Prevalence of Glaucoma in Diabetes Mellitus Patients Attending Tertiary Care Hospital in Pakistan
Unsa Miraj1, Syeda Aliza Kazmi1, Sibgha Ali1, Tooba Fida2,*, Muhammad Saad ur Rehman1 and Nasir Ahmed3
1Department of Medicine, Mayo Hospital, Pakistan
2Department of Internal Medicine, Mayo Hospital, lahore, Pakistan
3Eye Unit II, Mayo Hospital, Pakistan
Received Date: 05/04/2023; Published Date: 13/07/2023
*Corresponding author: Tooba Fida, Internal medicine, Mayo Hospital, lahore, Pakistan
Abstract
Background: This study showed the prevalence of glaucoma in diabetic patients. this cross-sectional survey estimated the presence of glaucoma and its determinants in patients of type 2 diabetes mellitus who visited tertiary care hospital in Lahore, Pakistan.
Methods: A hospital-based cross-sectional study was carried out in the department of ophthalmology at tertiary hospital Lahore, Pakistan. a total of 62 diabetic patients attending the eye OPD at tertiary hospital, Lahore was included in the study according to the inclusion criterion after taking prior consent from each patient. then, an ophthalmologist examined both eyes of all the patients comprehensively for the presence of glaucoma including measurement of IOP by applanation tonometry. the optic disc examination by stereoscopic slit lamp was also done for each patient. Glaucoma was defined as IOP >21mmhg and cup-disc ratio >0.03 with a pale neuroretinas rim.
Results: A total of 62 diabetic patients participated in the study, out of which 30 were males and 32 were females. The mean age of the participants was 56.04 ± 12.09. The mean age of diabetic females having glaucoma was 58.25 ± 9.94 and the mean age of males was 58.36 ±11.12. The ethnicity of all the patients was Punjabi and their diet contained both vegetables and meat. 10 out of 62 patients (16%) had moderate socioeconomic status while 52 out of 62 (84%) had poor socioeconomic status. on observation of the hereditary characteristics, 4 patients (6.45%) reported a positive family history of glaucoma. Only 1 patient had previous knowledge of the relationship between glaucoma and the eye.
Conclusions: Out of 62 diabetic patients who visited the ophthalmology department, 32.25% of them had glaucoma. Regular glaucoma screening for diabetic retinopathy results in manageable cases of glaucoma.
Keywords: Glaucoma; Diabetic Retinopathy; Diabetes Mellitus; Tertiary Care Hospital
Introduction
Diabetes mellitus refers to a group of disorders characterized by increased blood glucose levels. An increase in blood levels of glucose occurs either due to diminished insulin production caused by the destruction of beta cells or due to resistance of the body cells to normal insulin levels or both. The chronically increased blood glucose levels and metabolic abnormalities of diabetes are often associated with secondary damage to multiple organ systems, especially the kidneys, eyes, nerves and blood vessels.
The world health organization (who) has declared that the incidence of diabetes is increasing rapidly worldwide, which has become a major public health concern. The global prevalence of diabetes was estimated to be 2.8% in 2000 and is predicted to be 4.4% in 2030 [1].
Glaucoma is defined as optic nerve damage which is progressive and is caused by a group of ocular conditions led by raised intra-ocular pressure, characteristic visual field defects and distinctive changes in the cup of the optic nerve. Most people with glaucoma have elevated intra-ocular pressure, although some having characteristic optic nerve and visual field changes have normal intraocular pressure. studies indicate that 40% of people with glaucoma have normal IOP [2].
Glaucoma development in people depends upon a large number of risk factors such as age (the elderly is at increased risk), race, first-degree relatives of patients, myopes, and diabetics. people who stress a lot and are nervous, present with an unstable vasomotor system are more prone to glaucoma development.
