Barriers to Exclusive Breastfeeding among Lactating Mother in Rural Community of Bangladesh
Ripa Veronika Rozario1, Shahanaz Parveen2,*, Ferdous Jahan3 and Fahima Khatun4
1Nursing Instructor, Shaheed Tajuddin Ahmed Nursing College, Bangladesh
2Faculty, National Institute of Advanced Nursing Education and Research (NIANER), Bangladesh
3Faculty Depertment of Community Health Nursing, Faculty of Nursing, NIANER, Bangladesh
4Faculty Depertment of Womens Health and Midwifery Nursing, NIANER, Bangladesh
Received Date: 29/03/2023; Published Date: 03/07/2023
*Corresponding author: Shahanaz Parveen, MSN, RN, Faculty, NIANER, National Institute of Advanced Nursing Education and Research, Mugda, Dhaka, Bangladesh
Abstract
Background: Exclusive Breast Feeding (EBF) has been defined by the World Health Organization as the infant has receives only breast milk from his/her mother or a wet nurse, or expressed breast milk, and no other liquids or solids, with the exception of drops or syrups consisting of vitamins, mineral supplements or medicines.
Objective: The aim of the study is to assess the barrier to EBF among lactating mother in rural community of Bangladesh.
Methodology: A descriptive study design was carried out using a convenience sample size of 120 lactating mothers in EPI center of Shaheed Ahsan Ullah Master General Hospital Tongi, Gazipur. Data was collected by face-to-face interview from the participants. Descriptive statistics and bivariate analysis including ANOVA, t-test, and Pearson correlation were used in this study.
Result: The mean age of the participants was 21.42 years. Half (50.8%) of the participant was service holder and above half (65.8%) of the participants were primary educated. Most (84.2%) of the participants were Muslim and their monthly income average 26850 taka. More than half (65.8%) of the participants were mode of delivery by cesarean section and conduct by nurse 58.3%. The age of mother has significant positive correlation with family barriers to exclusive breastfeeding. Mother with higher age had more family barriers to exclusive breastfeeding.
Conclusion: The results would serve as a source of information for nursing education, services and community nurse to make the intervention for the community people in Bangladesh as well as the findings can also be used as basis for further studies.
Keywords: Barriers; Exclusive; Breastfeeding; Mother; Infant
Introduction
Worldwide breastfeeding is a wealth that provides short and long term advantages for infants; as well as mothers. Breast milk contains essential nutrients which is stimulate optimal physiological and psychological growth and development of infant [1]. In worldwide, exclusively breastfed among the infants of under 6 months of age are <40% [2]. Globally about 37% of infants are exclusively breastfed until the age of six months, which is indicated that early cessation of EBF is prevalent in low and middle income countries [3]. Exclusive Breastfeeding (EBF) has been defined as the infant has receives only breast milk from his/her mother or a wet nurse, or expressed breast milk, and no other liquids or solids, with the exception of drops or syrups consisting of vitamins, mineral supplements or medicines [4]. Rate of EBF varies by countries and regions. EBF rate is lower among the high-income countries than low and middle income countries. In 2014 United States of America and the United Kingdom breastfeeding rate was 19% and 1% respectively. The trends of six months EBF rates below 20% in high income countries. On the other hand six month EBF rate is close to achieve the WHO goal, varies from different countries like in China 28 % (2008), 63% in Uganda (2011), Sudan and Cambodia 41% and 74% respectively (2010), Pakistan 38% and Indonesia 42% (2012), Korea 89% (2009), 34% in Philippines (2008) [1]. In India, prevalence of EBF was 54.9% in 2018 [5]. In Bangladesh the rate of exclusive breastfeeding practice is around 61% percent with significant variation across several individual-, household, and community-level factors [6].
Improper feeding practice impaired infant growth and development [7]. Due to insufficient breastfed increased the risk of infectious morbidity and under-nutrition, as well as risks of childhood obesity, type 1 and type 2diabetes, leukemia, and sudden infant death syndrome [8]. Children morbidity and mortality is high in developing countries because of improper child fed practice, poverty, lack of nutrition knowledge, lack of care by caregivers, and infection [9]. EBF prevent diseases like diarrhea, fever and ARI [10]. EBF reduce the risk of sudden infant death syndrome [6]. Improper feeding of infants leading to their poor nutrition that is a significant problem and affecting socioeconomic progress in general developed and developing countries [7].
