Assessment of Responsiveness to No Treatment (ther. 0), Treatment with Steroids and Cyclophosphamide (ther. 2), Treatment with Steroids Alone (ther. 3) in 177 Patients with Glomerulonephritis and Nephrotic Syndrome (NS)
Claudio Bazzi*
Retired from Nephrology and Dialysis Unit, San Carlo Borromeo Hospital, Italy
Received Date: 17/03/2023; Published Date: 08/06/2023
*Corresponding author: Claudio Bazzi, Retired from Nephrology and Dialysis Unit, San Carlo Borromeo Hospital, Via Pio II, 3, Milan, Italy
Abstract
Background: The patients with glomerulonephritis and nephrotic syndrome (NS) are heterogeneous for renal function, type and severity of renal lesions and urinary excretion of proteins with different molecular weight. The patients after biopsy have different functional outcomes: remission (24-hour proteinuria <2.0 g/24 hour); persistent nephrotic syndrome with normal or decreasing renal function; progression to end stage renal disease (ESRD); reduction of eGFR < 50% of baseline.
Methods: Aim of the present study is the evaluation of functional outcome according to treatments. Three types of treatment were considered: no treatment (ther. 0), treatment with immuno-suppressive drugs steroids and cyclophosphamide in combination, (ther. 2); treatment with steroids alone (ther. 3). It is interesting to assess the functional outcome according to these 3 types of therapy and the clinical, functional, histological and proteinuric parameters associated with the different outcomes.
Results: 22 patients reached Remission after (ther. 0), 55 patients reached remission after (ther. 2); 20 patients reached remission after (ther. 3). The comparison of 22 remission patients with (ther. 0) with 55 remission patients with (ther. 2) show no significant differences for baseline and last eGFR, GGS%, TID score and AH score; otherwise, the 22 patients with (ther. 0) show highly significant lower values of TUP/C (0.0001), IgG/C (0.001), α2m/C (0.04), Alb/C (<0.0001), α1m/C (<0.0001) (Table 1).
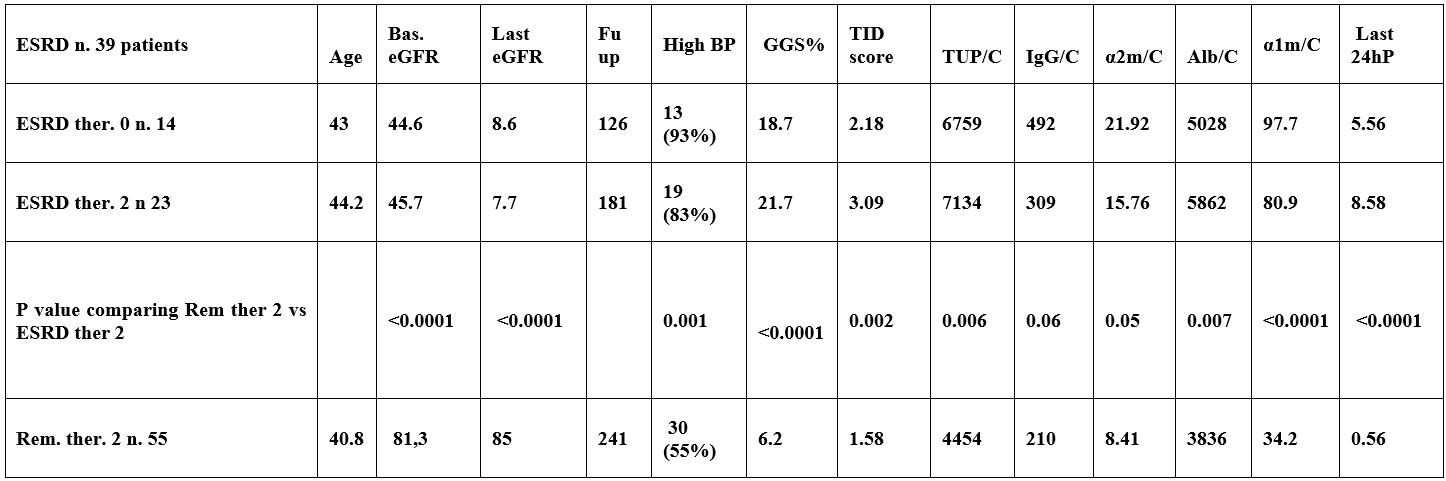
39 patients progressed to ESRD, 14 with (ther. 0), 23 with (ther. 2) and 2 with (ther. 3). The patients progressing to ESRD with (ther. 2) compared with patients reaching Remission with (ther. 2) showed that the ESRD patients treated with (ther.2) have significant lower value of baseline eGFR (<0.0001) and significant higher values of histologic and proteinuric parameters: TUP/C (0.006), IgG/C (0.06), α2m/C (0.05), Alb/C (<0.007), α1m/C (<0.0001) and last 24h P(<0.0001) (Table 1).
