Lifelong Aspirin Even in Childhood in Sickle Cell Diseases
Mehmet Rami Helvaci1,*, Feryal Bastaci2, Gozde Yarasir Aydin2, Hava Fatma Kucukbesleme2, Abdulrazak Abyad3 and Lesley Pocock4
1Specialist of Internal Medicine, Turkey
2Ministry of Health of Turkey, Turkey
3Middle-East Academy for Medicine of Aging, Lebanon
4Medi-WORLD International, Australia
Received Date: 07/03/2023; Published Date: 19/05/2023
*Corresponding author: Prof Dr Mehmet Rami Helvaci, MD, Specialist of Internal Medicine, Turkey
Abstract
Background: Sickle Cell Diseases (SCDs) are severe inflammatory processes on vascular endothelium, particularly at the capillary level since the capillary system is the main distributor of hardened Red Blood Cells (RBCs) into the tissues.
Methods: All patients with the SCDs were included.
Results: We studied 222 males and 212 females with similar ages (30.8 vs 30.3 years, p>0.05, respectively). Disseminated teeth losses (5.4% vs 1.4%, p<0.001), ileus (7.2% vs 1.4%, p<0.001), cirrhosis (8.1% vs 1.8%, p<0.001), leg ulcers (19.8% vs 7.0%, p<0.001), digital clubbing (14.8% vs 6.6%, p<0.001), coronary heart disease (18.0% vs 13.2%, p<0.05), chronic renal disease (9.9% vs 6.1%, p<0.05), chronic obstructive pulmonary disease (25.2% vs 7.0%, p<0.001), and stroke (12.1% vs 7.5%, p<0.05) were all higher but not acute chest syndrome (2.7% vs 3.7%), pulmonary hypertension (12.6% vs 11.7), deep venous thrombosis and/or varices and/or telangiectasias (9.0% vs 6.6%), and mean age of mortality (30.2 vs 33.3 years) in males (p>0.05 for all).
Conclusion: The hardened RBCs-induced capillary endothelial damage, inflammation, edema, and fibrosis are initiated at birth, and terminate with diffuse tissue hypoxia and multiorgan insufficiencies even at childhood in the SCDs. Although RBCs supports and corticosteroids in emergencies and hydroxyurea therapy in whole lifespan decrease severity of the SCDs with some extent, the survival still shortened in both genders, dramatically. Due to the higher mortality rates, lifelong aspirin with an anti-inflammatory dose should also be used even in childhood both to decrease severity of capillary endothelial inflammation and to prevent acute thromboembolic complications in SCDs.
Keywords: Sickle cell diseases; Capillary endothelial inflammation; Capillary endothelial edema; Aspirin; Atherosclerosis; Metabolic syndrome; Aging
Introduction
Chronic endothelial damage may be the main cause of aging and death by causing end-organ insufficiencies in human being [1]. Much higher Blood Pressures (BPs) of the afferent vasculature may be the major accelerating factor by causing recurrent injuries on vascular endothelial cells. Probably, whole afferent vasculature including capillaries are mainly involved in the process. Thus the term of venosclerosis is not as famous as atherosclerosis in the literature. Due to the chronic endothelial damage, inflammation, edema, and fibrosis, vascular walls thicken, their lumens narrow, and they lose their elastic natures, those eventually reduce blood supply to the terminal organs, and increase systolic and decrease diastolic BPs further. Some of the well-known accelerating factors of the inflammatory process are physical inactivity, sedentary lifestyle, animal-rich diet, smoking, alcohol, overweight, chronic inflammations, prolonged infections, and cancers for the development of terminal consequences including obesity, Hypertension (HT), Diabetes Mellitus (DM), cirrhosis, Chronic Obstructive Pulmonary Disease (COPD), Coronary Heart Disease (CHD), Chronic Renal Disease (CRD), stroke, Peripheric Artery Disease (PAD), mesenteric ischemia, osteoporosis, dementia, early aging, and premature death [2,3]. Although early withdrawal of the accelerating factors can delay terminal consequences, after development of obesity, HT, DM, cirrhosis, COPD, CRD, CHD, stroke, PAD, mesenteric ischemia, osteoporosis, and dementia-like end-organ insufficiencies and aging, the endothelial changes can not be reversed due to their fibrotic natures, completely. The accelerating factors and terminal consequences of the vascular process are researched under the titles of metabolic syndrome, aging syndrome, and accelerated endothelial damage syndrome in the literature [4-6]. On the other hand, Sickle Cell Diseases (SCDs) are chronic inflammatory and highly destructive processes on vascular endothelium, initiated at birth and terminated with an advanced atherosclerosis induced end-organ insufficiencies in much earlier ages of life [7,8]. Hemoglobin S causes loss of elastic and biconcave disc shaped structures of Red Blood Cells (RBCs). Probably loss of elasticity instead of shape is the major problem because sickling is rare in peripheric blood samples of the cases with associated Thalassemia Minors (TMs), and human survival is not affected in hereditary spherocytosis or elliptocytosis. Loss of elasticity is present during whole lifespan, but exaggerated with inflammations, infections, and additional stresses of the body. The hardened RBCs induced chronic endothelial damage, inflammation, edema, and fibrosis terminate with tissue hypoxia all over the body [9]. As a difference from other causes of chronic endothelial damage, SCDs keep vascular endothelium particularly at the capillary level [10,11], since the capillary system is the main distributor of the hardened RBCs into the tissues. The hardened RBCs induced chronic endothelial damage builds up an advanced atherosclerosis in much earlier ages of life. Vascular narrowings and occlusions induced tissue ischemia and end-organ insufficiencies are the final consequences, so the mean life expectancy is decreased by 25 to 30 years for both genders in the SCDs [8].
Material and Methods
The study was performed in Medical Faculty of the Mustafa Kemal University between March 2007 and June 2016. All patients with the SCDs were included. The SCDs were diagnosed with the hemoglobin electrophoresis performed via High Performance Liquid Chromatography (HPLC). Medical histories including smoking, alcohol, acute painful crises per year, transfused units of RBCs in their lives, leg ulcers, stroke, surgical operations, Deep Venous Thrombosis (DVT), epilepsy, and priapism were learnt. Patients with a history of one pack-year were accepted as smokers, and one drink-year were accepted as drinkers. A complete physical examination was performed by the Same Internist, and patients with disseminated teeth losses (<20 teeth present) were detected. Patients with an acute painful crisis or any other inflammatory event were treated at first, and the laboratory tests and clinical measurements were performed on the silent phase. Check up procedures including serum iron, iron binding capacity, ferritin, creatinine, liver function tests, markers of hepatitis viruses A, B, and C, a posterior-anterior chest x-ray film, an electrocardiogram, a Doppler echocardiogram both to evaluate cardiac walls and valves, and to measure systolic BPs of pulmonary artery, an abdominal ultrasonography, a venous Doppler ultrasonography of the lower limbs, a Computed Tomography (CT) of brain, and a Magnetic Resonance İmaging (MRI) of hips were performed. Other bones for avascular necrosis were scanned according to the patients’ complaints. So avascular necrosis of bones was diagnosed by means of MRI [12]. Associated TMs were detected with serum iron, iron binding capacity, ferritin, and hemoglobin electrophoresis performed via HPLC, since the SCDs with associated TMs show a milder clinic than the sickle cell anemia (SCA) (Hb SS) alone [13]. Systolic BPs of the pulmonary artery of 40 mmHg or higher are accepted as pulmonary hypertension (PHT) [14]. The criterion for diagnosis of COPD is a post-bronchodilator forced expiratory volume in one second/forced vital capacity of lower than 70% [15]. Acute Chest Syndrome (ACS) is diagnosed clinically with the presence of new infiltrates on chest x-ray film, fever, cough, sputum production, dyspnea, or hypoxia [16]. An x-ray film of abdomen in upright position was taken just in patients with abdominal distention or discomfort, vomiting, obstipation, or lack of bowel movement, and ileus was diagnosed with gaseous distention of isolated segments of bowel, vomiting, obstipation, cramps, and with the absence of peristaltic activity. CRD is diagnosed with a persistent serum creatinine level of 1.3 mg/dL or higher in males and 1.2 mg/dL or higher in females. Cirrhosis is diagnosed with physical examination findings, laboratory parameters, and ultrasonographic evaluation. Digital clubbing is diagnosed with the ratio of distal phalangeal diameter to interphalangeal diameter of higher than 1.0, and with the presence of Schamroth’s sign [17,18]. An exercise electrocardiogram is performed in cases with an abnormal electrocardiogram and/or angina pectoris. Coronary angiography is taken for the exercise electrocardiogram positive cases. So CHD was diagnosed either angiographically or with the Doppler echocardiographic findings as movement disorders in the cardiac walls. Rheumatic heart disease is diagnosed with the echocardiographic findings, too. Stroke is diagnosed by the CT of brain. Sickle cell retinopathy is diagnosed with ophthalmologic examination in patients with visual complaints. Mann-Whitney U test, Independent-Samples t test, and comparison of proportions were used as the methods of statistical analyses.
