Attitudes toward Stimulant Medication for Treating ADHD among Physical Education Student Teachers
Sharon Tsuk1,*, Sima Zach1, Omer Glixman1, Arie Rotstein1, Einat Avieli1, and Aviva Mimouni-Bloch2,3
1The Levinsky - Wingate Academic center, Netanya, Israel
2The Pediatric Neurology and Developmental Unit, Loewenstein Rehabilitation Medical Center, Raanana, Israel
3Sackler Faculty of Medicine, Tel-Aviv University, Tel-Aviv, Israel
Received Date: 06/03/2023; Published Date: 18/05/2023
*Corresponding author: Sharon Tsuk, The Academic College at Wingate, Wingate Institute 4290200, Israel
Abstract
The aim of the study was to evaluate the health behaviors and attitudes of Physical Education Student Teachers (PEST) compared to those of student teachers of other subjects (GEST). 652 Education students completed the questionnaire. Compared to GET students, fewer PEST (5.4% vs 9.1%) reported smoking tobacco, while more reported using marijuana or alcohol (6.1% vs 3.3% and 7.6% vs 4.8%, respectively). No differences were found regarding the use of prescribed stimulant medication for ADHD. However, more PEST reported currently using non-prescribed stimulant medication for treating ADHD (14.7% vs 2.7%), and more often not taking their prescribed medication (94.1% vs 78.4%). Furthermore, PEST were more against encouraging their future students with ADHD to comply with stimulant treatment. These results raise concerns regarding the health behaviors and attitudes of future physical education teachers, and the implications on children who have been diagnosed with ADHD.
Keywords: Methylphenidate; Misuse; Substances; Cigarettes; Alcohol
Introduction
Current professional guidelines consider methylphenidate and amphetamine medications to be main stimulant medication for treating Attention Deficit Hyperactivity Disorder (ADHD) [1]. Such medication has been found to improve core symptoms of ADHD (i.e., hyperactivity, impulsivity, and inattention), as well as associated functional impairments in ADHD patients [2]. However, the public’s perceptions of pharmacological treatment for ADHD is controversial [3,4] with negative attitudes possibly having a negative effect on adolescents’ adherence to treatment. Moreover, adolescents may also be influenced by others’ beliefs regarding the necessity of the medications [5].
As ADHD is a chronic condition, successful treatment for most individuals requires the ongoing adherence to therapy [6]. Indeed, a lack of adherence to pharmacological treatment may increase the risk of a wide range of ADHD-associated negative functional outcomes [7]. For example, both child and family characteristics may play a role in adherence to methylphenidate treatment [8]. Research also indicates that children of mothers with only one child or children of mothers with an average household income (compared to a high income) were more likely to be adherent to treatment, while children who began treatment aged 12 years or older (compared to younger than 12 years) and girls were more often not persistent in treatment.
Teachers play a key role in the diagnosis, referral, implementation, and treatment of children with ADHD, and are highly influential in children’s adherence to such treatment. For example, the beliefs, attitudes, and efficacy of school teachers are important factors in the improving of students’ health literacy [9]. However, despite more than 10% of their students being prescribed with such medications, teachers report having limited knowledge of psychotropic treatment. They also had little communication with parents or professionals regarding the use of such medication or their side effects [10]. As the number of school children and adolescents treated with stimulant medication for treating ADHD is substantial and growing [11], it is important for teachers to possess research-based knowledge, rather than mistaken perceptions or attitudes, regarding stimulant medication for treating ADHD.
Specifically, Physical Education (PE) teachers are an important group that should be addressed in this regard, as health promotion aspects are at the essence of their profession [12]. Physical Education Student Teachers (PEST) are trained to serve as role models regarding healthy behaviors, and as such, should promote a healthy life style within their schools [13]. During their academic studies, PEST practice physical activity (PA) and sports as part of their curriculum. In addition, most also practice more PA as a built-in component of their personal and professional lives [14]. However, PEST may be more susceptible to negative body images, eating disorders, and exercise disorders than their same-aged peers who are involved in careers that are not related to food, health education, or exercise [15]. People who exercise excessively are prone to risky behaviors, such as exercise disorders, using steroids, body image concerns, and eating problems [16,17]. In turn, these higher health risks may raise the likelihood of inappropriate and precarious behaviors among PEST being conveyed to their school students in the future [15]. It should, however, be noted that data relating to other risk factors among PEST, such as alcohol consumption and tobacco use, are scarce.
Prescription stimulants for treating ADHD are a class of medications that has a high abuse potential, particularly among college students who mainly use them to enhance academic achievements [18-20]. College students who used non-prescribed stimulants reported continuing to do so even after graduating [21]. While the effects of stimulants on academic performance in non-ADHD college students are unclear, serious adverse health effects have been indicated [22]. For example, college students who were involved in the misuse of stimulant medication, the use of un-prescribed stimulants, or the transferring of stimulant medication to others may underestimate associated risks while overestimating benefits [23].
