The Different Degree of Severity Intrinsically Present in Each Type of Renal Lesions [Arteriolar Hyalinosis (Ah Score), Tubulo-Interstitial-Damage Score (TID Score), Global Glomerular Sclerosis (GGS%) are a Very Simple Predictor of Functional Outcome and High Blood Pressure Frequency in Glomerulonephritis Patients
Claudio Bazzi*
Retired from Nephrology and Dialysis Unit, San Carlo Borromeo Hospital, Italy
Received Date: 17/03/2023; Published Date: 09/06/2023
*Corresponding author: Claudio Bazzi, Retired from Nephrology and Dialysis Unit, San Carlo Borromeo Hospital, Via Pio II, 3, Milan, Italy
Abstract
Background: In chronic glomerulonephritis (GN) the patients have different types of renal lesions: the more frequent lesions are: Global Glomerular Sclerosis evaluated by percentage (GGS%); Tubulo- Interstitial-Damage evaluated by a score: tubular atrophy, interstitial fibrosis and inflammatory cell infiltration graded 0, 1 or 2 if absent, focal or diffuse (TID global score: 0-6); Arteriolar Hyalinosis evaluated by a score: 0, 1, 2, 3 if absent, focal, diffuse, diffuse with lumen reduction, respectively (AH global score 0- 3). The aim of the study was to assess the predictive value of outcome and high blood pressure according to the data of different severity in each type of renal lesion.
Methods: 363 patients were evaluated according to GGS%, 362 according to TID score, 361 according to AH score.
Results: Remission was 76% in patients with AH score=0; 80% in patients with TID score =0; 81% in patients with GGS % =0. Progression to ESRD was 48% in patients with TID score 5+6, 45% in GGS≥50% and 12% in AH score=3. The frequency of high blood pressure (BP1) was 38% vs 81% in AH =0 vs AH=3; 70% vs 86% in patients with TID score=0 vs TID score 5+6; 32% vs 83% in GGS=0% and GGS≥50%. In every type of renal lesion, the patients with remission and progression to ESRD are very different for baseline and last eGFR and for all proteinuric parameters.
Conclusion: In chronic glomerulonephritis and nephroangiosclerosis the different degrees of severity that characterize evry single renal lesion are a very simple and useful marker for prediction of functional outcome and high blood pressure frequency in comparison to renal lesion as such.
Introduction
The key role of renal lesions assessed by renal biopsy for CKD progression is widely recognized. In patients with glomerulonephritis are present different types of renal lesions; the more frequent are : Global Glomerular Sclerosis evaluated by percentage (GGS%), Tubulo-Interstitial-Damage valuable by a score of severity: tubular atrophy, interstitial fibrosis and inflammatory cell infiltration graded 0, 1 or 2 if absent, focal or diffuse (TID global score: 0-6); Arteriolar Hyalinosis evaluated by a score: 0, 1, 2, 3 if absent, focal, diffuse, diffuse with lumen reduction, respectively (AH global score 0-3). The role of each renal lesion may be considered as such or taking into account that each type of lesion includes different degree of severity that are useful to identify different percentages of the various outcomes. In the majority of previous studies, the prediction of functional outcome was mainly based on urinary excretion of various types of proteins with different molecular weight (2-28). To my knowledge no one publication evaluated the clinical significance of the different degree of severity of renal lesion. Aim of this study is to assess which is the percentage of the main functional outcome [Remission and Progression to ESRD] according to the different severity that characterizes evry renal lesions. The patients with 0 value in any type of renal lesion are associated with the highest percentage of Remission: 81% in GGS%=0, 80% in TID score=0, 76% in AH score=0; ESRD is 52% in TID score 5+6, 45% in GGS≥50% and 12% in AH score=3. The outcomes Remission and ESRD in each type of renal lesion are characterized by different values of clinical parameters such as age, baseline and last eGFR, percentage of GGS, values of TID and AH score, excretion of total proteinuria (TUP/C) and of proteins of different molecular weight.