Primary open angle glaucoma is the most common of all types of glaucoma. It is a painless condition with an insidious onset and raised intra-ocular pressure while the angle of the anterior chamber of the eye is wide open. The elevation of intraocular pressure results from more resistance to the outflow of aqueous humour in trabecular meshworks. Although the cause of resistance in trabecular meshwork is not known clearly, it is thought to be associated with a genetic basis. several studies indicate that vascular diseases such as diabetes mellitus damage the microvascular of the retina and cause the death of retinal cells which causes increased pressure in the eye that ultimately leads to glaucoma [3]. Recently, poag has been seen most commonly in diabetics in many studies taking diabetes mellitus as one of the major risk factors for glaucoma [4]. NVG (Neovascular Glaucoma) is also a complication of glaucoma where leaky new vessels grow in the iris and block the eye’s natural drainage system that leads to glaucoma.
Based on “vision-2020 initiatives”, glaucoma and diabetic retinopathy are becoming leading causes of eye defects worldwide. If comprehensive health care screening techniques are developed in secondary and tertiary care hospitals, severe blindness caused by glaucoma can be detected early and prevented, as nowadays, diabetics are being screened for diabetic retinopathy and its various types [5]. Obviously, vast scale studies on the association between POAG and diabetes mellitus are to be done to increase awareness in the community, which will eventually lead to the development of screening techniques. In Pakistan, few studies are done in some large cities while wide scale research studies need to be done. According to research studies done worldwide, the association between POAG and DM varies widely as some studies indicate no correlation between glaucoma and diabetes [6].
Glaucoma causes irreversible blindness globally. It has become a public health issue and there is a need to introduce new health polices at the national level and to ensure that its screening is done in all areas in a country, including urban and rural [7]. It is measured by several techniques, such as gonioscopy, fundoscopy, perimetry and, including those that evaluate IOP in patients, such as tonometry. Some studies indicate slightly raised IOP among diabetics as compared to non-diabetics, but this IOP variation is relatively small and not well established clinically [8]. Diabetes mellitus causes microvascular abnormalities that lead to diabetic retinopathy, which is well known and proved. Now several studies taking place globally provide evidence that glaucoma and diabetes mellitus have similar risk factors and pathology and elevated fasting glucose ultimately leads to glaucoma [9].
To reduce the burden of disease on the health care system caused by diabetes and its complications, early screening techniques for visual disturbances and end organ damage in diabetic patients should be introduced in tertiary care hospitals, as decreased vision impairs the quality of life at all ages, especially the working age [10].
Materials and Methods
Study Sample
A hospital-based cross-sectional study was conducted to determine the prevalence of glaucoma among the diabetic patients attending the tertiary care Hospital, Lahore's Department of Ophthalmology’s OPD. Prior to conducting this research project and collection of data, the Institutional Review Board (IRB) gave its approval for the conduction of the study. The sample size for assessing the prevalence of glaucoma among diabetic patients who visited the Mayo Hospital’s OPD was computed using a confidence level of 95%, absolute precision of 10%, and an estimated percentage of prevalence of glaucoma of 20% [1]. By using the following formula
n= Z21-α/2P (1-P)
where Z1-α/2= d2
Confidence level 95 percent=1.96
P=Prevalence 20 percent
q=1-p
d=Absolute precision 10 percent
The final sample size for assessing the prevalence of glaucoma among the diabetic patients attending the eye department’s OPD was 62 patients who met the inclusion criteria. Simple random sampling was done using the convenient method. From December 2022 to February 2023, a three-month study was conducted. Patients were selected according to the inclusion criterion of this research study. After receiving Institutional Review Board (IRB) permission, patients were selected based on the study's inclusion criterion.
Inclusion criterion:
Diabetic patients who were at least 18 years old. All diabetic patients who visited the Eye OPD between December 2022 and February 2023 and agreed to participate in the study. Patients with diabetes were confirmed by following the standard diagnostic criterion recommended by the American Diabetic Association (ADA) [11].