Conclusion: The decision to treat the NS patients with immunosuppressive treatment with steroids and cyclophosphamide may be dependent on the evaluation of functional, histologic and proteinuric parameters.
Introduction
The patients with glomerulonephritis and nephrotic syndrome (NS) are heterogeneous for renal function, type and severity of renal lesions and urinary excretion of proteins with different molecular weight. The patients followed for rather long time after biopsy may have different functional outcomes: remission (24-hour proteinuria <2.0 g/24 hour); persistent nephrotic syndrome with normal or decreasing renal function; progression to end stage renal disease (ESRD); reduction of eGFR < 50% of baseline value. Several articles showed that high urinary excretion of some proteins is associated with progression. Aim of the present study is the evaluation of functional outcome according to treatment [1-5]. Three types of treatment were considered: no treatment (ther. 0), treatment with immuno-suppressive drugs such as steroids and cyclophosphamide in combination (ther. 2); treatment with steroids alone, (ther. 3). It will be interesting to assess the functional outcome according to these 3 types of therapy and the clinical, functional, histological and proteinuric parameters associated with the different type of outcome. The first aim of the study was to compare all parameters in patients reaching Remission without treatment with those reaching Remission after treatment with steroids and cyclophosphamide. A second aim was to compare the patients reaching Remission with treatment with steroids and cyclophosphamide in comparison to patients reaching ESRD notwithstanding a treatment with Steroids and Cyclophosphamide [6-9].
Patients and Methods
Between January 1992 and april 2006 469 patients performed renal biopsy; 177 have nephrotic syndrome (NS: proteinuria: ≥3.5 g/24 hour) (follow up 87.2±75.5 months) and 203 have persistent non-nephrotic proteinuria (PP). In evry type of outcome according to type of therapy several clinical, functional, histological and proteinuric parameters were evaluated: age, baseline eGFR, last eGFR, percentage of Global Glomerular sclerosis (GGS%). degree of Tubulo-Interstitial-Damage evaluated by a score from 0 to 6 (TID score 0-6) and degree of Arteriolar Hyalinosis evaluated by a score from 0 to 3 (AH score 0-3) and the urinary excretion of several proteins of different molecular weight expressed as mg of protein per g of urinary creatinine: Total Urinary proteins (TUP/C), IgG/C, α2m/C, Alb/C, α1m/C, last 24-hour proteinuria [10-15]. The functional outcome was: Remission reached in 97 patients: 22 patients untreated with immuno-suppression (ther. 0); 55 treated with Steroids and Cyclophosphamide (ther. 2) and 20 treated with Steroids alone (ther. 3). Progression to ESRD was observed in 39 patients, 14 untreated with immuno-suppression (ther. 0), 23 treated with Steroids and Cyclophosphamide (ther. 2) and 2 with steroids alone (ther. 3). The first aim of the study was to compare all parameters in patients reaching Remission without treatment (ther. 0) with those reaching Remission with treatment with steroids and cyclophosphamide (ther. 2) . The second aim was to compare the patients reaching Remission with treatment with (ther .2) with patients reaching ESRD notwithstanding a treatment with immuno-suppression with Steroids and Ciclophosphamide(ther 2) [16-19].
Results
22 patients reached Remission without (ther. 0), 55 patients reached remission after (ther. 2); 20 patients reached remission after (ther. 3). The comparison of 22 patients with (ther. 0) with 55 patients with therapy (ther. 2) show no significant differences for baseline and last eGFR, GGS%, TID score and AH score; otherwise, the 22 patients with (ther.0) show significantly lower values of TUP/C (0.0001), IgG/C (0.001), α2m/C (0.04), Alb/C (<0.0001), α1m/C (<0.0001) (Table 1).