Results
The study included 222 males and 212 females with similar ages (30.8 vs 30.3 years, p>0.05, respectively). Prevalences of associated TMs were similar in both genders, too (72.5% vs 67.9%, p>0.05, respectively). Smoking (23.8% vs 6.1%) and alcohol (4.9% vs 0.4%) were higher in males (p<0.001 for both) (Table 1). Transfused units of RBCs in their lives (48.1 vs 28.5, p=0.000), disseminated teeth losses (5.4% vs 1.4%, p<0.001), ileus (7.2% vs 1.4%, p<0.001), cirrhosis (8.1% vs 1.8%, p<0.001), leg ulcers (19.8% vs 7.0%, p<0.001), digital clubbing (14.8% vs 6.6%, p<0.001), CHD (18.0% vs 13.2%, p<0.05), CRD (9.9% vs 6.1%, p<0.05), COPD (25.2% vs 7.0%, p<0.001), and stroke (12.1% vs 7.5%, p<0.05) were all higher but not ACS (2.7% vs 3.7%), PHT (12.6% vs 11.7), DVT and/or varices and/or telangiectasias (9.0% vs 6.6%), and mean age of mortality (30.2 vs 33.3 years) in males (p>0.05 for all) (Table 2). Beside that the mean ages of terminal consequences were shown in Table 3.
Table 1: Characteristic features of the study cases.
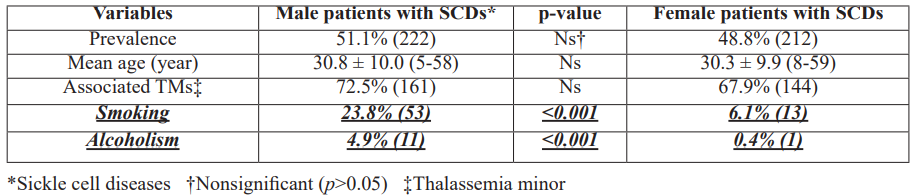
Table 2: Associated pathologies of the study cases.
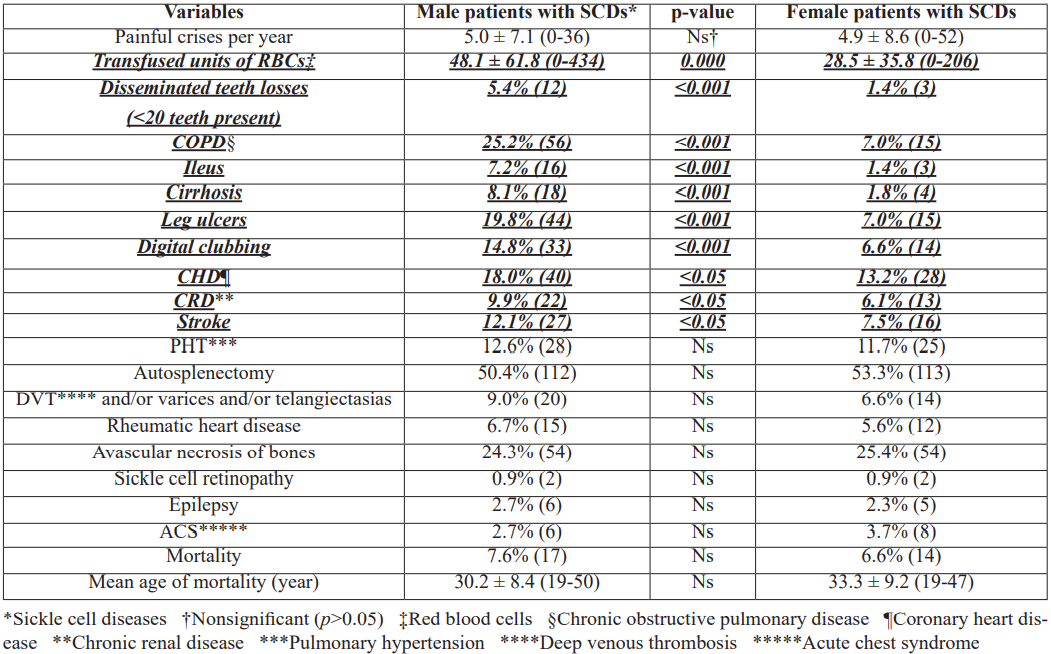
Table 3: Mean ages of the consequences of the sickle cell diseases.

Discussion
Acute painful crises are the most disabling symptoms of the SCDs. Although some authors reported that pain itself may not be life threatening, infections, medical or surgical emergencies, and emotional stress-like factors are the most common precipitating factors of the crises [19]. The increased basal metabolic rate during such additional stresses aggravates the capillary endothelial damage, inflammation, edema, tissue hypoxia, and multiorgan insufficiencies. So the risk of mortality is significantly higher during such crises. The deaths in the SCDs can not be explained by a solitary reason alone, instead they may have a multisystemic nature. Actually, each painful crisis may complicate with the following crises by leaving some sequelaes on the capillary endothelial system. After a period of time, the sequelaes may terminate with sudden end-organ insufficiencies. On the other hand, pain is the result of a complex and poorly understood interaction between RBCs, White Blood Cells (WBCs), Platelets (PLTs), and endothelial cells, yet. Whether leukocytosis contributes to the pathogenesis of the crises by releasing cytotoxic enzymes is unknown. The adverse actions of WBCs on endothelium are of particular interest with regard to the cerebrovascular diseases in the SCDs. For example, leukocytosis even in the absence of any infection was an independent predictor of the severity of the SCDs [20], and it was associated with the risk of stroke in a cohort of Jamaican patients [21]. Disseminated tissue hypoxia, releasing of inflammatory mediators, bone infarctions, and activation of afferent nerves may take role in the pathophysiology of the intolerable pain. Because of the severity of pain, narcotic analgesics are usually required to control them [22], but according to our practice, simple and repeated RBCs transfusions may be highly effective both to relieve pain and to prevent sudden death that may develop secondary to multiorgan failures on the chronic inflammatory background of the SCDs.