Patients and Methods
The patient’s cohort included in the study was not selected. The patients attending the Nephrology and Dialysis Unit of San Carlo Borromeo Hospital, Milan, Italy, between January 1992 and April 2006 with renal biopsy diagnosis of GN were 469; the patients with acute reversible renal failure (ARF) at biopsy were excluded from analysis as do not meet the inclusion criterion (chronic glomerulonephritis); for the objective of the present study were selected only the patients with a follow up and outcome; thus 363 patients were the object of this study with the following types of chronic primary glomerulonephritis (GN), Nephroangiosclerosi (n. 20) and Lupus Nephritis (LN n. 36; [WHO classes: 3+5 n. 5, 4 n. 16; 5 n. 5, 3 n. 5, 2 n. 5)], (Table 1): Focal Segmental Glomerulosclerosis (FSGS, n. 38), Idiopathic Membranous Nephropathy (IMN, n. 81), Minimal change disease (MCD, n. 12), Membrano-proliferative glomerulonephritis (MPGN, n. 18); IgA nephropathy (IgAN, n. 124), Crescentic IgAN (CIgAN, n. 34), Nephroangosclerosis (n. 20). Inclusion criteria: at least six glomeruli in renal biopsy; typical features at light and immunofluorescence microscopy; no clinical signs of secondary GN except for LN. The patients evaluated by TID score are 362, by GGS% are 363 and by Arteriolar Hyalinosis score are 361. The functional outcome was available for the 361-363 patients with rather long follow up: mean 74±60 months (12-354). Four types of outcomes were considered: 1) Remission 2) progression to end-stage renal disease (ESRD); 3) eGFR reduction ≤ 50% of baseline). We decided to consider as outcomes Remission and ESRD. Diagnosis and clinical presentation of patients are reported in Table 1.
Table 1: Diagnosis of patients included in the study and comparison between normal and high blood pressure.


Laboratory Analysis
Proteinuria was measured in 24 hours urine collection and second morning urine sample by the Coomassie blue method (modified with sodium-dodecyl-sulphate) and expressed as 24/hour proteinuria and protein creatinine/ratio (mg urinary protein/g urinary creatinine: UP/C). Serum and urinary creatinine were measured enzymatically and expressed in mg/dL. Urinary albumin IgG and α1-microglobulin (α1m) were measured by immunonephelometry and expressed as urinary protein/creatinine ratio (IgG/C, Alb/C, α1m/C). Estimated glomerular filtration rate (eGFR) was measured by the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) formula (1). Three types of renal lesions as markers of disease severity were evaluated: percentage of glomeruli with global glomerulosclerosis (GGS%); extent of tubulo-interstitial damage (TID) evaluated semi-quantitatively by a score: tubular atrophy, interstitial fibrosis and inflammatory cell infiltration graded 0, 1 or 2 if absent, focal or diffuse (TID global score: 0-6) and extent of Arteriolar Hyalinosis (AH) evaluated semiquantitatively by a score: 0, 1, 2, 3 if absent, focal, diffuse, diffuse with lumen reduction, respectively (AH global score 0- 4) (Table 2).
Table 2: Functional Outcome and High Blood Pressure according to Arteriolar Hyalinosis (AH) score, Tubulo-interstitial damage (TID) score and percentages of Global Glomerular Sclerosis (GGS%).

Results
Remission was 76% in patients with AH score=0; 80% in patients with TID scor =0; 81% in patients with GGS %=0. Progression to ESRD was 48% in patients with TID score 5+6, 45% in GGS≥50% and 12% in AH score 3. The frequency of high blood pressure (BP1) was 38% vs 81% in AH =0 vs AH=3; 70% vs 86% in patients with TID score=0 vs TID score 5+6; 32% vs 83% in GGS=0% and GGS≥50%. In evry type of renal lesion the patients with remission were very different from patients with ESRD for baseline and last eGFR and for all proteinuric parameters.
Table 3: Percentages of Remission and progression to ESRD in patients according to Arteriolar hyalinosis score (n.361).