Children under 5 years of age 11.6 percent preventable death occur due to suboptimum breastfeeding [10]. In low and middle-income countries are universal (90%) coverage of breastfeeding is estimated to prevent around 13% of all deaths among children under five years of age [11]. EBF rate is residue low approximately universal in Bangladesh. There is tremendous attrition in breastfeeding with rapid urbanization. Bottle feeding provides upper hand over infant-mother bonding and psychological communication of mother with the newborn. The infant mortality and morbidity result is increase due to various diseases of attrition in breastfeeding practice and the import of Breast Milk Substitute (BMS) is imposing a considerable damage on the economy of this country as well. Breastfeeding is universal but prelacteal food and early initiative of supplementary food both hampered exclusive breastfeeding practice. EBF practice is significantly increase by breastfeeding counseling [12]. Benefits of EBF to the child include a reduction of the prevalence and/or severity of many infectious diseases such as diarrhea, otitis media, urinary tract and respiratory tract infections. EBF also found to decrease the incidence of overweight, obesity, type 1 diabetes mellitus, and asthma [2]. EBF increases the maternal-infant bonding and physical and psychological communication. It may reduce the risk of breast and ovarian cancers, and osteoporosis in the mother [13].
In the context of Bangladeshi culture, the majority of women are dominated by men and other in their family (such as husbands, their mothers, mothers-in-law, grandmothers, and other family members). Traditionally, a woman in Bangladesh derives her status from her family in child bearing and child rearing. For this reason, without support from family members, it may be difficult for lactating mothers to practice and maintain exclusive breastfeeding. Knowledge gained from this study could be beneficial for lactating mother health care providers, particularly nurses, to take initiatives to improve this situation in Bangladesh.
Methods
A descriptive exploratory study design was used to identify the barriers to EBF among lactating mother in selected Hospital. The approval was obtained from the Institutional Review Board (IRB) of NIANER and BSSMU and from Shaheed Ahsan Ullah Master General Hospital, Tongi, and Gazipur. The data were collected from in between November 2018 to February 2019. The convenience sampling method was used to recruit the participants. Potential participants were explained about details of the study and were informed that they had the right to withdraw from the study any time without any harm. Participants who decided to participate in the study were asked to sign the consent form. Total of 120 lactating mothers were selected based on the following inclusion criteria; the lactating mother with child under the six months; those who were present during data collection period and willing to participate in this study.
The questionnaire used to collect data included in Socio-demographic Characteristics of Mothers and Infants; and the Barriers to Exclusive Breastfeeding among Lactating Mothers. Questionnaires were 5-point Likert scale: 1= strongly disagree, 2= disagree, 3= undecided, 4= agree, 5 = strongly agree. The validity of the instrument was examined by three experts. Then the investigator modified the instrument based on experts’ recommendation. Reliability of the instrument was .62 tested by the Cronbach’s alpha coefficient.
Results
Socio-demographic Characteristics of Mothers and Infants
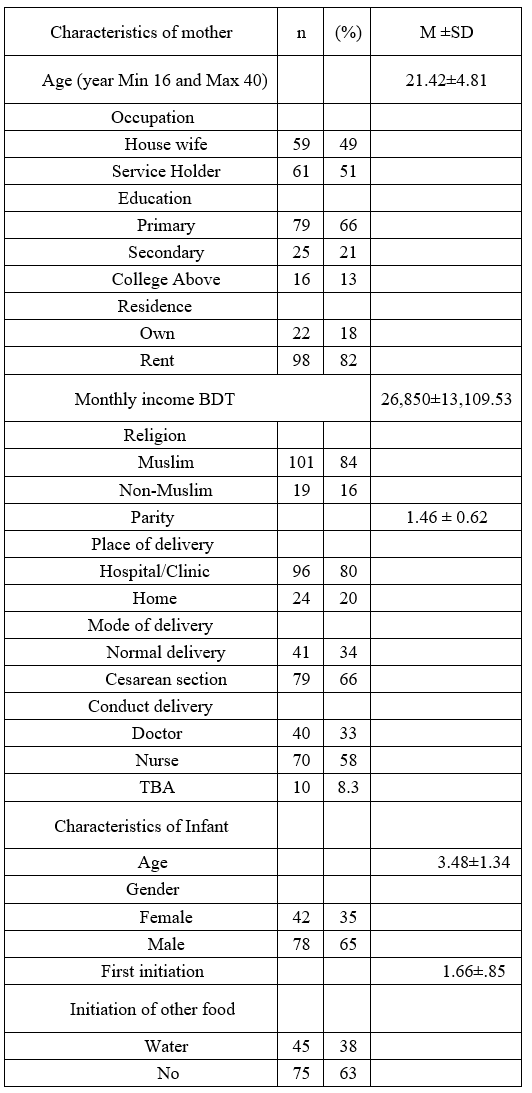
The mean age of the participants was, 21.42 years, and age ranged from 16 to 40 years. More than half (50.8%) of the participants were service holder and majority (65.8%) of them were primary educated. Most (81.7%) of the participants were lived in rented house and average monthly income were 26850 taka. Most of the (84.2%) participants were Muslim. Most (64.2%) of the participants places of delivery in hospital or clinic and only of 20% were in home. Nearly two third (65.8%) participants mode of delivery were cesarean section. More than half (58.3%) of the delivery were conducted by nurse and rest of doctor, and traditional birth attendant. The mean age of the infants was 3.48±1.34. Near about two-third 65% of the infant were male and 62.5% infants were not initiation of other food.