Exclusion Criterion:
Patients who did not meet the ADA criterion for diabetes. Patients who had any active eye disease, such as conjunctivitis or iridiocyclitis, as well as those on diabetogenic drugs or those with a history of trauma related to glaucomatous damage were all excluded.
Development of glaucoma assessment questionnaire and procedure
For these individuals, a detailed semi-structured questionnaire was created, which included questions based on previously conducted research of a similar nature found after significant literature review. The questions were simple and asked about their personal information such as age, sex, race, diet, family history, diabetic disease history, understanding of the association between diabetes and glaucoma [1]. A separate section was also introduced for recording the results of their glaucoma clinical examination. After presenting the aims of our research project and the technique of clinical examination for the assessment of glaucoma to each patient, written informed consent was taken from each patient who met the inclusion criteria and was willing to participate in the research study.
Then, using the ADA’s recommended criterion, fasting and postprandial blood sugar levels as well as the clinical history were recorded for the confirmation of diabetes mellitus. The participation of diabetic patients in this study was entirely voluntary and confidentiality was guaranteed. All of the selected patients filled out the questionnaire for personal data, demographic data, diabetes disease history and knowledge after written informed consent [2]. Then, an expert ophthalmologist from the Mayo Hospital Lahore's department of ophthalmology evaluated both eyes of all those diabetic patients comprehensively for the existence of glaucoma, including measuring their IOP (intra ocular pressure) using applanation tonometry. Each patient had an optic disc examination using a stereoscopic slit lamp as well as evaluation of the anterior chamber drainage angle by gonioscopy. IOP (intraocular pressure) greater than 21mmHg and CDR (cup-disc-ratio) more than 0.7 or a difference of 0.2 between the two eyes with a pale neuroretinal rim was considered glaucoma.
Statistical analysis
Statistical Packages for Social Sciences was used to conduct the statistical analysis [12].
The completeness of the response part as well as the clinical data section of the questionnaires were evaluated. Only questionnaires that were completely filled out, including the clinical examination section, were considered for analysis. Percentages, tables and mean standard deviations have been used to present data.
Results
A total of 62 diabetic patients participated in the study. Out of that, 30 were males and 32 were females. The mean age of the participants is 56.04 ± 12.09. The mean age of diabetic females having glaucoma is 58.25 ± 9.94 and of males is 58.36 ±11.12. The ethnicity of all the patients was Punjabi and their diet contained both vegetables and meat. 10 out of 62 patients (16%) have moderate socioeconomic status while 52 out of 62 (84%) have poor socioeconomic status.
On observation of the hereditary characteristics, 4 patients (6.45%) reported a positive family history of glaucoma.
Only 1 patient had previous knowledge of the relationship between glaucoma and eye problems.
The number of years for which diabetes mellitus was present in the glaucoma patients was 7.1± 7.45 years. The mean IOP in diabetic patients who have glaucoma was 22.25 ± 12.14 mm Hg and the mean CD ratio was 0.53 ± 0.24.
46.77% of the study population were males and 53.23% were females (Table 1).
Out of 62 diabetic patients who visited the Ophthalmology department 32.25% of them had glaucoma (Table 2,3). Out of 32.25 percent of diabetic patients with glaucoma, 55 percent were male and 45 percent were female.
85% of the patients having glaucoma were poor (Table 4).
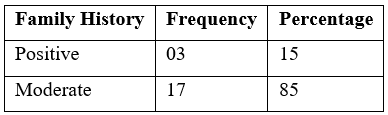
Only 3 diabetic patients having glaucoma reported a positive family history (Table 5).
Table 1: Distribution of males and females in the study population (n = 62).

Table 2: Distribution of glaucoma patients in the study population (n = 62).
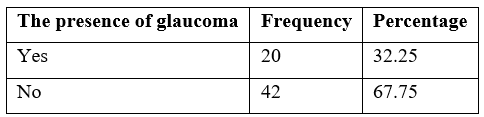
Table 3: Distribution of glaucoma in diabetic patients based on sex (n = 20).