The deaths seem sudden and unexpected events in the SCDs. Unfortunately, most of the deaths develop just after the hospital admission, and majority of them are patients without hydroxyurea therapy [23,24]. Rapid RBCs supports are usually life-saving for such cases but preparation of RBCs units for transfusion usually takes time. Beside that RBCs supports in emergencies become much more difficult in terminal cases due to the repeated transfusions induced blood group mismatch. Actually, transfusion of each unit of RBCs complicates the following transfusions by means of the blood subgroup mismacth. Due to the significant efficacy of hydroxyurea therapy, RBCs transfusions should be kept just for acute events and emergencies in the SCDs [23,24]. According to our experiences, simple and repeated transfusions are superior to RBCs exchange in the SCDs [25,26]. First of all, preparation of one or two units of RBCs suspensions in each time rather than preparation of six units or higher provides time to clinicians to prepare more units by preventing sudden death of such high-risk patients. Secondly, transfusions of one or two units of RBCs suspensions in each time decrease the severity of pain, and relax anxiety of the patients and their relatives since RBCs transfusions probably have the strongest analgesic effects during the crises. Actually, the decreased severity of pain by transfusions also indicates the decreased severity of inflammation in whole body. Thirdly, transfusions of lesser units of RBCs suspensions in each time by means of the simple transfusions will decrease transfusion-related complications including infections, iron overload, and blood group mismatch in the future. Fourthly, transfusion of RBCs suspensions in the secondary health centers may prevent some deaths developed during the transport to the tertiary centers for the exchange. Finally, cost of the simple and repeated transfusions on insurance system is much lower than the exchange that needs trained staff and additional devices.
Hydroxyurea may be the only life-saving drug for the treatment of the SCDs. It interferes with the cell division by blocking the formation of deoxyribonucleotides by means of inhibition of ribonucleotide reductase. The deoxyribonucleotides are the building blocks of DNA. Hydroxyurea mainly affects hyperproliferating cells. Although the action way of hydroxyurea is thought to be the increase in gamma-globin synthesis for fetal hemoglobin (Hb F), its main action may be the suppression of leukocytosis and thrombocytosis by blocking the DNA synthesis in the SCDs [27,28]. By this way, the chronic inflammatory and destructive process of the SCDs is suppressed with some extent. Due to the same action way, hydroxyurea is also used in moderate and severe psoriasis to suppress hyperproliferating skin cells. As in the viral hepatitis cases, although presence of a continuous damage of sickle cells on the capillary endothelium, the severity of destructive process is probably exaggerated by the patients’ own WBCs and PLTs. So suppression of proliferation of them may limit the endothelial damage-induced edema, ischemia, and infarctions in whole body [29]. Similarly, final Hb F levels in hydroxyurea users did not differ from their pretreatment levels [30]. The Multicenter Study of Hydroxyurea (MSH) studied 299 severely affected adults with the SCA, and compared the results of patients treated with hydroxyurea or placebo [31]. The study particularly researched effects of hydroxyurea on painful crises, ACS, and requirement of blood transfusion. The outcomes were so overwhelming in the favour of hydroxyurea that the study was terminated after 22 months, and hydroxyurea was initiated for all patients. The MSH also demonstrated that patients treated with hydroxyurea had a 44% decrease in hospitalizations [31]. In multivariable analyses, there was a strong and independent association of lower neutrophil counts with the lower crisis rates [31]. But this study was performed just in severe SCA cases alone, and the rate of painful crises was decreased from 4.5 to 2.5 per year [31]. Whereas we used all subtypes of the SCDs with all clinical severity, and the rate of painful crises was decreased from 10.3 to 1.7 per year (p<0.000) with an additional decreased severity of them (7.8/10 vs 2.2/10, p<0.000) in the previous study [24]. Parallel to our results, adult patients using hydroxyurea for frequent painful crises appear to have reduced mortality rate after a 9-year follow-up period [32]. Although the underlying disease severity remains critical to determine prognosis, hydroxyurea may also decrease severity of disease and prolong survival [32]. The complications start to be seen even in infancy in the SCDs. For example, infants with lower hemoglobin values were more likely to have a higher incidence of clinical events such as ACS, painful crises, and lower neuropsychological scores, and hydroxyurea reduced the incidences of them [33]. Hydroxyurea therapy in early years of life may protect splenic function, improve growth, and prevent end-organ insufficiencies. Transfusion programmes can also reduce all of the complications, but transfusions carry many risks including infections, iron overload, and development of allo-antibodies causing subsequent transfusions difficult.
ACS is a significant cause of mortality in the SCDs [34]. It occurs most often as a single episode, and a past history is associated with a high mortality rate [34]. Similarly, all of 14 cases with ACS had just a single episode, and two of them were fatal in spite of the immediate RBCs and ventilation supports and antibiotic therapy in the present study. The remaining 12 patients are still alive without a recurrence at the end of the ten-year follow up period. ACS is the most common between two to four years of age, and its incidence decreases with aging [35]. As a difference from atherosclerotic consequences, the incidence of ACS did not show an increase with aging in the present study, and the mean ages of the cases with ACS and SCDs were similar (30.3 vs 30.5 years, p>0.05, respectively). The decreased incidence with aging may be due to the high mortality rate during the first episode and/or an acquired immunity against various antigens, and/or decreased strength of immune response by aging. Probably, ACS shows an inborn severity of the SCDs, and the incidence of ACS is higher in severe cases such as cases with SCA and higher WBCs counts [34,35]. According to our experiences, the increased metabolic rate during infections accelerates sickling, thrombocytosis, leukocytosis, and capillary endothelial damage and edema, and terminates with end-organ insufficiencies. ACS may also be a collapse of the pulmonary vasculature during such infections, and the exaggerated immune response against the abnormal RBCs-induced diffuse capillary endothelial damage may be important in the high mortality rate. A preliminary result from the Multi-Institutional Study of Hydroxyurea in the SCDs indicating a significant reduction of episodes of ACS with hydroxyurea therapy suggests that a considerable number of episodes are exaggerated with the increased numbers of WBCs and PLTs [36]. Similarly, we strongly recommend hydroxyurea therapy for all patients with the SCDs that may also be the cause of the low incidence of ACS among our follow up cases (2.7% in males and 3.7% in females). Additionally, ACS did not show an infectious etiology in 66% of cases (34, 35), and 12 of 27 cases with ACS had evidence of fat embolism in the other study [37]. Beside that some authors indicated that antibiotics do not shorten the clinical course [38]. RBCs support must be given early in the course of ACS. RBCs support has the obvious benefits of decreasing sickle cell concentration directly, and suppressing bone marrow for the production of abnormal RBCs and excessive WBCs and PLTs. So they prevent further sickling, capillary endothelial damage, exaggerated capillary endothelial inflammation and edema, tissue hypoxia, and end-organ insufficiencies in whole body.