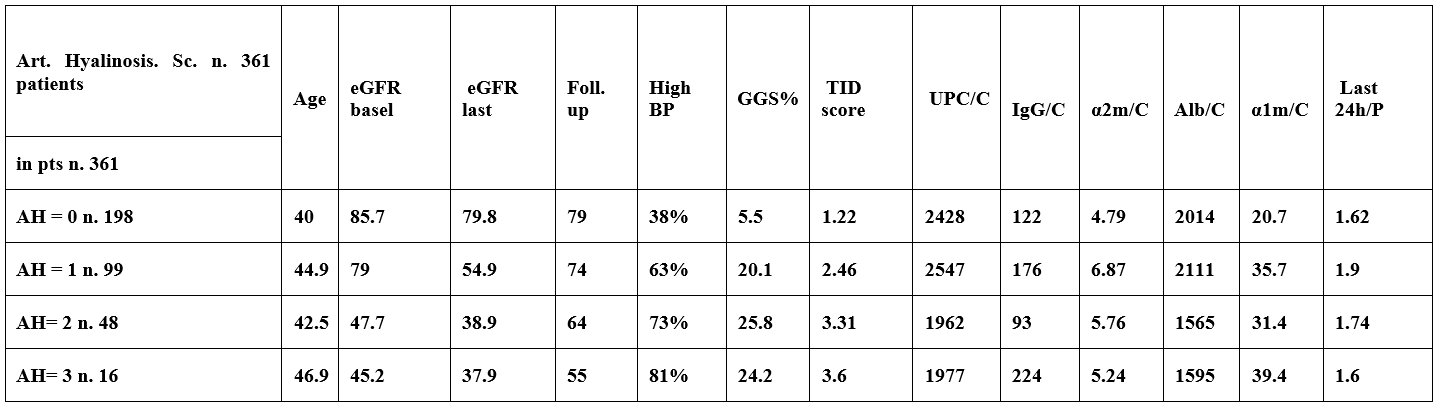
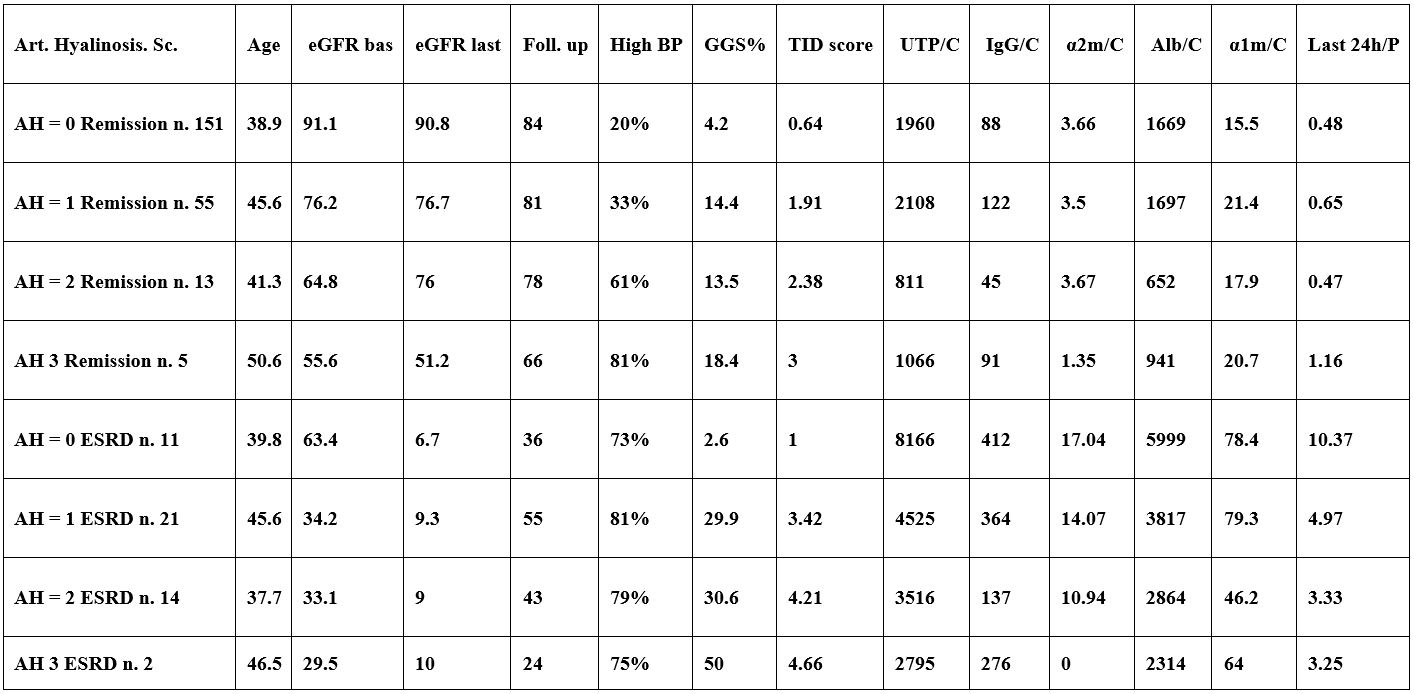
Table 4: Percentages of Remission and progression to ESRD in patients accoding to Tubulo-interstitial damage score (TID score n. 363 patients).
