I2 = 99%) but also in 13% of right- sided cancers (95% CI 2–30%, I2 = 96%). In all patients with cancer who presented with isolated change in bowel habit, with or without rectal bleeding, the cancer was right sided in 8% of cases (95% CI 4–12%, I2 = 69%). This suggests that there may be a significantly higher number of patients with proximal colon pathology which would be missed by FS alone [10].
There are other factors to be taken into consideration regarding WCI versus FS for the investigation of colorectal symptoms. For example, although FS for left-sided symptoms is considered a quicker and less technically challenging procedure when compared with OC, it has been suggested that only 65% successfully visualise the colon to the hepatic flexure, over 7% are abandoned due to poor bowel preparation and as many as 31.0-34.8% may require subsequent WCI [4,11]. It should be borne in mind that all patients diagnosed with colorectal cancer will require completion WCI [1]. Furthermore, although FS alone for left-sided symptoms may miss only a small proportion of cancers, it will miss all extra-colonic pathology as well as any benign proximal colonic pathology such as diverticulosis or adenomas.
OC and CTC remain the two core options for WCI, with OC generally considered to be the gold standard, and barium enema having been superseded by CTC [3]. However, CTC has been shown to have equivocal sensitivity when compared with OC - quoted at approximately 96% vs 94% respectively in a large systematic review and meta-analysis by Pickhardt et al involving 11,151 patients [8]. They further noted user heterogeneity to be much lower for CTC when compared with OC, which requires significant skill in endoscopy to complete efficiently and safely [9]. Although CTC is sensitive, it has some drawbacks. For example, the SIGGAR trial found that 30% of patients undergoing CTC for possible colorectal cancer required additional colonic investigations, versus only 8% in the OC group [7]. There is also a high rate of incidental extracolonic pathology detected, reportedly 58.7%.
Approximately 14.2% of these findings require investigation and only 2-3% are thought to be significant, such as malignancies and aneurysms [12,13]. The incidence with which these extracolonic incidentals may explain the patients’ symptoms is reported to be around 2.8%, however one study also suggested no difference in the incidence of extracolonic pathology between symptomatic (diagnostic) and asymptomatic (screening) groups [12,14]. Finally, it should also be remembered that CTC and OC are both able to diagnose benign but potentially significant proximal colonic pathology such as diverticulosis and adenomas in patients with “left sided” symptoms, though the incidence of right sided cancers may be low. Papers concerning the use of FS have recognised these limitations and often recommended further cost-benefit analysis regarding the use of WCI versus FS [2-4].
It is interesting to note that part of the argument given for FS over WCI in these patients, in light of the time and cost benefits, is that only 0.5-1.3% of colorectal cancers would be missed [2,3]. However, as outlined above, up to 8% of cancers in patients presenting with symptoms alone may be right sided [10]. Furthermore, completion WCI is still recommended for all colorectal cancers in light of a synchronous cancer incidence of approximately 2.3-3.5% [1,15,16]. This objective risk of missed cancer is deemed unacceptable, whereas a risk of at least 0.5-1.3% would be deemed acceptable were more liberal FS guidelines to be adopted.
Our results examined the possibility of missed non-”left sided” pathology (both right-sided colonic and other intra-abdominal causes) if guidelines were adopted recommending more liberal use of FS. Specifically, it is interesting to compare the current ACPGBI guidelines for the investigation of possible colorectal cancer with the widely cited recommendations by Cross et al. and similar papers, which suggest FS for investigating presentations of “left sided” symptoms in the absence of anaemia or an abdominal mass [1,2]. Our results revealed that 20% of those with non-”left sided” pathology would have qualified for FS alone, with 4 potentially significant findings missed, by application of the ACPGBI guidelines. However, 55% would have qualified for FS alone, with 12 potentially significant findings missed, by application of the Cross et al recommendations, including 4 right-sided polyps and an ileal neuroendocrine cancer (T3N1M0). It is important to note that by use of CTC, both groups also comprised potentially significant non-neoplastic findings such as right-sided diverticulosis, AAAs, an ovarian cyst, and lesions within the liver and spleen.
Conclusion
We found that there was a potential incidence of missed significant non-”left sided” pathology in 4% versus 12% of patients respectively when comparing the ACPGBI guidelines with those recommending FS alone for “left sided” symptoms without anaemia or abdominal mass on examination. A significant number of these potentially missed findings were extra-colonic and it should be noted that although CTC may lead to a high rate of incidental findings, a proportion of these turn out to be clinically significant.
Use of WCI versus FS for the investigation of patients presenting with “left- sided” symptoms remain an ongoing topic for discussion and ACPGBI guidelines remain unchanged. The benefits and limitations of both WCI and FS should be taken into consideration, as well as between OC and CTC. Factors such as efficiency, cost-effectiveness, invasiveness and diagnostic specificity must be weighed against the risk of missed cancers, incidental findings and the need for further investigations in order to establish the “best test first”. Further detailed cost-benefit studies are required in order to bring clarity both in FS versus WCI in patients with “left sided” symptoms, and regarding OC versus CTC for patients where WCI is appropriate.