Discrepancies exist between medical recommendations for people with ADHD and certain public perceptions regarding the effectiveness of such treatment. As such, it would be of value to examine these attitudes among PEST, and compare them to general education student teachers (GEST), who are not necessarily trained to actively promote healthy lifestyle behaviors. In this study, we hypothesize that as PEST participate in a large number of academic courses on human physiology, physical activity, and health consequences, they will show more positive health behaviors and attitudes compared to GEST students. Thus, the aim of this study was to compare health behaviors and attitudes regarding ADHD treatments among PEST to GEST, including adherence to stimulant medication for treating ADHD.
Methodology
Participants
A Web-based questionnaire was distributed via E-mail and social media to 4,000 education student teachers from four different colleges in Israel. After positively responding to the first question on the questionnaire, which asked for the person’s approval to take part in the survey, 652 respondents completed the questionnaire: 438 PEST and 214 GEST respondents.
Questionnaire
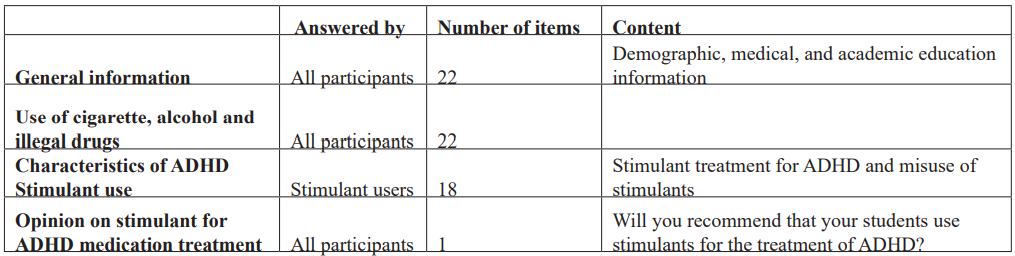
The questionnaire was designed by two experts in the field of ADHD and was evaluated by two other experts, as a means for assessing the use and misuse of prescription stimulants and other harmful substances (Table 1). The questionnaire, which also screened students’ health habits, included 41 items regarding general information, use of stimulant medication for treating ADHD, and attitudes towards such medication. The Institutional Review Board of the authors’ affiliated academic institution (#123) approved the study.
First, all participants were asked to answer the first 22 items, which included information relating to demographics, medical background, and academic education. The participants were also asked about their consumption of specific substances (including for treating ADHD) on a regular basis (from a given list or from their own additions). Some substances are illegal in Israel (such as marijuana and psychoactive drugs) or are considered harmful (such as alcohol, tobacco, and cigarettes).
Next, those who stated that they use at least one stimulant medication for treating ADHD were asked to respond to 18 additional items regarding stimulant use and misuse. For example, “Which stimulants do you use? Were you administered the stimulant through a doctor’s prescription? Have there been occasions when you chose not to take your prescribed medication? Have you been formally diagnosed with ADHD? Does your stimulant treatment affect the way you feel? Do you feel that the stimulant affects your physical performance during physical activity?”
Finally, all participants were asked to express their attitudes towards stimulant therapy, via the following question: "In the future, if you are a teacher, will you recommend that your students use stimulant medication for treating their ADHD?"
Table 1: Questionnaire structure.
Statistical Analysis
Analyses were carried out using SPSS Statistics for Windows (2017) version 25.0 (IBM Corp, Armonk, NY, USA). As most variables were a-parametric, significant differences between PEST and GET students were determined by chi-square tests. Numerical characteristic variables were analyzed through t-tests.
Results
The PEST group included significantly more male students than the GET group, 43.4% vs 11.7%, respectively. Furthermore, more students in the PEST group reported participating in PA, not having chronic diseases, and not regularly administering medication. No differences were found between the groups regarding their age or body mass index (BMI) (Table 2).
Table 2: Social and demographic subjects' characteristics.

PEST – physical education student teachers; GET – general education teacher students. * p ≤ .05; ** p ≤ .001, significant difference between GET and PEST
a such as Crohn disease, anemia, asthma, hypothyroidism, etc.
b such as ADHD stimulants and other medications such as thyroid hormones, contraceptives, insulin, iron supplements, SSRIs, and cardiac medications.
As seen in Table 3, the prevalence of alcohol, cigarettes, and marijuana consumption differed significantly between the two groups, whereby more students from the PEST reported that they do not use any harmful substances whatsoever (not including prescribed medication), and fewer reported smoking cigarettes or drinking alcohol. Interestingly, less PEST reported regular use of pain killing drugs. Seven students reported using illegal stimulating drugs (not for ADHD), three from the PEST and four from the GET group.
Table 3: Differences of Prevalence of Substance Use among PEST and GET students. The only reported substances used were Marijuana. Alcohol Cigarettes and Pain medications.