PHT is a condition of increased BPs within the arteries of the lungs. Shortness of breath, fatigue, chest pain, palpitation, swelling of legs and ankles, and cyanosis are common symptoms of PHT. Actually, it is not a diagnosis itself, instead solely a hemodynamic state characterized by resting mean pulmonary artery pressure of 25 mmHg or higher. An increase in pulmonary artery systolic pressure, estimated noninvasively by the echocardiography, helps to identify patients with PHT [39]. The cause is often unknown. The underlying mechanism typically involves inflammation, fibrosis, and subsequent remodelling of the arteries. According to World Health Organization, there are five groups of PHT including pulmonary arterial hypertension, PHT secondary to left heart diseases, PHT secondary to lung diseases, chronic thromboembolic PHT, and PHT with unknown mechanisms [40]. PHT affects about 1% of the world population, and its prevalence may reach 10% above the age of 65 years [41]. Onset is typically seen between 20 and 60 years of age [40]. The most common causes are CHD and COPD [40,42]. The cause of PHT in COPD is generally assumed to be hypoxic pulmonary vasoconstriction leading to permanent medial hypertrophy [43]. But the pulmonary vascular remodeling in the COPD may have a much more complex mechanism than just being the medial hypertrophy secondary to the long-lasting hypoxic vasoconstriction alone [43]. In fact, all layers of the vessel wall appear to be involved with prominent intimal changes [43]. The specific pathological picture could be explained by the combined effects of hypoxia, prolonged stretching of hyperinflated lungs-induced mechanical stress and inflammatory reaction, and the toxic effects of cigarette smoke [43]. On the other hand, PHT is also a common consequence of the SCDs [44], and its prevalence was detected between 20% and 40% in the SCDs [45]. Whereas we detected the ratio as 12.2% in the present study. Although the higher prevalences of smoking, alcohol, disseminated teeth losses, ileus, cirrhosis, leg ulcers, digital clubbing, CRD, COPD, and stroke-like atherosclerotic risk factors or consequences in male gender, and the male gender alone is a risk factor for the systemic atherosclerosis, the similar prevalences of PHT and ACS in both genders also support nonatherosclerotic natures of PHT and ACS in SCDs in the present study. Additionally, frequencies of DVT and/or varices and/or telangiectasias were similar in males and females parallel to ACS and PHT (9.0% vs 6.6%, p>0.05, respectively). Similarly, CHD is the other most common cause of PHT in the society [46], and although the higher prevalence of CHD in males in the present study (18.0% vs 13.2%, p<0.05), PHT was not higher in males, again. In another definition, PHT may have a hardened RBCs-induced chronic thromboembolic whereas ACS may have an acute thromboembolic backgrounds in the SCDs [47,48], since the mean age of ACS is lower than PHT (30.3 and 34.0 years, p<0.05), and its mortality is much higher than PHT [34,35,40].
COPD is the third leading cause of death with various underlying etiologies in whole world [49,50]. Aging, physical inactivity, sedentary lifestyle, animal-rich diet, smoking, alcohol, male gender, excess weight, chronic inflammations, prolonged infections, and cancers may be the major underlying causes. Beside smoking, regular alcohol consumption is also important for the pulmonary and systemic inflammatory process of the COPD, since COPD was one of the most common diagnoses in alcohol dependence [51]. Furthermore, 30-day readmission rates were higher in the COPD patients with alcoholism [52]. Probably an accelerated atherosclerotic process is the main structural background of functional changes that are characteristics of the COPD. The inflammatory process of vascular endothelium is enhanced by release of various chemicals by inflammatory cells, and it terminates with an advanced fibrosis, atherosclerosis, and pulmonary losses. COPD may actually be the pulmonary consequence of the systemic atherosclerotic process. Since beside the accelerated atherosclerotic process of the pulmonary vasculature, there are several reports about coexistence of associated endothelial inflammation all over the body in COPD [53,54]. For example, there may be close relationships between COPD, CHD, PAD, and stroke [55]. Furthermore, two-third of mortality cases were caused by cardiovascular diseases and lung cancers in the COPD, and the CHD was the most common cause in a multi-center study of 5.887 smokers [56]. When the hospitalizations were researched, the most common causes were the cardiovascular diseases, again [56]. In another study, 27% of mortality cases were due to the cardiovascular diseases in the moderate and severe COPD [57]. On the other hand, COPD may be the pulmonary consequence of the systemic atherosclerotic process caused by the hardened RBCs in the SCDs [49].
Digital clubbing is characterized by the increased normal angle of 165° between nailbed and fold, increased convexity of the nail fold, and thickening of the whole distal finger [58]. Although the exact cause and significance is unknown, the chronic tissue hypoxia is highly suspected [59]. In the previous study, only 40% of clubbing cases turned out to have significant underlying diseases while 60% remained well over the subsequent years [18]. But according to our experiences, digital clubbing is frequently associated with the pulmonary, cardiac, renal, and hepatic diseases and smoking which are characterized with chronic tissue hypoxia [5]. As an explanation for that hypothesis, lungs, heart, kidneys, and liver are closely related organs which affect their functions in a short period of time. On the other hand, digital clubbing is also common in the SCDs, and its prevalence was 10.8% in the present study. It probably shows chronic tissue hypoxia caused by disseminated endothelial damage, inflammation, edema, and fibrosis at the capillary level in the SCDs. Beside the effects of SCDs, smoking, alcohol, cirrhosis, CRD, CHD, and COPD, the higher prevalence of digital clubbing in males (14.8% vs 6.6%, p<0.001) may also show some additional role of male gender in the systemic atherosclerotic process.
Leg ulcers are seen in 10% to 20% of the SCDs, and the ratio was 13.5% in the present study [60]. Its prevalence increases with aging, male gender, and SCA [61]. Similarly, its ratio was higher in males (19.8% vs 7.0%, p<0.001), and mean age of the leg ulcer cases was higher than the remaining patients (35.3 vs 29.8 years, p<0.000) in the present study. The leg ulcers have an intractable nature, and around 97% of them relapse in a period of one year [60]. As an evidence of their atherosclerotic nature, the leg ulcers occur in the distal segments of the body with a lesser collateral blood flow [60]. The hardened RBCs induced chronic endothelial damage, inflammation, edema, and fibrosis at the capillary level may be the major causes, again [61]. Prolonged exposure to the hardened bodies due to the pooling of blood in the lower extremities may also explain the leg but not arm ulcers in the SCDs. The hardened RBCs induced venous insufficiencies may also accelerate the process by pooling of causative bodies in the legs, and vice versa. Pooling of blood may also have some effects on development of venous ulcers, diabetic ulcers, Buerger’s disease, digital clubbing, and onychomycosis in the lower extremities. Furthermore, probably pooling of blood is the cause of delayed wound and fracture healings in the lower extremities. Smoking and alcohol may also have some additional atherosclerotic effects on the ulcers in males. Hydroxyurea is the first drug that was approved by Food and Drug Administration in the SCDs [62]. It is an orally-administered, cheap, safe, and effective drug that blocks cell division by suppressing formation of deoxyribonucleotides which are the building blocks of DNA [11]. Its main action may be the suppression of hyperproliferative WBCs and PLTs in the SCDs [63]. Although presence of a continuous damage of hardened RBCs on vascular endothelium, severity of the destructive process is probably exaggerated by the patients’ own immune systems. Similarly, lower WBCs counts were associated with lower crises rates, and if a tissue infarct occurs, lower WBCs counts may decrease severity of pain and tissue damage [30]. According to our experiences, prolonged resolution of leg ulcers with hydroxyurea may also suggest that the ulcers may be secondary to increased WBCs and PLTs counts induced exaggerated capillary endothelial inflammation and edema instead of the fibrosis, yet.