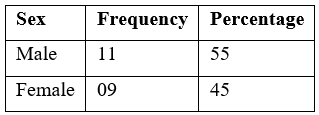
Table 4: Distribution of glaucoma in diabetic patients based on socioeconomic status (n = 20).
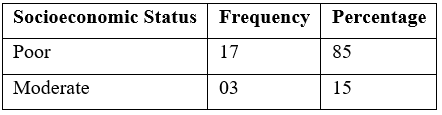
Table 5: Distribution of glaucoma in diabetic patients based on family history (n = 20).
Discussion
Diabetes mellitus has become a leading cause of many of the ocular diseases including glaucoma. Diabetes mellitus has a damaging effect on the microvasculature of the eye. Long standing hyperglycemia and lipid dysregulation also increase the risk of neuronal stress damage, suggesting that diabetic patients are at significantly increased risk of developing glaucoma [13-15]. According to a study done by the American diabetes association, the risk of glaucoma is 1.6 -4.7 times more in diabetics than in non-diabetic individuals. In our study that was continued for about 2 months, 62 patients who visited ophthalmology department OPD, Mayo hospital Lahore were examined and questioned individually. Among these 62 patients, 32.25% of patients were diagnosed with glaucoma while the prevalence of glaucoma in a study done in East Sikkim was found to be 20% [1]. Moreover, according to the Tema Eye Survey, the prevalence was 6.8% overall, increasing from 3.7% among 40 to 49 years old to 14.6% among those 80 years and older [16]. In consonance with our study and the results obtained from other studies suggest that prevalence is more among diabetics because, based on the study done by Amy E Cha et al, in which they compared diabetic adults with non-diabetics, they found that adults with diabetes are more likely to develop eye disorders including glaucoma, cataract and diabetic retinopathy [17]. The mean age of the patients that participated in our study was 56.04+12.09 years. And the age of diabetic patients is another highly important risk factor for glaucoma. There could be several reasons why the prevalence of glaucoma increases with age. One of the studies has shown that aging reduces the area of trabecular lumen that can lead to decreased aqueous outflow [18]. Age related retro bulbar hemodynamic changes may contribute to an increased risk of glaucoma [18]. As claimed by the study done on the adult population of Shahrud, Iran, glaucoma prevalence was 0.9% in the 40-44 years age group and significantly increased to 3.55% in the 60-64 years age group [19]. It indicates that subjects aged between 56-70 are more prone to develop glaucoma. According to our study, 85% of patients having glaucoma were poor socio-economically. That might be the reason for prevalence, as those patients could not afford proper medication and routine examination and this also becomes the reason for not detecting glaucoma and other eye problems earlier. In our study, out of the patients with glaucoma, 55% were males and 45% were females. So, we found that the risk of developing glaucoma is more among males as compared to females as proven by another study in which prevalence among males was slightly higher (4.41%) as compared to females (3.1%) [20]. So, based on sex distribution, patients having glaucoma are often males. Duration of diabetes is another factor that has a relationship with glaucoma. In our study, the number of years for which diabetes mellitus was present in glaucomatous patients was 7.1+7.45 years and as reported by one of the studies that 75% pf patients suffering from glaucoma were diabetics for 5 to 10 years and 25% had diabetes for less than 5 years [20]. However, only a few studies have been done before that assessed the duration of diabetes among patients suffering from glaucoma. Moreover, the patients in our study were both vegetarians and non-vegetarians, whereas in the study done by Jayanta T. et al, all the patients were vegetarians [21]. The fact that all the patients in their study where vegetarians might be because of their religious or cultural norms.