Table 1: Socio-demographic Characteristics of Mothers and Infants (120).
The Barriers to Exclusive Breastfeeding among Lactating Mothers:
Crake nipple and insufficient milk production was barrier to EBF that were agreed to 57.5% and 85.8% participants respectively. Most of the (77.55%) participants were agreed to breastfeeding was a tinning exercises the barrier to exclusive breastfeeding. More than 32% of the participants were undecide that neighbors pressure was the barrier to wean the baby. More than 67.5% participants were agreed to during breastfeeding insufficient food for mothers was the barrier to EBF. Nearly forty percent mother were undecide when the mother has tuberculosis they cannot breastfeed their baby. Nearly seventy eight percent participants agreed that baby was not breast feeding well to barriers to EBF. Most (73.3%) of the participants said that family members force to give water, formula milk, and honey to barriers to EBF. Above half (60%) of the participants said that mal position and attachment of the barriers to EBF. More than half (53.3%) of the participants said that the health care worker prescribe formula milk. Most (87.5%) of the participants said that lack of baby care facility of the barrier to EBF. Sixty five percent participants were agreed to insufficient facility to store breast milk at work place was the barrier to exclusive breast feeding. More than half (55.8%) of the participants were agreed to baby feed in public place was the barrier to EBF.
Table 2: Distribution of Barriers to Exclusive breast feeding.

Relationship between Socio-demographics Characteristics and Barriers to EBF of Participants
The age of mother has significant positive correlation with family barriers to EBF. The mother with higher age had more family barriers to EBF which is statistically significant (.036). It was also found that mother with higher number of parities had higher family barriers to EBF but it is not statistically significant (Table 3).
Table 3: Relationship between Socio-demographic Characteristics and Barriers to Exclusive Breastfeeding.

Discussion
The mean age of participants was 21.42 . The finding was similar in the study conducted in Gujarat; they found the maternal mean age was 24.6 years. This may the reason in India was situated in beside in Bangladesh [14]. More than half (50.8%) of the participants were service holder and house wife 49.2%. House wife mothers were more likely to exclusive breast fed their infants than working mothers; this finding was supported by Setegn et al., 2012, they found that, unemployed mothers were about 5 times more likely to breastfed exclusively as compared to employed mothers. This may attribute to worked mothers were away from the home and from their infants which make the breast feeding difficult [15]. Most (65.8%) of the participants were primary educated. It was in contrast of the study conducted in Kaneya, among lactating mothers, that study showed majority of the mother’s level of education was college and above hence (college 54.2%, primary 18.2%, secondary 20.3%) mothers could make better informed decision of infant feeding [16]. This is due to the reasonal variation of Kaneya.
The place of delivery, 84.2% of the participants was delivered their baby in hospital and or Clinic and only 15.5%.was home. One study conducted by Howlader, S. U., Razzak, A., & Raza, S. 2018, in Bangladesh, they found that the place of delivery was 75.5% is institutional delivery among them 37.7% in Clinic, 35.6% in Hospital, and 2.3% health care center) and one forth (24.5%) was delivered in home. It was nearly similar in the present study [17]. It is also similar in the study conducted by Limo, Fridah & Jebet, 2018, in Kenya, they found that the place of delivery in hospital 83.3% and home was only 16.7%. It may the reason Kenya is the midle income country [16]. The mode of delivery were above half (65.8%) of the participants were delivered by cesarean section and normal delivery were 34.2%. Another study found in Bangladesh, they found that 53.9% baby was deliverred normally and by cesarian section was 46.1%. This is due to place of delivery [17]. In contrast other studies results showed that normal delivery was 80.6% and 19.4% operative delivery in India [18]. Another study nn Kenya found that normal delivery 67.0%, cesarean section 13.3%, assist delivery 19.7% [16].