Cirrhosis was the 10th leading cause of death for men and the 12th for women in the United States in 2001 [6]. Although the improvements of health services worldwide, the increased morbidity and mortality of cirrhosis may be explained by prolonged survival of the human being, and increased prevalence of excess weight all over the world. For example, Nonalcoholic Fatty Liver Disease (NAFLD) affects up to one third of the world population, and it became the most common cause of chronic liver disease even at childhood, nowadays [64]. NAFLD is a marker of pathological fat deposition combined with a low-grade inflammation which results with hypercoagulability, endothelial dysfunction, and an accelerated atherosclerosis [64]. Beside terminating with cirrhosis, NAFLD is associated with higher overall mortality rates as well as increased prevalences of cardiovascular diseases [65]. Authors reported independent associations between NAFLD and impaired flow-mediated vasodilation and increased mean Carotid artery İntima-Media Thickness (CIMT) [66]. NAFLD may be considered as one of the hepatic consequences of the metabolic syndrome and SCDs [67]. Probably smoking also takes role in the inflammatory process of the capillary endothelium in liver, since the systemic inflammatory effects of smoking on endothelial cells is well-known with Buerger’s disease and COPD [68]. Increased oxidative stresses, inactivation of antiproteases, and release of proinflammatory mediators may terminate with the systemic atherosclerosis in smokers. The atherosclerotic effects of alcohol is much more prominent in hepatic endothelium probably due to the highest concentrations of its metabolites there. Chronic infectious or inflammatory processes and cancers may also terminate with an accelerated atherosclerosis in whole body [69]. For example, chronic Hepatitis C Virus (HCV) infection raised CIMT, and normalization of hepatic function with HCV clearance may be secondary to reversal of favourable lipids observed with the chronic infection [69,70]. As a result, cirrhosis may also be another atherosclerotic consequence of the SCDs.
The increased frequency of CRD can also be explained by aging of the human being, and increased prevalence of excess weight all over the world [71,72]. Aging, physical inactivity, sedentary lifestyle, animal-rich diet, excess weight, smoking, alcohol, inflammatory or infectious processes, and cancers may be the major causes of the renal endothelial inflammation. The inflammatory process is enhanced by release of various chemicals by lymphocytes to repair the damaged endothelial cells of the renal arteriols. Due to the continuous irritation of the vascular endothelial cells, prominent changes develop in the architecture of the renal tissues with advanced atherosclerosis, tissue hypoxia, and infarcts. Excess weight induced hyperglycemia, dyslipidemia, elevated BPs, and insulin resistance may cause tissue inflammation and immune cell activation [73]. For example, age (p= 0.04), high-sensitivity C-reactive protein (p= 0.01), mean arterial BPs (p= 0.003), and DM (p= 0.02) had significant correlations with the CIMT [72]. Increased renal tubular sodium reabsorption, impaired pressure natriuresis, volume expansion due to the activations of sympathetic nervous system and renin-angiotensin system, and physical compression of kidneys by visceral fat tissue may be some mechanisms of the increased BPs with excess weight [74]. Excess weight also causes renal vasodilation and glomerular hyperfiltration which initially serve as compensatory mechanisms to maintain sodium balance due to the increased tubular reabsorption [74]. However, along with the increased BPs, these changes cause a hemodynamic burden on the kidneys in long term that causes chronic endothelial damage [75]. With prolonged weight excess, there are increased urinary protein excretion, loss of nephron function, and exacerbated HT. With the development of dyslipidemia and DM in cases with excess weight, CRD progresses much more easily [74]. On the other hand, the systemic inflammatory effects of smoking on endothelial cells may also be important in the CRD [76]. Although some authors reported that alcohol was not related with the CRD [76], various metabolites of alcohol circulate even in the blood vessels of the kidneys and give harm to the renal vascular endothelium. Chronic inflammatory or infectious processes may also terminate with the accelerated atherosclerosis in the renal vasculature [69]. Although CRD is due to the atherosclerotic process of the renal vasculature, there are close relationships between CRD and other atherosclerotic consequences of the metabolic syndrome including CHD, COPD, PAD, cirrhosis, and stroke [77]. For example, the most common cause of death was the cardiovascular diseases in the CRD again [78]. The hardened RBCs-induced capillary endothelial damage in the renal vasculature may be the main cause of CRD in the SCDs. In another definition, CRD may just be one of the several atherosclerotic consequences of the metabolic syndrome and SCDs, again [79].
Stroke is an important cause of death, and develops as an acute thromboembolic event on the chronic atherosclerotic background in most of the cases. Aging, male gender, smoking, alcohol, and excess weight may be the major underlying causes. Stroke is also a common complication of the SCDs [80,81]. Similar to the leg ulcers, stroke is particularly higher in the SCA and cases with higher WBCs counts [82]. Sickling induced capillary endothelial damage, activations of WBCs, PLTs, and coagulation system, and hemolysis may terminate with chronic capillary endothelial inflammation, edema, and fibrosis [83]. Probably, stroke may not have a macrovascular origin in the SCDs, and diffuse capillary endothelial inflammation, edema, and fibrosis may be much more important. Infections, inflammations, medical or surgical emergencies, and emotional stresses may precipitate stroke by increasing basal metabolic rate and sickling. A significant reduction of stroke with hydroxyurea may also suggest that a significant proportion of cases is developed due to the increased WBCs and PLTs counts-induced exaggerated capillary inflammation, edema, and fibrosis [36].
The venous endothelium is also involved in the SCDs [84]. Normally, leg muscles pump veins against the gravity, and the veins have pairs of leaflets of valves to prevent blood from flowing backwards. When the leaflets are damaged, varices and/or telangiectasias develop. DVT may also cause varicose veins. Varicose veins are the most common in superficial veins of the legs, which are subject to higher pressure when standing up, therefore physical examination must be performed in upright position. Although the relatively younger mean ages of the patients and significantly lower body mass index of the SCDs patients in the literature [10], the prevalences of DVT and/or varices and/or telangiectasias of the lower limbs were relatively higher in the present study (9.0% vs 6.6% in males and females, p>0.05, respectively), indicating an additional venous involvement of the SCDs. Similarly, priapism is the painful erection of penis that can not return to its flaccid state within four hours in the absence of any stimulation [85]. It is an emergency since repeated damaging of the blood vessels may terminate with fibrosis of the corpus cavernosa, a consecutive erectile dysfunction, and eventually a shortened, indurated, and non-erectile penis [85]. It is mainly seen with SCDs, spinal cord lesions (hanging victims), and glucose-6-phosphate dehydrogenase deficiency [86,87]. Ischemic (veno-occlusive), stuttering (recurrent ischemic), and nonischemic priapisms (arterial) are the three types [88]. Ninety-five percent of clinically presented priapisms are the ischemic (veno-occlusive) disorders in which blood can not return adequately from the penis as in the SCDs, and they are very painful [85,88]. The other 5% are nonischemic (arterial) type usually caused by a blunt perineal trauma in which there is a short circuit of the vascular system [85]. Treatment of arterial type is not as urgent as the veno-occlusive type due to the absence of risk of ischemia [85]. RBCs support is the treatment of choice in acute phase whereas hydroxyurea should be the treatment of choice in chronic phase [89]. According to our experiences, hydroxyurea is effective for prevention of attacks and consequences of priapism if iniatiated in early years of life, but it may be difficult due to the excessive fibrosis around the capillary walls if initiated later in life.