We assessed that only 3 diabetic patients having glaucoma reported a positive family history, but based on a study done by Divakar Gupta, MD, and Philip P. CHEN, MD, having a sibling with glaucoma has an odds ratio of 3.7% for primary open angle glaucoma [22]. In a study done in north east India, hereditary preponderance was 23.81% [23]. So, somehow, family history has a relationship with glaucoma. However, studies of family history and glaucoma may be prone to recall bias, which might explain widely differing prevalence rates in different studies. Moreover, a large number of people having glaucoma goes undiagnosed in the community. On the basis of ethnicity, all patients in our study were Punjabi. The reason behind this might be that we have conducted our study in a hospital located in Lahore, a city of the province of Punjab, Pakistan, where the majority of the population are Punjabi. Only 1 of 62 patients in our study was aware of the relationship between glaucoma and diabetes mellitus and it was also seen in a study done by Salih OAB et al. in Sudan where many were not aware of ophthalmic complications of diabetes [2]. This unawareness reflects the shortage in health education in the community. In keeping with all the studies done, people identified with glaucoma were unaware of this condition. That's why screening programs need to receive more attention. Screening programs for glaucoma in Pakistan is not effective and there are several reasons behind it. People might not get easy access to eye care clinics or maybe there is some lack in eye screening awareness and it results in a large number of patients remaining undiagnosed till they reach the advanced stage of the disease. That's why early detection will help us to reduce the prevalence of glaucoma.
Conclusion
This study throws light on the prevalence and demographic characteristics of glaucoma among diabetes mellitus patients in a tertiary care hospital in Lahore. The following conclusions were drawn from this study: A significant percentage of diabetic people developed glaucoma at various points in their life. The occurrence of glaucoma was more in the poor class people due to lack of available facilities for regular screening and knowledge about the disease. Hence, the above conclusions showed that patients with diabetes are at increased risk of glaucoma. This study also showed that the majority of the patients (except for one) who visited tertiary care had no previous knowledge of glaucoma as a disease and its relationship with other eye problems and diabetes. So, this study would document the prevalence of glaucoma in diabetes mellitus patients in Lahore and play a vital role in raising public awareness and preventing the progress of complications for which diabetes is a key factor.
Provenance and peer review: Not commissioned, externally peer reviewed.
Conflict of Interest: The authors declare no conflict of interest.
Source of Funding: No funding either internal or external sources was used in the research
Ethical Approval: The research was conducted after the ethical approval by the IRB committee of Mayo hospital
Consent: A well informed written consent was taken from the participants before the collection of the data
References
- Bhutia KL, Dhakal S, Bhutia SC. To find the prevalence of glaucoma in patients with diabetes mellitus attending tertiary care hospital, east Sikkim. Indian J Clin Exp Ophthalmol, 2018; 4(4): 447-449. doi: https://doi.org/10.18231/2395-1451.2018.0100
- Salih OAB, Hamed E. Open-angle glaucoma in diabetic patients’ prevalence and risk factors: a cross-sectional study in Sudan. Int J Res Med Sci, 2020; 8: 2205-2209. doi: http://dx.doi.org/10.18203/2320-6012.ijrms20202267
- Zhao YX, Chen XW. Diabetes and risk glaucoma: systematic review and a Meta-analysis of prospective cohort studies. Int JOphthalmol, 2017; 10(9): 1430-1435. Published 2017 Sep 18. doi: https://dx.doi.org/10.18240%2Fijo.2017.09.16
- Rajendran N, Isaac IA, Salor J, et al. Prevalence and risk factors associated with primary open angle glaucoma in diabetic patients in a tertiary care centre.Int. J.Med.Ophthalmol, 2021; 3(1): 01–4. https://doi.org/10.33545/26638266.2021.v3.i1a.51
- Dharmadhikari S, Lohiya K, Chelkar V, et al. Magnitude and determinants of glaucoma in type II diabetics: A hospital based cross-sectional study in Maharashtra India.Oman J, 2015; 8(1): 19-23. doi: https://dx.doi.org/10.4103%2F0974-620X.149858. PMID: 25709269; PMCID: PMC433353R
- Rivera C, Cantor E, Castillo A, Martinez A, Newball L, Rueda J, et al. Prevalence of Primary Open Angle Glaucoma among Patients with Diagnosis of Systemic Hypertension and Diabetes Mellitus: The Colombian Glaucoma Study. Open Journal of Ophthalmology, 2020; 10(02): 99-114.https://doi.org/10.4236/ojoph.2020.102012
- Khandekar R, Chauhan D, Yasir Z, et al. The prevalence and determinants of glaucoma among 40 years and older Saudi residents in the Riyadh Governorate (except the Capital) – A community-based survey. Saudi J Ophthalmol, 2019; 33(4): 332-337.https://doi.org/10.1016/j.sjopt.2019.02.006
- Yang D, Vien L. How diabetes and glaucoma intersect. Optom. times (online). 2021;13(8).