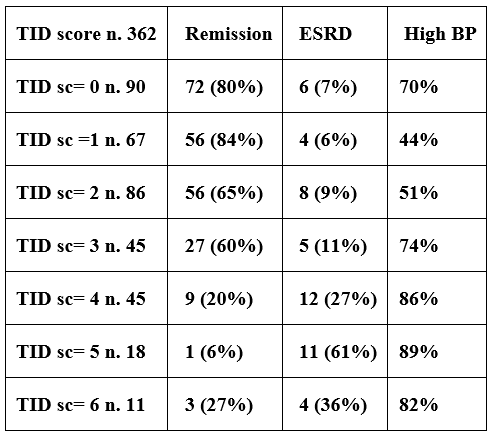
Table 5: Percentages of Remission and progression to ESRD in patients according to Tubulo-Interstitial Damage score (TID score n. 363 patients).

Table 6: Percentages of Remission and progression to ESRD according to percentage of Global Glomerular Sclerosis (GGS% n. 361 patients).
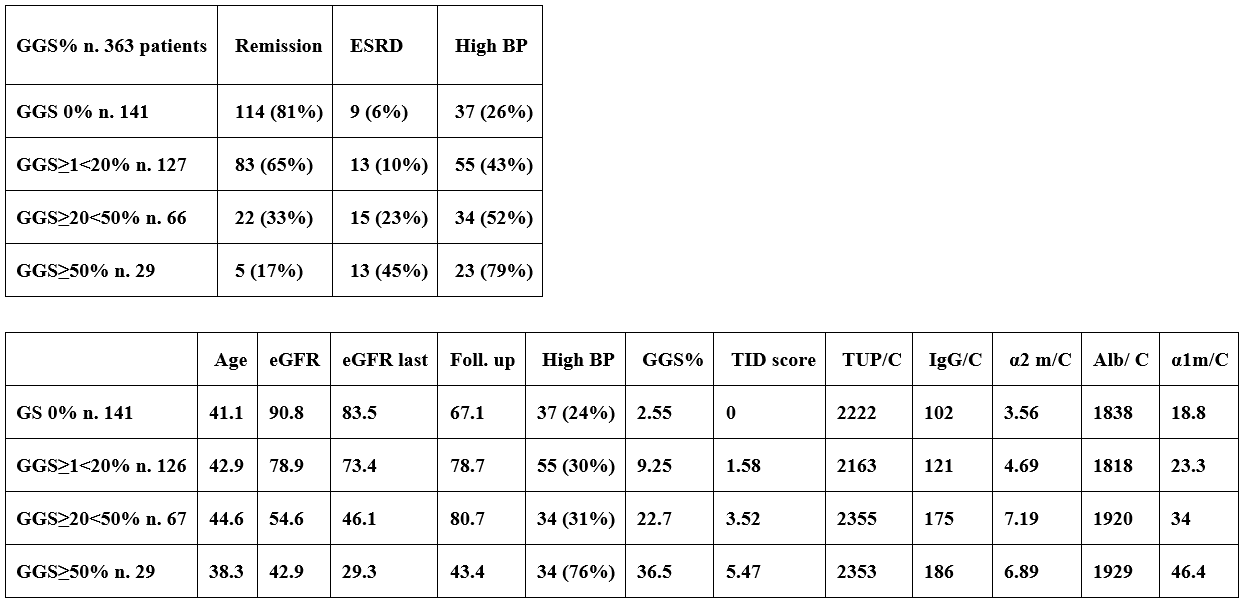
Table 7: Functional outcome in 67 patients with IMN, 35 with FSGS and 14 with MPGN according to Arteriolar Hyalinosis score.