Aspirin is a Nonsteroidal Anti-İnflammatory Drug (NSAID) used to reduce pain, fever, inflammation, and acute thromboembolic events. Although aspirin has similar anti-inflammatory effects with the other NSAIDs, it also suppresses the normal functions of PLTs, irreversibly. This property causes aspirin being different from other NSAIDs, which are reversible inhibitors. Aspirin acts as an acetylating agent where an acetyl group is covalently attached to a serine residue in the active site of the Cyclooxygenase (COX) enzyme. Aspirin’s ability to suppress the production of Prostaglandins (PGs) and Thromboxanes (TXs) is due to its irreversible inactivation of the COX enzyme required for PG and TX synthesis. PGs are the locally produced hormones with some diverse effects, including the transmission of pain into the brain and modulation of the hypothalamic thermostat and inflammation in the body. TXs are responsible for the aggregation of PLTs to form blood clots. In another definition, low-dose aspirin use irreversibly blocks the formation of TXA2 in the PLTs, producing an inhibitory effect on the PLT aggregation during whole lifespan of the affected PLTs (8-9 days). Since PLTs do not have nucleus and DNA, they are unable to synthesize new COX enzyme once aspirin has inhibited the enzyme. The antithrombotic property of aspirin is useful to reduce the incidences of myocardial infarction, transient ischemic attack, and stroke [90]. Heart attacks are caused primarily by blood clots, and low dose of aspirin is seen as an effective medical intervention to prevent a second myocardial infarction [91]. According to the literature, aspirin may also be effective in prevention of colorectal cancers [92]. On the other hand, aspirin has some side effects including gastric ulcers, gastric bleeding, worsening of asthma, and Reye syndrome in childhood and adolescence. Due to the risk of Reye syndrome, the US Food and Drug Administration recommends that aspirin or aspirin-containing products should not be prescribed for febrile patients under the age of 12 years [93]. Eventually, the general recommendation to use aspirin in children has been withdrawn, and it was only recommended for Kawasaki disease [94]. Reye syndrome is a rapidly worsening brain disease [94]. The first detailed description of Reye syndrome was in 1963 by an Australian pathologist, Douglas Reye [95]. The syndrome mostly affects children, but it can only affect fewer than one in a million children a year [95]. Symptoms of Reye syndrome may include personality changes, confusion, seizures, and loss of consciousness [94]. Although the liver toxicity typically occurs in the syndrome, jaundice is usually not seen with it, but the liver is enlarged in most cases [94]. Although the death occurs in 20-40% of affected cases, about one third of survivors get a significant degree of brain damage [94]. The cause of Reye syndrome is unknown [95]. It usually starts just after recovery from a viral infection, such as influenza or chicken pox. About 90% of cases in children are associated with an aspirin use [95,96]. Inborn errors of metabolism are also the other risk factors, and the genetic testing for inborn errors of metabolism became available in developed countries in the 1980s [94]. When aspirin use was withdrawn for children in the US and UK in the 1980s, a decrease of more than 90% in rates of Reye syndrome was seen [95]. Early diagnosis improves outcomes, and treatment is supportive. Mannitol may be used in cases with the brain swelling [95]. Due to the very low risk of Reye syndrome but much higher risk of death due to the SCDs in children, aspirin should be added both into the acute and chronic phase treatments with an anti-inflammatory dose even in childhood in the SCDs [97].
Conclusion
The hardened RBCs-induced capillary endothelial damage, inflammation, edema, and fibrosis are initiated at birth, and terminate with diffuse tissue hypoxia and multiorgan insufficiencies even at childhood in the SCDs. Although RBCs supports and corticosteroids in emergencies and hydroxyurea therapy in whole lifespan decrease severity of the SCDs with some extent, the survival still shortened in both genders, dramatically. Due to the much higher mortality rates, lifelong aspirin with an anti-inflammatory dose should also be used even in childhood both to decrease severity of capillary endothelial inflammation and to prevent acute thromboembolic complications in the SCDs.
References
- Widlansky ME, Gokce N, Keaney JF Jr, Vita JA. The clinical implications of endothelial dysfunction. J Am Coll Cardiol, 2003; 42(7): 1149-1160.
- Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet, 2005; 365(9468): 1415-1428.
- Franklin SS, Barboza MG, Pio JR, Wong ND. Blood pressure categories, hypertensive subtypes, and the metabolic syndrome. J Hypertens, 2006; 24(10): 2009-2016.
- Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation, 2002; 106(25): 3143-3421.
- Helvaci MR, Aydin LY, Aydin Y. Digital clubbing may be an indicator of systemic atherosclerosis even at microvascular level. HealthMED, 2012; 6(12): 3977-3981.
- Anderson RN, Smith BL. Deaths: leading causes for 2001. Natl Vital Stat Rep, 2003; 52(9): 1-85.
- Helvaci MR, Gokce C, Davran R, Akkucuk S, Ugur M, Oruc C. Mortal quintet of sickle cell diseases. Int J Clin Exp Med, 2015; 8(7): 11442-1144
- Platt OS, Brambilla DJ, Rosse WF, Milner PF, Castro O, Steinberg MH, et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N Engl J Med, 1994; 330(23): 1639-1644.
- Helvaci MR, Yaprak M, Abyad A, Pocock L. Atherosclerotic background of hepatosteatosis in sickle cell diseases. World Family Med, 2018; 16(3): 12-1
- Helvaci MR, Kaya H. Effect of sickle cell diseases on height and weight. Pak J Med Sci, 2011; 27(2): 361-364.
- Helvaci MR, Aydin Y, Ayyildiz O. Hydroxyurea may prolong survival of sickle cell patients by decreasing frequency of painful crises. HealthMED, 2013; 7(8): 2327-23
- Mankad VN, Williams JP, Harpen MD, Manci E, Longenecker G, Moore RB, et al. Magnetic resonance imaging of bone marrow in sickle cell disease: clinical, hematologic, and pathologic correlations. Blood, 1990; 75(1): 274-283.
- Helvaci MR, Aydin Y, Ayyildiz O. Clinical severity of sickle cell anemia alone and sickle cell diseases with thalassemias. HealthMED, 2013; 7(7): 2028-2033.
- Fisher MR, Forfia PR, Chamera E, Housten-Harris T, Champion HC, Girgis RE, et al. Accuracy of Doppler echocardiography in the hemodynamic assessment of pulmonary hypertension. Am J Respir Crit Care Med, 2009; 179(7): 615-621.
- Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med,2013; 187(4): 347-3
- Davies SC, Luce PJ, Win AA, Riordan JF, Brozovic M. Acute chest syndrome in sickle-cell disease. Lancet, 1984; 1(8367): 36-38.
- Vandemergel X, Renneboog B. Prevalence, aetiologies and significance of clubbing in a department of general internal medicine. Eur J Intern Med, 2008; 19(5): 325-329.
- Schamroth L. Personal experience. S Afr Med J, 1976; 50(9): 297-300.
- Parfrey NA, Moore W, Hutchins GM. Is pain crisis a cause of death in sickle cell disease? Am J Clin Pathol, 1985; 84: 209-212.
- Miller ST, Sleeper LA, Pegelow CH, Enos LE, Wang WC, Weiner SJ, et al. Prediction of adverse outcomes in children with sickle cell disease. N Engl J Med, 2000; 342: 83-89.