Limitations: The main limitation of this study is sample size. However, our numbers were adequate to demonstrate our argument and the issues which need to be considered for a fuller understanding of this issue. Further studies are required both regarding FS versus WCI for left-sided symptoms, and regarding colonoscopy versus CTC for patients where WCI is appropriate.
Conflict of Interest: We have no conflicts of interest to report.
Declaration: The authors do hereby confirm that we hold no conflicts of interest with respect to this article. Both authors have read and approved this work as honest and original.
Author Contribution:
Drew S Magowan: Design, literature search, data acquisition + analysis,
Jeremy W: Concept, Design, Manuscript Review
References
- Cunningham C, Leong K, Clark S, Plumb A, Taylor S, Geh I, et al. Association of Coloproctology of Great Britain & Ireland (ACPGBI): Guidelines for the Management of Cancer of the Colon, Rectum and Anus (2017) – Diagnosis, Investigations and Colorectal Dis, 2017; 19: 9-17.
- Cross AJ, Wooldrage K, Robbins EC, et al. Whole-colon investigation flexible sigmoidoscopy for suspected colorectal cancer based on presenting symptoms and signs: a multicentre cohort study. Br J Cancer, 2019; 120: 154–164.
- Atkin W, Wooldrage K, Shah U, Skinner K, Brown JP, Hamilton W, et Is whole-colon investigation by colonoscopy, computerised tomography colonography or barium enema necessary for all patients with colorectal cancer symptoms, and for which patients would flexible sigmoidoscopy suffice? A retrospective cohort studies. Health Technol Assess, 2017; 21(66).
- Thompson MR, Flashman KG, Wooldrage K, Rogers PA, Senapati A, O'Leary DP, et al. Flexible sigmoidoscopy and whole colonic imaging in the diagnosis of cancer in patients with colorectal Br J Surg, 2008; 95: 1140-1146.
- Shenbagaraj L, Thomas-Gibson S, Stebbing J, et Endoscopy in 2017: a national survey of practice in the UK. Frontline Gastroenterology, 2019; 10: 7-15.
- Performance Analysis Team (Central). NHS England and NHS Improvement. NHS Diagnostic Waiting Times and Activity Data – October 2019 Monthly Report, 2019.
- Atkin W, Dadswell E, Wooldrage K, Kralj‐Hans I, von Wagner C, Edwards R, et al. Computed tomographic colonography versus colonoscopy for investigation of patients with symptoms suggestive of colorectal cancer (SIGGAR): a multicentre randomised trial. Lancet, 2013; 381: 1194–1202.
- Pickhardt PJ, Hassan C, Halligan S, Marmo R. Colorectal cancer: CT colonography and colonoscopy for detection–systematic review and meta‐analysis. Radiology 2011; 259: 393–405.
- Thompson C, Ismail T, Radley S, Walt R, Ward ST. Conversion of colonoscopy to flexible sigmoidoscopy: an unintended consequence of quality measurement in endoscopy. Frontline Gastroenterol, 2016; 7(3): 202–206.
- Herrod PJJ, Boyd-Carson H, Doleman B, Blackwell JEM, Hardy EJO, Harper F, et al. Safe investigation of isolated change in bowel habit with a flexible sigmoidoscopy? A systematic review and meta- The Annals of The Royal College of Surgeons of England, 2019; 101(6): 379-386.
- Papagrigoriadis S, Arunkumar I, Koreli A, et Evaluation of flexible sigmoidoscopy as an investigation for “left sided” colorectal symptoms. Postgraduate Medical Journal, 2004; 80:104-106.
- Halligan S, Dadswell E, et al. Identification of Extracolonic Pathologies by Computed Tomographic Colonography in Colorectal Cancer Symptomatic Gastroenterology, 2018; 149(1): 89-101.
- Pooler BD, Kim DH, Pickhardt PJ. Potentially Important Extracolonic Findings at Screening CT Colonography: Incidence and Outcomes Data from a Clinical Screening Program. AJR Am J Roentgenol, 2016; 206(2): 313–318.
- Taya M, McHargue C, Ricci ZJ, et al. Comparison of extracolonic findings and clinical outcomes in a screening and diagnostic CT colonography Abdom Radiol, 2019; 44: 429.
- Lee BC, Yu CS, Kim J, et Clinicopathological features and surgical options for synchronous colorectal cancer. Medicine (Baltimore), 2017; 96(9): e6224.
- Lam AK, Chan SS, Leung M. Synchronous colorectal cancer: clinical, pathological and molecular World J Gastroenterol, 2014; 20(22): 6815–6820.