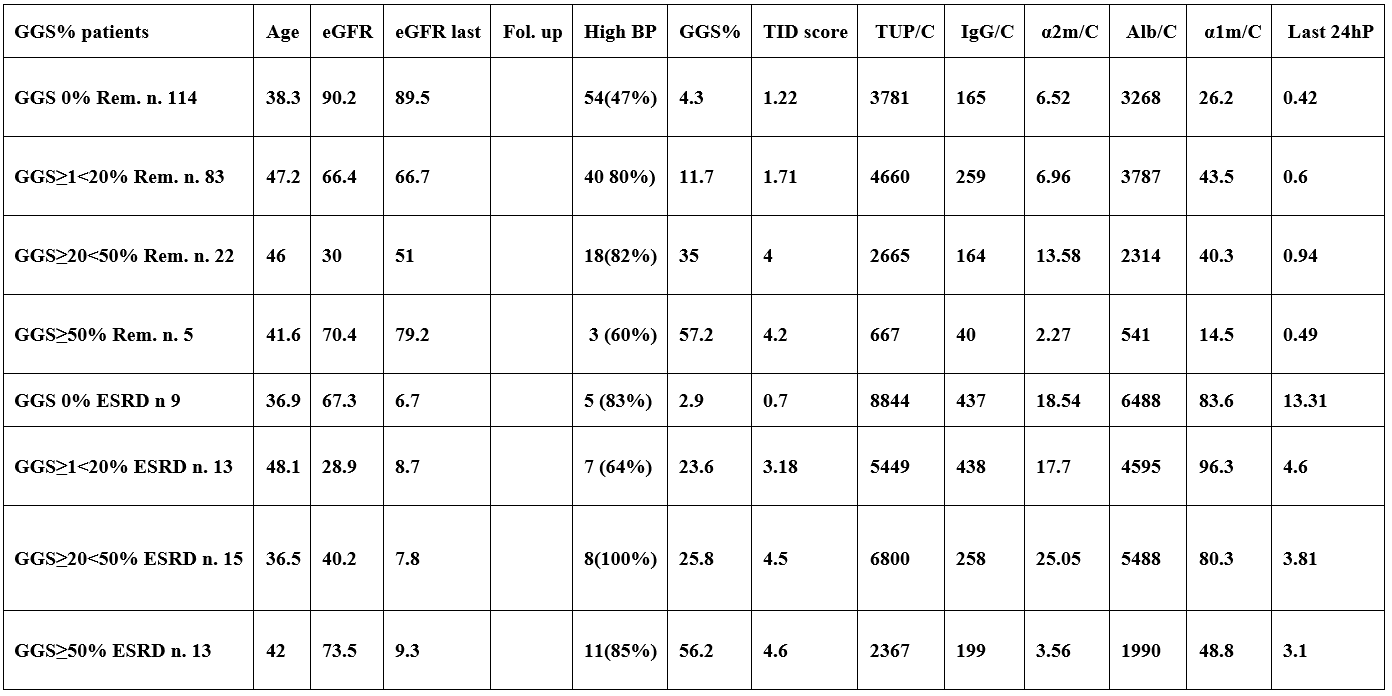
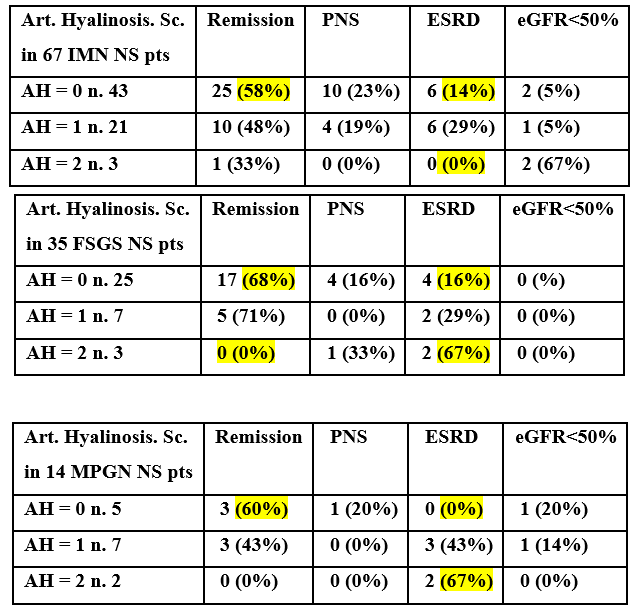
Table 8: Functional outcome according to renal lesions (AH sc., TID sc., GGS%) in combination.