- Balkaran B, Char G, Morris JS, Thomas PW, Serjeant BE, Serjeant GR. Stroke in a cohort of patients with homozygous sickle cell disease. J Pediatr, 1992; 120: 360-36
- Cole TB, Sprinkle RH, Smith SJ, Buchanan GR. Intravenous narcotic therapy for children with severe sickle cell pain crisis. Am J Dis Child, 1986; 140: 1255-125
- Helvaci MR, Ayyildiz O, Gundogdu M. Hydroxyurea therapy and parameters of health in sickle cell patients. HealthMED, 2014; 8(4): 451-45
- Helvaci MR, Tonyali O, Yaprak M, Abyad A, Pocock L. Increased sexual performance of sickle cell patients with hydroxyurea. World Family Med, 2019; 17(4): 28-
- Helvaci MR, Atci N, Ayyildiz O, Muftuoglu OE, Pocock L. Red blood cell supports in severe clinical conditions in sickle cell diseases. World Family Med, 2016; 14(5): 11-18.
- Helvaci MR, Ayyildiz O, Gundogdu M. Red blood cell transfusions and survival of sickle cell patients. HealthMED, 2013; 7(11): 2907-2912.
- Miller BA, Platt O, Hope S, Dover G, Nathan DG. Influence of hydroxyurea on fetal hemoglobin production in vitro. Blood, 1987; 70(6): 1824-182
- Platt OS. Is there treatment for sickle cell anemia? N Engl J Med, 1988; 319(22): 1479-14
- Helvaci MR, Aydogan F, Sevinc A, Camci C, Dilek I. Platelet and white blood cell counts in severity of sickle cell diseases. Pren Med Argent, 2014; 100(1): 49-56.
- Charache S. Mechanism of action of hydroxyurea in the management of sickle cell anemia in adults. Semin Hematol, 1997; 34(3): 15-21.
- Charache S, Barton FB, Moore RD, Terrin ML, Steinberg MH, Dover GJ, et al. Hydroxyurea and sickle cell anemia. Clinical utility of a myelosuppressive "switching" agent. The Multicenter Study of Hydroxyurea in Sickle Cell Anemia. Medicine (Baltimore), 1996; 75(6): 300-3
- Steinberg MH, Barton F, Castro O, Pegelow CH, Ballas SK, Kutlar A, et al. Effect of hydroxyurea on mortality and morbidity in adult sickle cell anemia: risks and benefits up to 9 years of treatment. JAMA, 2003; 289(13): 1645-16
- Lebensburger JD, Miller ST, Howard TH, Casella JF, Brown RC, Lu M, et al. BABY HUG Investigators. Influence of severity of anemia on clinical findings in infants with sickle cell anemia: analyses from the BABY HUG study. Pediatr Blood Cancer, 2012; 59(4): 675-67
- Poncz M, Kane E, Gill FM. Acute chest syndrome in sickle cell disease: etiology and clinical correlates. J Pediatr, 1985; 107(6): 861-866.
- Sprinkle RH, Cole T, Smith S, Buchanan GR. Acute chest syndrome in children with sickle cell disease. A retrospective analysis of 100 hospitalized cases. Am J Pediatr Hematol Oncol, 1986; 8(2): 105-110.
- Charache S, Terrin ML, Moore RD, Dover GJ, Barton FB, Eckert SV, et al. Effect of hydroxyurea on the frequency of painful crises in sickle cell anemia. Investigators of the Multicenter Study of Hydroxyurea in Sickle Cell Anemia. N Engl J Med, 1995; 332(20): 1317-1322.
- Vichinsky E, Williams R, Das M, Earles AN, Lewis N, Adler A, et al. Pulmonary fat embolism: a distinct cause of severe acute chest syndrome in sickle cell anemia. Blood, 1994; 83(11): 3107-3112.
- Charache S, Scott JC, Charache P. ‘‘Acute chest syndrome’’ in adults with sickle cell anemia. Microbiology, treatment, and prevention. Arch Intern Med, 1979; 139(1): 67-69.
- Gordeuk VR, Castro OL, Machado RF. Pathophysiology and treatment of pulmonary hypertension in sickle cell disease. Blood, 2016; 127(7): 820-828.
- Simonneau G, Gatzoulis MA, Adantia I, Celermajer D, Denton C, Ghofrani A, et al. Updated clinical classification of pulmonary hypertension. J American College Cardiol, 2013; 62(25): 34-41.
- Hoeper MM, Humbert M, Souza R, Idrees M, Kawut SM, Sliwa-Hahnle K, et al. A global view of pulmonary hypertension. Lancet Respir Med, 2016; 4(4): 306-322.
- Naeije R, Barbera JA. Pulmonary hypertension associated with COPD. Crit Care, 2001; 5(6): 286-289.
- Peinado VI, Barbera JA, Abate P, Ramirez J, Roca J, Santos S, et al. Inflammatory reaction in pulmonary muscular arteries of patients with mild chronic obstructive pulmonary disease. Am J Respir Crit Care Med, 1999; 59: 1605-1611.
- Helvaci MR, Arslanoglu Z, Celikel A, Abyad A, Pocock L. Pathophysiology of pulmonary hypertension in sickle cell diseases. Middle East J Intern Med, 2018; 11(2): 14-
- Castro O. Systemic fat embolism and pulmonary hypertension in sickle cell disease. Hematol Oncol Clin North Am, 1996; 10(6): 1289-1303.
- Duffels MG, Engelfriet PM, Berger RM, van Loon RL, Hoendermis E, Vriend JW, et al. Pulmonary arterial hypertension in congenital heart disease: an epidemiologic perspective from a Dutch registry. Int J Cardiol, 2007; 120(2): 198-204.
- Oudiz RJ. Classification of pulmonary hypertension. Cardiol Clin, 2016; 34(3): 359-361.
- Gladwin MT, Sachdev V, Jison ML, Shizukuda Y, Plehn JF, Minter K, et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med, 2004; 350(9): 886-895.
- Helvaci MR, Erden ES, Aydin LY. Atherosclerotic background of chronic obstructive pulmonary disease in sickle cell patients. HealthMED 2013; 7(2): 484-488.
- Rennard SI, Drummond MB. Early chronic obstructive pulmonary disease: definition, assessment, and prevention. Lancet, 2015; 385(9979): 1778-1788.
- Schoepf D, Heun R. Alcohol dependence and physical comorbidity: Increased prevalence but reduced relevance of individual comorbidities for hospital-based mortality during a 12.5-year observation period in general hospital admissions in urban North-West England. Eur Psychiatry, 2015; 30(4): 459-468.
- Singh G, Zhang W, Kuo YF, Sharma G. Association of Psychological Disorders With 30-Day Readmission Rates in Patients With COPD. Chest, 2016; 149(4): 905-915.
- Danesh J, Collins R, Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease: meta-analyses of prospective studies. JAMA, 1998; 279(18): 1477-1482.
- Mannino DM, Watt G, Hole D, Gillis C, Hart C, McConnachie A, et al. The natural history of chronic obstructive pulmonary disease. Eur Respir J, 2006; 27(3): 627-643.
- Mapel DW, Hurley JS, Frost FJ, Petersen HV, Picchi MA, Coultas DB. Health care utilization in chronic obstructive pulmonary disease. A case-control study in a health maintenance organization. Arch Intern Med, 2000; 160(17): 2653-2658.
- Anthonisen NR, Connett JE, Enright PL, Manfreda J. Lung Health Study Research Group. Hospitalizations and mortality in the Lung Health Study. Am J Respir Crit Care Med, 2002; 166(3): 333-339.
- McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA. TORCH Clinical Endpoint Committee. Ascertainment of cause-specific mortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax, 2007; 62(5): 411-415.