In the present study revealed that during delivery about half (58.3%) of the participants were conduct delivery by nurse, doctor 33.3% and TBA 8.3%. Similar result was found in the study conducted by Howlader, S. U., Razzak, A., & Raza, S. 2018, in Bangladesh, they found that 56.2% delivery conducted by health service personnel, 35.2% by trained traditional birth attendence (TTBA) and TBA 8.7% [17].
In this study the mean age of the infant was 3.48 month (SD=1.34). Similar result was found in the study conducted in Pakisthan, they found that the mean age of infants of group (62.1%) was of 2.2 months ± 0.7 and other group of infants (37.9%) was of mean age 5.2 months ± 0.6 [18]. This study result found that almost all (97.5%) of the participants were agreed to crake nipple was the barrier to exclusive breastfeeding. Other study also suported that Cracked nipples were the problem during the first week (31.9%) as well as during the rest of the first month and beyond the first month 36.5% and 30.3% respectively [19].Similar study was found that was conducted in Kenya, they found that majority (77.1%) of the participants were experienced sore or cracked nipples was the barrier to exclusive breastfeeding [16]. The present study revealed that all most (85.8%) the participants were agreed to insufficient milk production was the barrier to exclusive breastfeeding. The mothers stated that because of inadequate milk production they were not able to exclusively feed infants regularly. It is nearly similar to the study conducted in India found that insufficient milk production that 65.2% is significantly related to the barrier to exclusive breastfeeding. This is due to India is the nearer country of Bangladesh [20]. Many of them were using infant’s formula and cow’s milk to feed the infants. According to a study conducted in Pakistan 71% mothers had reported lack of sufficient milk production, while a cohort study performed internationally reported 80% mothers with insufficient breast milk [21]. This was approximately greater (24%) than our local value. Inadequacy of milk production in mothers could be of reasons such as not to eat well, drink juices, milk, water and other kind of liquid diet intake. Milk production could also be increased by feeding the child with the interval of two or three hours as documented by WHO, it might prove helpful to keep up milk production and comfort of both mother and child [22].
The present study showed that around half 46.75 % of the participants were experienced of painful and enlarged breasts was barriers to exclusive breastfeeding. Incontrast only 6% participants were experienced that painful and enlarged breasts was barriers to exclusive breastfeeding that was conductedin Kenya [22]. This study showed that about 67.55 participants were the insufficient food for mother of the barriers to exclusive breastfeeding. In another study in Uganda found that ‘Poverty makes me fail to buy food and so I don’t eat a balanced diet which limits the milk for the baby [23]. This study revealed that more than half (53.3%) of the participants were agreed to health care worker prescribe formula milk and only 9.2% participants were agreed to neighbors’ pressure to wean the baby which was the barriers to exclusive breastfeeding. In another study found that advice given by health care providers (4.9%) was the least common reason and advice given by relatives or neighbors (7.3%) was the second least common reason [23]. Most (73.3%) of the participants were forced from the family members to give water, formula milk, honey, during this period. In another study showed similar result that their participants (53%) were given to the infants was mainly milk and others (47%) included soft ugali, herbal medicine and fruits juice [16].
Conclusion
The policymakers, nurse and other healthcare workers, employers, staff in work places and the community need to be made aware of importance of exclusive breastfeeding. Breastfeeding promotion messages by the health sector should focus on alleviating the misconceptions mothers have on exclusive breastfeeding such as the perception of insufficient breast milk production and inappropriateness of expressing breast milk for infants to consume when mothers are away. It is time to make all work places breastfeeding friendly and to make feeding places available at all public places. Strategies approved by the health workers and Non-government Organizations should be implemented to encourage exclusive breastfeeding, targeting the key role players who are; fathers, traditional birth attendants and all grandmothers.
References
- Thepha T, Marais D, Bell J, Muangpin S. Facilitators and Barriers to Exclusive Breastfeeding in Thailand: A Narrative Review Journal of Community & Public Health Nursing, 2017; 3(1). doi:10.4172/2471-9846.1000160.
- Mensah KA, Acheampong E, Anokye FO, Okyere P, Appiah-Brempong E, Adjei RO. Factors influencing the practice of exclusive breastfeeding among nursing mothers in a peri-urban district of Ghana. BioMed Central research notes, 2017; 10: 1-7.
- Victoria CG, Bahl R, Barros AJ, França GV, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology mechanisms, and lifelong effect. The Lancet, 2016; 387(10017): 475-490.