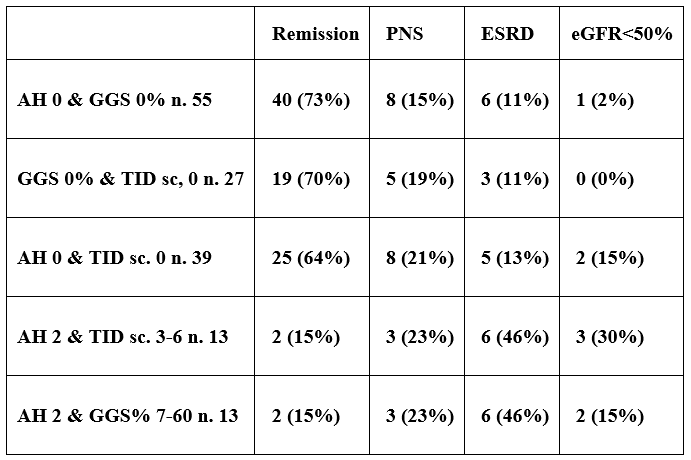
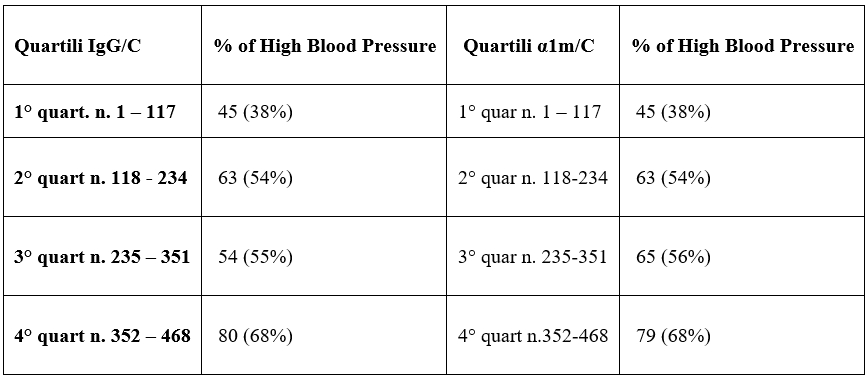
Table 9: Percentage of high blood pressure according to quartiles of IgG/C and α1m/C.
Comparison of patients with nephrotic syndrome (NS) and patients with non-nephrotic proteinuria (PP).
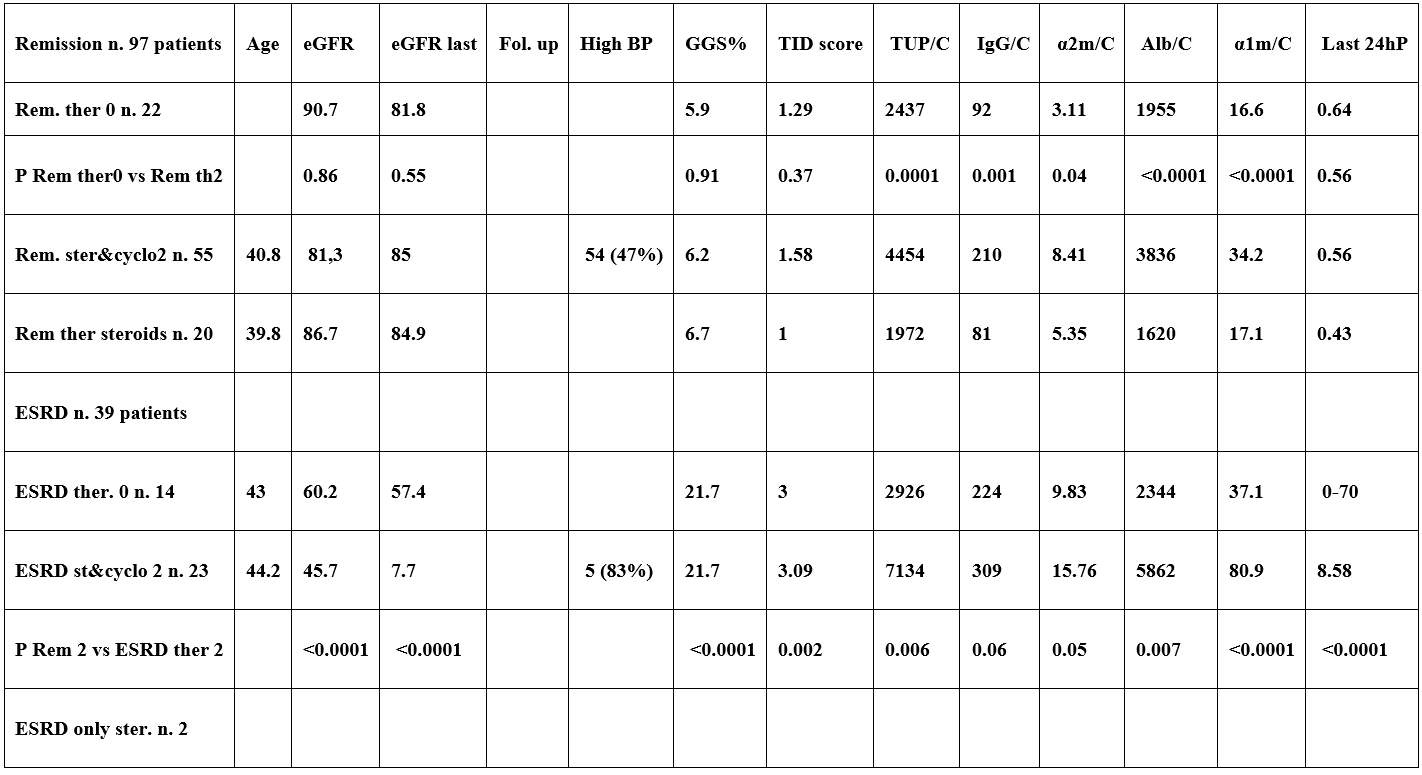
Table 10: Functional outcome in 67 patients with IMN, 35 with FSGS and 14 with MPGN according to Comparison of Remission and ESRD between patients with persistent nephrotic syndrome (NS: KI). according to: no therapy, teraphy with Steroids and Cyclophosphamide and teraphy with only steroids.

Discussion
The prediction of functional outcome and responsiveness to treatments in GN patients is of paramount importance in clinical practice. Several studies in last decades evaluated the predictive power of functional outcome of several proteinuric and novel molecular biomarkers but none of them reached 100% prediction. The identification of a new simple marker with high outcome prediction would be very useful also to assess responsiveness to new therapies introduced recently.
Conclusion
The 3 types of renal lesions considered in this study are all characterized by increasing severity that is for Global Glomerular Sclerosis the percentage of GGS; for Tubulo-Interstitial-Damage the evaluation of a score from 0 to 6 (indicated in the methods paragraph); also Arteriolar hyalinosis is evaluated by a score from 0 to 3 (indicated in methods paragraph); the various markers of severity of each type of renal lesion are a very simple predictors of functional outcome and percentage of high blood pressure.
References