- Myers KA, Farquhar DR. The rational clinical examination. Does this patient have clubbing? JAMA, 2001; 286(3): 341-347.
- Toovey OT, Eisenhauer HJ. A new hypothesis on the mechanism of digital clubbing secondary to pulmonary Med Hypotheses, 2010; 75(6): 511-513.
- Trent JT, Kirsner RS. Leg ulcers in sickle cell disease. Adv Skin Wound Care, 2004: 17(8); 410-41
- Minniti CP, Eckman J, Sebastiani P, Steinberg MH, Ballas SK. Leg ulcers in sickle cell disease. Am J Hematol, 2010; 85(10): 831-83
- Yawn BPs, Buchanan GR, Afenyi-Annan AN, Ballas SK, Hassell KL, James AH, et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. JAMA, 2014; 312(10): 1033-10
- Helvaci MR, Aydogan F, Sevinc A, Camci C, Dilek I. Platelet and white blood cell counts in severity of sickle cell diseases. HealthMED, 2014; 8(4): 477-4
- Bhatia LS, Curzen NP, Calder PC, Byrne CD. Non-alcoholic fatty liver disease: a new and important cardiovascular risk factor? Eur Heart J, 2012; 33(10): 1190-1200.
- Pacifico L, Nobili V, Anania C, Verdecchia P, Chiesa C. Pediatric nonalcoholic fatty liver disease, metabolic syndrome and cardiovascular risk. World J Gastroenterol, 2011; 17(26): 3082-3091.
- Mawatari S, Uto H, Tsubouchi H. Chronic liver disease and arteriosclerosis. Nihon Rinsho, 2011; 69(1): 153-157.
- Bugianesi E, Moscatiello S, Ciaravella MF, Marchesini G. Insulin resistance in nonalcoholic fatty liver disease. Curr Pharm Des, 2010; 16(17): 1941-1951.
- Helvaci MR, Aydin LY, Aydin Y. Chronic obstructive pulmonary disease may be one of the terminal end points of metabolic syndrome. Pak J Med Sci, 2012; 28(3): 376-379.
- Mostafa A, Mohamed MK, Saeed M, Hasan A, Fontanet A, Godsland I, et al. Hepatitis C infection and clearance: impact on atherosclerosis and cardiometabolic risk factors. Gut, 2010; 59(8): 1135-11
- Helvaci MR, Ayyildiz O, Gundogdu M, Aydin Y, Abyad A, Pocock L. Hyperlipoproteinemias may actually be acute phase reactants in the plasma. World Family Med, 2018; 16(1): 7-10.
- Levin A, Hemmelgarn B, Culleton B, Tobe S, McFarlane P, Ruzicka M, et al. Guidelines for the management of chronic kidney disease. CMAJ, 2008; 179(11): 1154-11
- Nassiri AA, Hakemi MS, Asadzadeh R, Faizei AM, Alatab S, Miri R, et al. Differences in cardiovascular disease risk factors associated with maximum and mean carotid intima-media thickness among hemodialysis patients. Iran J Kidney Dis, 2012; 6(3): 203-20
- Xia M, Guerra N, Sukhova GK, Yang K, Miller CK, Shi GP, et al. Immune activation resulting from NKG2D/ligand interaction promotes atherosclerosis. Circulation, 2011; 124(25): 2933-2943.
- Hall JE, Henegar JR, Dwyer TM, Liu J, da Silva AA, Kuo JJ, et al. Is obesity a major cause of chronic kidney disease? Adv Ren Replace Ther, 2004; 11(1): 41-
- Nerpin E, Ingelsson E, Risérus U, Helmersson-Karlqvist J, Sundström J, Jobs E, et al. Association between glomerular filtration rate and endothelial function in an elderly community cohort. Atherosclerosis, 2012; 224(1): 242-246.
- Stengel B, Tarver-Carr ME, Powe NR, Eberhardt MS, Brancati FL. Lifestyle factors, obesity and the risk of chronic kidney disease. Epidemiology, 2003; 14(4): 479-4
- Bonora E, Targher G. Increased risk of cardiovascular disease and chronic kidney disease in NAFLD. Nat Rev Gastroenterol Hepatol, 2012; 9(7): 372-381.
- Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, et al. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol, 2006; 17(7): 2034-20
- Helvaci MR, Aydin Y, Aydin LY. Atherosclerotic background of chronic kidney disease in sickle cell patients. HealthMED, 2013; 7(9): 2532-253
- DeBaun MR, Gordon M, McKinstry RC, Noetzel MJ, White DA, Sarnaik SA, et al. Controlled trial of transfusions for silent cerebral infarcts in sickle cell anemia. N Engl J Med, 2014; 371(8): 699-
- Gueguen A, Mahevas M, Nzouakou R, Hosseini H, Habibi A, Bachir D, et al. Sickle-cell disease stroke throughout life: a retrospective study in an adult referral center. Am J Hematol, 2014; 89(3): 267-2
- Majumdar S, Miller M, Khan M, Gordon C, Forsythe A, Smith MG, et al. Outcome of overt stroke in sickle cell anaemia, a single institution's experience. Br J Haematol, 2014; 165(5): 707-7
- Kossorotoff M, Grevent D, de Montalembert M. Cerebral vasculopathy in pediatric sickle-cell anemia. Arch Pediatr, 2014; 21(4): 404-4
- Helvaci MR, Gokce C, Sahan M, Hakimoglu S, Coskun M, Gozukara KH. Venous involvement in sickle cell diseases. Int J Clin Exp Med 2016; 9(6): 11950-11957.
- Kaminsky A, Sperling H. Diagnosis and management of priapism. Urologe A, 2015; 54(5): 654-661.
- Anele UA, Le BV, Resar LM, Burnett AL. How I treat priapism. Blood, 2015; 125(23): 3551-3558.
- Bartolucci P, Lionnet F. Chronic complications of sickle cell disease. Rev Prat, 2014; 64(8): 1120-1126.
- Broderick GA. Priapism and sickle-cell anemia: diagnosis and nonsurgical therapy. J Sex Med, 2012; 9(1): 88-103.
- Ballas SK, Lyon D. Safety and efficacy of blood exchange transfusion for priapism complicating sickle cell disease. J Clin Apher, 2016; 31(1): 5-10.
- Toghi H, Konno S, Tamura K, Kimura B, Kawano K. Effects of low-to-high doses of aspirin on platelet aggregability and metabolites of thromboxane A2 and prostacyclin. Stroke, 1992; 23(10): 1400-1403.
- Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, et al. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet, 2009; 373(9678): 1849-1860.
- Algra AM, Rothwell PM. Effects of regular aspirin on long-term cancer incidence and metastasis: a systematic comparison of evidence from observational studies versus randomised trials. Lancet Oncol, 2012; 13(5): 518-527.
- Macdonald S. Aspirin use to be banned in under 16 year olds. BMJ, 2002; 325(7371): 988.
- Schrör K. Aspirin and Reye syndrome: a review of the evidence. Paediatr Drugs, 2007; 9(3): 195-204.
- Pugliese A, Beltramo T, Torre D. Reye’s and Reye’s-like syndromes. Cell Biochem Funct, 2008; 26(7): 741-746.
- Hurwitz ES. Reye’s syndrome. Epidemiol Rev, 1989; 11: 249-253.
- Meremikwu MM, Okomo U. Sickle cell disease. BMJ Clin Evid, 2011; 2011: 2402.

