Malignant Hypertension Unmasking Aortic Coarctation in a Young Adult
Sayarh Salma*, Karimou Bondabou Abdoul Wahab, Bakkali Tarik, Lekhel Brahim and Cherti Mohammed
Department of Vascular Surgery, Ibn Sina Rabat University Hospital, Mohamed V University of Rabat, Morocco
Received Date: 14/03/2023; Published Date: 12/06/2023
*Corresponding author: Sayarh Salma, Department of Vascular Surgery, Ibn Sina Rabat University Hospital, Mohamed V University of Rabat, Morocco
Summary
Coarctation of the aorta accounts for 6 to 8% of congenital heart disease. In 10 to 15% of cases they are diagnosed in adolescence or adulthood. It is a narrowing of the aortic lumen most often of the isthmus, around the intersection of the arterial ligament downstream of the birth of the left subclavian artery. Its pathophysiology describes a circumferential extension of ductal tissue during organogenesis culminating in the closure of the ductus arteriosus at an extension of intimal hyperplasia to the aortic isthmus resulting in native circumferential striction [4].
Patients may be asymptomatic which makes diagnosis difficult. Symptoms are related to high blood pressure of the upper hemisphere and poor perfusion of the lower hemibody. High blood pressure is the most common telltale sign. The characteristic murmur is systolic or continuous intense left interscapuloverterbral.
The 2D ETT makes it possible to visualize the coarctation by sternal route, specifies its anatomical shape and evaluates the impact on the left ventricle. In continuous Doppler by sternal route, a negative systolic flow with persistence of a diastole flow in case of severe coarctation. CT angiography and anigioMRI provide details on the location, diameter and length of the narrowed segment.
The treatment will be done by percutaneous transluminal balloon angioplasty with stenting or by surgical cure.
Its management is detailed in the ESC 2020 recommendations on congenital heart disease in adults [7].
Patients without surgery usually die before the age of 50 from complications of hypertension, early coronary artery disease, and aneurysms formation upstream or downstream of coarctation [1-3].
We report through the case of a 23-year-old patient, referred for HTA and diagnosed coarctation of the aorta the diagnostic and therapeutic modalities of this entity.
Introduction
Coarctation of the aorta accounts for 6 to 8% of congenital heart disease, with a male/female ratio of 2:1. It is a localized narrowing of the aortic lumen sitting most often at the level of the isthmus around the intersection of the arterial ligament downstream of the birth of the left subclavian artery. High blood pressure is the most common telltale sign; however, patients may have no other symptoms which sometimes makes diagnosis difficult. Symptoms vary depending on the severity of the abnormality. 10-15% of aortic coarctations are diagnosed in adolescence or adulthood. Diagnosis is based on echocardiography, CT angiography or MRI angiography. Treatment will be done by transluminal balloon angioplasty with stent placement or by surgical cure.
Patients without surgery usually die before the age of 50 from complications of high blood pressure, early coronary artery disease, and aneurysms formation upstream or downstream of coarctation [1-3].
Through this observation, we report the case of a 23-year-old patient, addressed in a context of hypertension, in whom transthoracic echocardiography, CT angiography and MRI angiography have established the diagnosis of coarctation.
This clinical case highlights the importance of blood pressure measurement during any examination and we discuss the diagnostic and therapeutic modalities of this entity.
Materials and Methods
We report the case of a 23-year-old patient with no notable pademiological history admitted to the medical emergency department for headache and vomiting in a context of apyrexia and worsening sharply for 48 hours. Clinical examination revealed high blood pressure at 270/140 mmHg in both arms. The cardiovascular examination found a systolic murmur at the aortic focus and an abolition of femoral pulses on both sides. The pleuropulmonary and neurological examination were without peculiarities. A cerebral CT scan was performed urgently revealing signs of hypertensive encephalopathy without hemorrhagic or ischemic signs The electrocardiogram objectified a regular sinus rhythm at 67 bpm with the presence of hypertrophy of the left ventricle (Sokoloff index at 37 mm) without repolarization disorders.
Medical management with Nicardipine IV allowed, under continuous monitoring, a significant decrease in blood pressure and an improvement in signs of neurological suffering.
The etiological assessment of this malignant hypertension revealed on transthoracic echocardiography a left ventricle site of septal hypertrophy with good systolic function and a left atrium slightly dilated but without dilation of the aorta Upward.
Thoracic angio-CT objectified a coarctation of the aorta located 39 mm from the birth of the subclavian aorta (Figure 1).
Therapeutically, the patient benefited from angioplasty with placement of a stent at the site of coarctation with simple postoperative follow-up (Figure 2, 3).
With a one-year hindsight, blood pressure is controlled (130/80 mmHg) under antihypertensive monotherapy (10 mg amlodipine per day).

Figure 1: CT angiography with multiplanar reconstruction objectifying the coarctation of the aorta.

Figure 2, 3: Postoperative control CT angio-CT (after placement of a stent).
Discussion
Moroganu was the first to describe in 1760 the coarctation of the aorta. It is said to be simple when isolated, and complex in the presence of lesions associated with congenital heart disease (bicuspidism, subaortic stenosis...), an aneurysm of the Willis polygon or a retroesophageal subclavian artery. The pathophysiology of isthmic coarctation remains hypothetical: 2 hypotheses [4].
During fetal life, a decrease in blood flow in the ascending thoracic aorta, secondary to obstructive lesion of the left heart or ventricular septal defect, would explain in some cases the presence of coarctation associated with hypoplasia of the aortic arch.
In other cases, a circumferential extension of ductal tissue during organogenesis leading at the time of closure of the ductus arteriosus to an extension of intimal hyperplasia to the aortic isthmus resulting in native circumferential striction.