- Levey AS, Stevens LA Schmid CH, Zhang YL, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann. Intern. Med, 2009; 150: 604–612.
- Branten AJ, du BUF-Vereijken, Klasen IS, Bosch FH, Feith GW, Hollander DA, et al. Urinary excretion of beta2-microglobulin and IgG predict prognosis in idiopathic membranous nephropathy: a validation study. J Am Soc Nephrol, 2005; 16: 169–174.
- Deegens JK, Wetzels JF. Fractional excretion of high- and low-molecular weight proteins and outcome in primary focal segmental glomerulosclerosis. Clin Nephrol, 2007; 68: 201–208.
- Tofik R, Torffvit O, Tippe B, Bakoush O. Increased urine IgM excretion predicts cardiovascular events in patients with type 1 diabetic nephropathy. BMC Med, 2009. doi:10.1186/1741-7015-7-39.
- Tofik R, Aziz R, Reda A, et al. The value of IgG-uria in predicting renal failure in idiopathic glomerular diseases. A long-term follow up study. Scand J Clin Lab Invest, 2011; 71: 123–128.
- Tofik R, Ekelund U, Torffvit O, Sward P, Rippe B, Bakoush O. Increased urinary IgM excretion in patients with chest pain due to coronary artery disease. BMC Cardiovasc Disord, 2013. doi:10.1186/1471-2261-13-72.
- van der Brand JAJG, Hofstra JM, Wetzels JFM. Low-molecular-weight proteins as prognostic markers in idiopathic membranous nephropathy. Clin J Am Soc Nephrol, 2011; 6: 2846–2853.
- Bakoush O, Grubb A, Rippe B, Tencer J. Urine excretion of protein HC in proteinuric glomerular diseases correlates to urine IgG but not to albuminuria. Kidney Int, 2001b; 60: 1904–1909.
- Bakoush O, Torffvit O, Rippe B, Tencer J. High proteinuria selectivity index based upon IgM is a strong predictor of poor renal survival in glomerular diseases. Nephrol Dial Transplant, 2001a; 16: 1357–1363.