- Song BJ, Aiello LP, Pasquale LR. Presence and risk factors for glaucoma in patients with diabetes. Curr Diab Rep, 2016; 16(12): 124. https://dx.doi.org/10.1007%2Fs11892-016-0815-6
- McMonnies CW. Glaucoma history and risk factors. J Optom [Internet], 2017; 10(2): 71–78.
- 1 American Diabetes Association. Standards of medical care in diabetes - 2015. Diabetic Care, 2015; 38: S1-S9.
- 1 IBM Corp. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp; 2012.
- Bonovas S, Peponis V, Filioussi K, Diabetes mellitus as a risk factor for primary open- angle glaucoma: a meta-analysis. Diabetic Medicine, 2004; 21(6): pp.609-614.
- Zhou M, et al. “Diabetes mellitus as a risk factor for open-angle glaucoma: A systematic review and meta-analysis,” PLoS ONE, 2014; 9(8). https://doi.org/10.1371/journal.pone.0102972.
- International Journal of Ophthalmology. Diabetes and risk of glaucoma: systematic review and a Meta-analysis of prospective cohort studies, 2017.
- Budenz D, Barton K, Whiteside-de Vos J, Schiffman J, Bandi J, Nolan W, et al. Prevalence of Glaucoma in an Urban West African Population. JAMA Ophthalmology, 2013; 131(5): p.651.
- Cha AE, Villarroel MA, Vahratian A. Eye Disorders and Vision Loss Among U.S. Adults Aged 45 and Over with Diagnosed Diabetes, 2016-2017. NCHS Data Brief. 2019 Jul;(344):1-8. PMID: 31442198.
- Grzybowski, A. et al. “Primary open angle glaucoma and vascular risk factors: A review of Population Based Studies from 1990 to 2019,” Journal of Clinical Medicine, 2020; 9(3): p. 761. https://doi.org/10.3390/jcm9030761.
- Hashemi H, et al. “Prevalence and risk factors of glaucoma in an adult population from Shahroud, Iran,” Journal of Current Ophthalmology, 2019; 31(4): pp. 366–372. https://doi.org/10.1016/j.joco.2018.05.003.
- M MR, M M, K SR. “Prevalence of primary open angle glaucoma in diabetic patients,” IOSR Journal of Dental and Medical Sciences, 2017; 16(06): pp. 147–151. https://doi.org/10.9790/0853-160603147151.
- Jayanta T, Dipali DC, Santana S. Prevalence of glaucoma amongst diabetic patients attending a tertiary health care in North Eastern India. IJHRMLP, 2017; 03: 96-101.
- Gupta D, Chen PP. Glaucoma. Am Fam Physician. 2016 Apr 15;93(8):668-74. PMID: 27175839.
- Paul C, et al. “Prevalence of glaucoma in eastern India: The Hooghly River Glaucoma Study,” Indian Journal of Ophthalmology, 2016; 64(8): p. 578. Available at: https://doi.org/10.4103/0301-4738.191497.