The functional signs, not very specific, are related to a high blood pressure of the upper hemibody and poor perfusion of the lower hemibody. High blood pressure is the most common telltale sign. It is associated with a blood pressure gradient between the upper and lower limb of 20 mmHg in systole. This difference can be mitigated by the presenceof collateral circulation. The pulse of the lower limbs is decreased or abolished. The characteristic murmur is an intense left interscapulovertebral systolic or continuous murmur.
The complementary examinations have three objectives: the diagnosisic positive, the evaluation of the visceral impact and the search for associated lesions.
Chest radiography can also contribute to the diagnosis especially in older children and adults by objectifying the presence of costal erosions indicating collateral circulation.
Two-dimensional transthoracic ultrasound (ETT) makes it possible to visualize the coarctation by the sternal pathway, to specify its anatomical shape (diaphragm, hourglass) and to evaluate the impact on the left ventricle. In continuous Doppler, one can record, by sternal route, a negative systolic flow with persistence of a diastole flow in case of severe coarctation.
The transstenotic pressure gradient can be evaluated from the maximum values of these speed peaks using Bernouilli's formula. In color Doppler, the mosaic flow of coarctation takes on an hourglass appearance by resolving in the descending aorta where it is very turbulent. Echocardiography makes it possible to look for other associated malformations such as bicuspid aorticism.
CT angiography or anigioMRI are the examinations to be carried out in first line because in addition to the diagnosis of certainty, they provide details on the site, diameter and the length of the narrowed segment.
Chest CT angiography allows the precise localization of coarctation as well as a good analysis of collateral circulation and associated vascular abnormalities (aneurysms upstream or downstream of coarctation).
The MRI year is the method of choice for exploring the coarctation of the adult aorta.
It gives information similar to that of aortography and CT angiography and has the advantage of being able to be offered to patients with a contraindication to iodine injection.
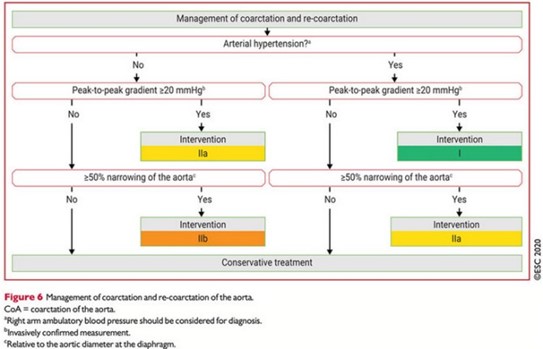
Its management is detailed in the ESC recommendations on congenital heart disease in adults, published in 2020.
The following are recommendations for intervention in case of coarctation of the aorta:
-Surgical or percutaneous repair of aortic coarctations is recommended in hypertensive patients with an increased non-invasive gradient confirmed by an invasive peak to peak gradient >20mmHg with a preference for percutaneous technique (with stenting if possible (class I)
- Percutaneous repair of aortic coarctations should be considered in normotensive patients with an increased non-invasive gradient, confirmed by an invasive peak-to-peak gradient >20 mmHg (Class IIa)
-Stenting remains indicated in hypertensive patients with a gradient < 20 mmHg but stenosis >or = 50% (class IIa)
In adults, transluminal angioplasty has seen a lot of progress in recent years. Indeed, in case of native coarctation with a favorable anatomy, angioplasty with placement of a stent has become the first-line treatment in several centers.
Surgical treatment consists of resection of the coarctation with terminoterminal suture of the upper and substenotic segments (Crafoord intervention).
Non-operated patients usually die before the age of 50 from complications of hypertension, early coronary artery disease, and aneurysms formation upstream or downstream of coarctation [1-3].
The long-term survival rate of patients operated on in adulthood is significantly lower than in the normal population [5,6]. This is related to earlier coronary artery disease, persistence of high blood pressure and the presence of possible aortic bicuspidism.
Conclusion
Coordination in young adults, treated or not, must be monitored for life because this pathology must be evoked in front of any hypertension of the young subject associated with a decrease in femoral pulse.
It reflects a global damage to the arterial wall sometimes responsible for long-term aneurysms, dissections and coronary and ventricular sequelae sometimes early.
Early diagnosis prevents the risk of persistent hypertension and especially reduces mortality related to associated complications.
The ESC recommendations detailed in 2020 the management of aortic coarctation in adults [7].
References
- Wells WJ, Prendergast TW, Berdjis F, et al. Repair of coarctation of the aorta in adults: The fate of systolic hypertension. Ann Thorac Surg, 1996; 61: 1168-1171.
- Aris A, Subirana T, Ferrés P, et al. Repair of aortic coarctation in patients more than 50 years of age. Ann Thorac Surg, 1999; 67: 1376-1379.
- Artigou J, Monsuez J. Coarctation of the aorta and interruption of the aortic arch. In: Cardiology and vascular diseases. Ed. Masson, 2007; 945-948.
- Morrow WR, Huhta JC, Murphy Jr DJ, et al. Quantitative morphology of the aortic arch in neonatal coarctation. J Am Coll Cardiol, 1986; 8: 616–620.
- Liberthson RR, Pennington DG, Jacobs ML, et al. Coarctation of the aorta: review of 234 patients and clari?cation of management problems. Am J Cardiol, 1979; 43: 835.
- Werning C, Schönbeck M, Widemann P, et al. Plasma rennin activity in patients with coarctation of the aorta. Comment on the pathogenesis of pre-stenotic hypertension. Circulation, 1969; 450: 731.
- ESC 2020 recommendations congenital heart disease of the adulte.