- Bakoush O, Tencer J, Tapia J, Rippe B, Torffvit O. Higher urinary IgM excretion in type 2 diabetic nephropathy compared to type 1 diabetic nephropathy. Kidney Int, 2002; 61: 203–208.
- Bakoush O, Torffvit O, Rippe B, Tencer J. Renal function in proteinuric glomerular diseases correlates to the changes in urine IgM excretion but not to the changes in the degree of albuminuria. Clin Nephrol, 2003; 59: 345–352.
- Bakoush O, Segelmark M, Torffvit O, Ohlsson S, Tencer J. Urine IgM excretion predicts outcome in ANCA-associated renal vasculitis. Nephrol Dial Transplant, 2006; 21: 1263–1269.
- Irazabal MW, Eirin A, Lieske J, et al. Low- and high-molecular weight proteins as predictors of response to rituximab in patients with membranous nephropathy: a prospective study. Nephrol Dial Transplant, 2013; 28: 137–146.
- Bazzi C, Petrini C, Rizza V, Paparella M, Pisano L, D’Amico G. In Membrano-Proliferative Glomerulonephritis (MPGN) Fractional Excretion of IgG Correlates with Tubulo-Interstitial Damage and Predicts ESRF and Remission in Response to Therapy. Journal of American Society of Nephrology, Renal Week, 2002.
- D’Amico G, Bazzi C. Pathophysiology of proteinuria. Kidney Int, 2003a; 63: 809–825.
- Bazzi C, Petrini C, Rizza V, Napodano P, Paparella M, Arrigo G, et al. Fractional excretion of IgG predicts renal outcome and response to therapy in primary focal segmental glomerulosclerosis: A pilot study. Am J Kidney Dis, 2003; 41:328–335.
- Bazzi C, Rizza V, Raimondi S, et al. In crescentic IgA nephropathy fractional excretion of IgG in combination with nephron loss is the best predictor of progression and responsiveness to immunosuppression. Clin J Am Soc Nephrol, 2009; 4: 929–935.
- Park EY, Kim TY. Fractional excretion of protein may be a useful predictor of decline of renal function in pan-chronic kidney diseases. Nephrol Dial Transplant, 2011; 26: 1746–1747.
- Mc Quarrie EP, Shakerdi L, Jardine AG, et al. Fractional excretions of albumin and IgG are the best predictors of progression in primary glomerulonephritis. Nephrol Dial Transplant, 2011; 26: 1563–1569.
- Bazzi C, Rizza V, Casellato D, et al. Validation of some pathophysiological mechanisms of the CKD progression theory and outcome prediction in IgA nephropathy. J Nephrol, 2012; 25: 810–818.
- Bazzi C, Rizza V, Casellato D, et al. Urinary IgG and α2-macroglobulin are powerful predictors of outcome and responsiveness to steroids and cyclophosphamide in idiopathic focal segmental glomerulosclerosis with nephrotic syndrome. Biomed Res Int, 2013. doi:10.1155/2013/941831.
- Bazzi C, Rizza V, Casellato D, Tofik R, Berg AL, Gallieni M, et al. Fractional excretion of IgG in idiopathic membranous nephropathy with nephrotic syndrome: a predictive marker of risk and drug responsiveness. BMC Nephrol, 2014. doi:10.1186/1471-2369-15-74.
- Gentile G, Remuzzi G. Novel Biomarkers for Renal Diseases? None for the moment (but one). J Biomolecular Screening, 2016; 21: 655-670.
- Madhav C. Menon, Peter Y Chuang, Cijiang John He. The Glomerular Filtration Barrier: Components and Crosstalk. Int J Nephrol, 2012; doi:10.1155/2012/749010
- Haraldsson B, Nystrom J, Deen WM. Properties of the glomerular barrier and mechanisms of proteinuria. Physiol Rev, 2008; 88: 451–487.
- Miner JH. Glomerular basement membrane composition and filtration barrier. Pediatr Nephrol, 2011; 26: 1413–1417.
- Hiroshi Kawachi, Yoshivasu Fukusumi. New insight into podocyte slit diaphragm, a therapeutic target of Proteinuria. Clin Exp Nephrol, 2020; 24(3): 193-204.
- Chen Y, Schieppati A, Cai G, et al. Immunosuppression for membranous nephropathy: a systematic review and meta-analysis of 36 clinical trials. Clin J Am Soc Nephrol, 2013; 8: 787–796.