39 patients progressed to ESRD, 14 with (ther. 0), 23 with (ther. 2) and 2 with (ther.3). The comparison of patients progressing to ESRD with therapy (2) with patients reaching Remission with therapy (2) showed that the ESRD patients treated with therapy (2) are characterized by significant lower value of baseline eGFR (<0.0001) and significant higher values of GGS% (<0.0001), TID score (0.002), AH score (<0.0001) and significant higher values of all proteinuric parameters :TUP/C (0.006), IgG/C (0.06), α2m/C (0.05), Alb/C(<0.007), α1m/C (<0.0001) and last value of UPT/C (<0.0001) (Table 2) Taken toghether these result show that spontaneous Remission in untreated patients is associated with significantly lower values of all proteinuric markers in comparison to patients reaching Remission after (ther. 2) that show higher values of all proteinuric markers; thus Remission is possible without treatment in patients with low values of all proteinuric markers. Progression to ESRD in patients treated with (ther. 2) show that the patients may reach ESRD notwithstanding (ther. 2); these patients have significantly lower value of baseline eGFR and significantly higher values of all histologic and proteinuric parameters [20-22].
Table 1: Comparison of functional. histologic and proteinuric parameters in patients reaching remission without therapy (ther. 0) and patients reaching remission after treatment with steroids and Cyclophosphamide (ther. 2). The patients reaching Remission without treatment show high significantly lower values of all proteinuric parameter.
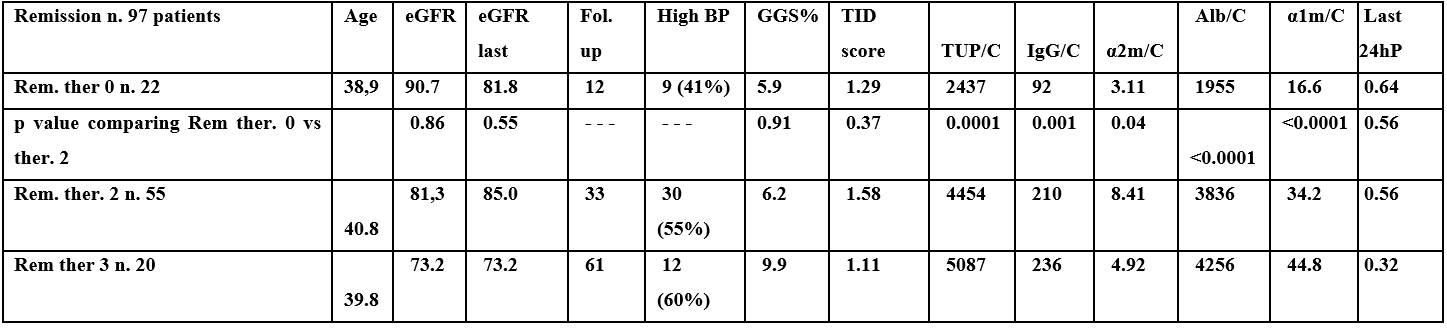
Table 2. Comparison of functional. histologic and proteinuric parameters in 55 patients reaching Remission after treatment with steroid and cyclophosphamide (ther. 2) and 23 patients progressing to ESRD notwithstanding treatment with Steroids and Cyclophosphamide (ther. 2). The ESRD patients show lower value of baseline eGFR and significantly higher values of histologic and proteinuric parameters.
Conclusion
The decision to treat the NS patients with immunosuppressive treatment with steroids and cyclophosphamide may be dependent on the evaluation of functional, histologic and proteinuric parameters.
References
- Levey AS, Stevens LA Schmid CH, Zhang YL, et al. CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann. Intern. Med, 2009; 150: 604–612.
- Branten AJ, du BUF-Vereijken, Klasen IS, Bosch FH, Feith GW, Hollander DA, et al. Urinary excretion of beta2-microglobulin and IgG predict prognosis in idiopathic membranous nephropathy: a validation study. J Am Soc Nephrol, 2005; 16: 169–174.
- Deegens JK, Wetzels JF. Fractional excretion of high- and low-molecular weight proteins and outcome in primary focal segmental glomerulosclerosis. Clin Nephrol, 2007; 68: 201–208.
- Tofik R, Torffvit O, Tippe B, Bakoush O. Increased urine IgM excretion predicts cardiovascular events in patients with type 1 diabetic nephropathy. BMC Med, 2009. doi:10.1186/1741-7015-7-39.
- Tofik R, Aziz R, Reda A, et al. The value of IgG-uria in predicting renal failure in idiopathic glomerular diseases. A long-term follow up study. Scand J Clin Lab Invest, 2011; 71: 123–128.