- Hunegnaw MT, Gezie LD, Teferra AS. Exclusive breastfeeding and associated factors among mothers in Gozamin district, northwest Ethiopia: a community based cross-sectional study. International breastfeeding journal, 2017; 12: 1-8.
- Pareek S. Exclusive breastfeeding in India: an ultimate need of infants. Nursing Practice Today, 2019; 6(1): 4-6.
- Rahman MA, Khan MN, Akter S, Rahman A, Alam MM, Khan MA, et al. Determinants of exclusive breastfeeding practice in Bangladesh: Evidence from nationally representative survey data. Plos one, 2020; 15(7): e0236080.
- Berhanu Z, Alemu T, Argaw D. Predictors of inappropriate complementary feeding practice among children aged 6 to 23 months in Wonago District, South Ethiopia, 2017; case control study. BMC pediatrics, 2019; 19(1): 1-13.
- Stuebe A. The risks of not breastfeeding for mothers and infants. Reviews in obstetrics and gynecology, 2009; 2(4): 222.
- Ijarotimi OS. Determinants of childhood malnutrition and consequences in developing countries. Current Nutrition Reports, 2013; 2: 129-133.
- Khan MN, Islam MM. Effect of exclusive breastfeeding on selected adverse health and nutritional outcomes: a nationally representative study. BMC public health, 2017; 17: 1-7.
- Joshi PC, Angdembe MR, Das SK, Ahmed S, Faruque AS, Ahmed T. Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: a cross-sectional study. International Breastfeeding Journal, 2014; 9(1). doi:10.1186/1746-4358-9-7.
- Mihrshahi S, Oddy WH, Peat JK, Kabir I. Association between infant feeding patterns and diarrhoeal and respiratory illness: A cohort study in Chittagong, Bangladesh. International Breastfeeding Journal, 2008; 3(1): 28. doi: 10. 1186/1746-4358-3-28.
- Liu J, Leung P, Yang A. Breastfeeding and active bonding protects against children’s internalizing behavior problems. Nutrients, 2013; 6(1): 76-89.
- Chudasama R, Patel P, Kavishwar A. Breastfeeding initiation practice and factors affecting breastfeeding in South Gujarat region of India. The Internet Journal of family practice, 2009; 7(2).
- Setegn T, Belachew T, Gerbaba M, Deribe K, Deribew A, Biadgilign S. Factors associated with exclusive breastfeeding practices among mothers in Goba district, south east Ethiopia: a cross-sectional study. International Breastfeeding Journal, 2012; 7(1). doi:10.1186/1746-4358-7-17.
- Limo FJ, Kangogo M, Mutai J. Factors associated with exclusive breastfeeding among mothers with children aged six months and below attending Baringo County Refferal Hospital, Kabarnet, Kenya. East African Medical Journal, 2018; 94(3).
- Howlader SU, Razzak A, Raza S. Rate of home delivery and participation of traditional birth attendants is declining in selected areas of Dhaka city. MOJ Public Health, 2018; 7(2): 69-73.
- Bhanderi D, Pandya Y, Sharma D. Barriers to exclusive breastfeeding in rural community of central Gujarat, India. Journal of Family Medicine and Primary Care, 2019; 8(1): 54. doi:10.4103/jfmpc.jfmpc329_18.
- Babakazo P, Bosonkie M, Mafuta E, Mvuama N, Mapatano MA. Common breastfeeding problems experienced by lactating mothers during the first six months in Kinshasa. Plos one, 2022; 17(10): e0275477.
- Nasrullah M, Khan A, Khan MA, Safdar S. Barriers to exclusive breastfeeding in children under 6 months of age in district Kasur. Annals of Punjab Medical College, 2018; 12(1): 43-47
- Ibrahimm S, Ansari NS. Factors associated with failure of exclusive breastfeeding. Pak Jaoural Medical Health Science, 2006; 11: 24-26.
- World Health Organization. Guidelines on maternal, newborn, child and adolescent World Health Organization Guidelines, 2013; 1-3.
- Gitonga, Betty, Makena. Factors influencing exclusive breastfeeding of children for the first six months after birth. A case of thika level five hospital, Kiambu County, Kenya, 2014.
- Engebretsen IM, Moland KM, Nankunda J, Karamagi CA, Tylleskär T, Tumwine JK. Gendered perceptions on infant feeding in Eastern Uganda: continued need for exclusive breastfeeding support. International Breastfeeding Journal, 2010; 5(1): 13. doi:10.1186/1746-4358-5-13.