- Tofik R, Ekelund U, Torffvit O, Sward P, Rippe B, Bakoush O. Increased urinary IgM excretion in patients with chest pain due to coronary artery disease. BMC Cardiovasc Disord, 2013. doi:10.1186/1471-2261-13-72.
- van der Brand JAJG, Hofstra JM, Wetzels JFM. Low-molecular-weight proteins as prognostic markers in idiopathic membranous nephropathy. Clin J Am Soc Nephrol, 2011; 6: 2846–2853.
- Bakoush O, Grubb A, Rippe B, Tencer J. Urine excretion of protein HC in proteinuric glomerular diseases correlates to urine IgG but not to albuminuria. Kidney Int, 2001b; 60: 1904–1909.
- Bakoush O, Torffvit O, Rippe B, Tencer J. High proteinuria selectivity index based upon IgM is a strong predictor of poor renal survival in glomerular diseases. Nephrol Dial Transplant, 2001a; 16: 1357–1363.
- Bakoush O, Tencer J, Tapia J, Rippe B, Torffvit O. Higher urinary IgM excretion in type 2 diabetic nephropathy compared to type 1 diabetic nephropathy. Kidney Int, 2002; 61: 203–208.
- Bakoush O, Torffvit O, Rippe B, Tencer J. Renal function in proteinuric glomerular diseases correlates to the changes in urine IgM excretion but not to the changes in the degree of albuminuria. Clin Nephrol, 2003; 59: 345–352.
- Bakoush O, Segelmark M, Torffvit O, Ohlsson S, Tencer J. Urine IgM excretion predicts outcome in ANCA-associated renal vasculitis. Nephrol Dial Transplant, 2006; 21: 1263–1269.
- Irazabal MW, Eirin A, Lieske J, et al. Low- and high-molecular weight proteins as predictors of response to rituximab in patients with membranous nephropathy: a prospective study. Nephrol Dial Transplant, 2013; 28: 137–146.
- Bazzi C, Petrini C, Rizza V, Paparella M, Pisano L, D’Amico G. In Membrano-Proliferative Glomerulonephritis (MPGN) Fractional Excretion of IgG Correlates with Tubulo-Interstitial Damage and Predicts ESRF and Remission in Response to Therapy. Journal of American Society of Nephrology, Renal Week, 2002.
- D’Amico G, Bazzi C. Pathophysiology of proteinuria. Kidney Int, 2003a; 63: 809–825.
- Bazzi C, Petrini C, Rizza V, Napodano P, Paparella M, Arrigo G, et al. Fractional excretion of IgG predicts renal outcome and response to therapy in primary focal segmental glomerulosclerosis: A pilot study. Am J Kidney Dis, 2003; 41: 328–335.
- Bazzi C, Rizza V, Raimondi S, et al. In crescentic IgA nephropathy fractional excretion of IgG in combination with nephron loss is the best predictor of progression and responsiveness to immunosuppression. Clin J Am Soc Nephrol, 2009; 4: 929–935.
- Park EY, Kim TY. Fractional excretion of protein may be a useful predictor of decline of renal function in pan-chronic kidney diseases. Nephrol Dial Transplant, 2011; 26: 1746–1747.
- Mc Quarrie EP, Shakerdi L, Jardine AG, et al. Fractional excretions of albumin and IgG are the best predictors of progression in primary glomerulonephritis. Nephrol Dial Transplant, 2011; 26: 1563–1569.
- Bazzi C, Rizza V, Casellato D, et al. Validation of some pathophysiological mechanisms of the CKD progression theory and outcome prediction in IgA nephropathy. J Nephrol, 2012; 25: 810–818.
- Bazzi C, Rizza V, Casellato D, et al. Urinary IgG and α2-macroglobulin are powerful predictors of outcome and responsiveness to steroids and cyclophosphamide in idiopathic focal segmental glomerulosclerosis with nephrotic syndrome. Biomed Res Int, 2013. doi:10.1155/2013/941831.
- Bazzi C, Rizza V, Casellato D, Tofik R, Berg AL, Gallieni M, et al. Fractional excretion of IgG in idiopathic membranous nephropathy with nephrotic syndrome: a predictive marker of risk and drug responsiveness. BMC Nephrol, 2014. doi:10.1186/1471-2369-15-74.