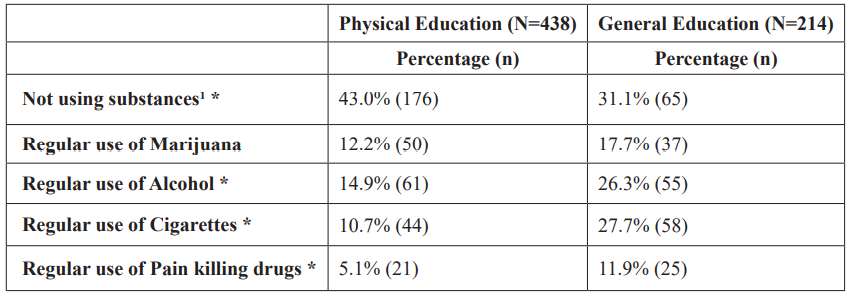
1not using alcohol, cigarettes, any legal or illegal drugs or medications, * p ≤ .05
Analysis of the participants’ behavior regarding the use of stimulant medication for treating ADHD showed that 15.3% of the PEST participants and 17.3% of the GET respondents were using these medications at the time of the study (Table 2). In both groups, immediate-release methylphenidate was the most frequently used (PEST: 11.0%; GEST, 8.9%), while the second most frequently used stimulant was the extended-release methylphenidate. More PEST participants reported to be currently using non-prescribed ADHD stimulants than GEST ones (14.7% vs 2.7%).
When analyzing the students who were currently using prescribed stimulants for treating ADHD in the two groups, the PEST group included more male participants, lower BMI, higher reported PA, and less reports of chronic diseases, use of other medications, alcohol consumption, or cigarette smoking. The PEST group also reported having used prescribed medication for a shorter period, most only having started ADHD treatment in the previous year – compared to GEST participants; however, no differences were seen in the frequency of their using the ADHD treatment (Table 4). More participants in the PEST group reported that they occasionally choose not to use stimulants, partly as it interferes with their PA. As in the PEST group as a whole, the subgroup of stimulant users within the PEST group reported participating more often in PA, less chronic diseases (not including ADHD), less medications (other than stimulants for ADHD), and less alcohol consumption and cigarette smoking (Table 4).
Table 4: Characteristics of subjects using prescribed ADHD stimulants presented as percentage (number).

PEST – Physical Education Student Teachers; GET – General Education Teacher Students. * p ≤ .05; ** p ≤ .001, significant difference between GET and PEST
The final question that the students were asked was, "In the future, if you are a teacher, will you recommend that your students use stimulants for treating ADHD?" Significant differences were seen between the two groups (Table 5), whereby PEST respondents were more decisive against using stimulants (e.g., "I will recommend that the pupil does not use such stimulants "; "I will only recommend using such medications as the last resort "; or "I will recommend that the pupil uses the medication as infrequently as possible”). GEST students were less decisive regarding their objection to their future pupils using stimulants, answering that their recommendations concerning ADHD treatment would depend on several variables, such as the child’s symptoms and social status. Relatively few students in both groups answered that they would refer the pupil to a professional or that they would adhere to a professional's recommendation. In the subgroup of current stimulant users, about 27.6% of the PEST and 19.4% of the GEST respondent stated that they would not recommend the use of such medications among children.
Table 5: Attitudes of Education Students toward Use of ADHD Treatment of their Future Students.
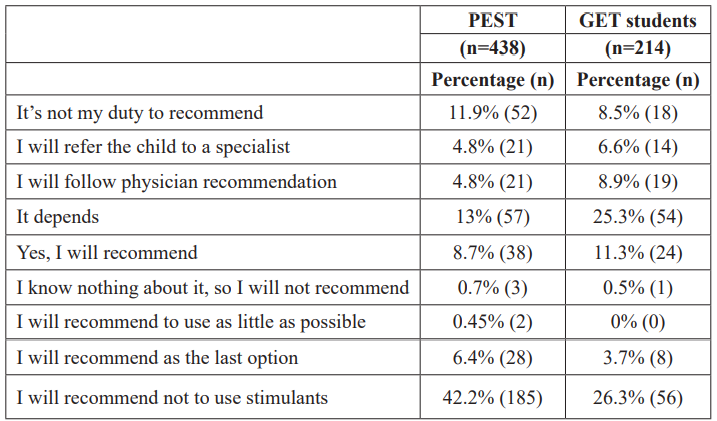
Answers to the question: Will you recommend stimulants for your future students?
Significant differences were found between the answers of PEST compared to that of GET students, p ≤ .001
Discussion
The aim of the present study was to evaluate the health behaviors and attitudes of future teachers regarding stimulant medication for treating ADHD among children. Our findings indicate that in line with their expected role as health promoters, PEST respondents tend to engage in PA, do not smoke, and do not consume alcohol, compared to GEST respondents. These findings are in line with previous studies, whereby PEST respondents tend to consume less alcohol and cigarettes than other college students [24,25]. Indeed, researchers state that differences in smoking and alcohol usage might be the result of the students’ major academic field of studies [26] or living location [27]. In addition, fewer PEST respondents reported having chronic diseases or using medications other than ADHD-related stimulant. These differences between the two groups may stem from the healthier lifestyles and behaviors, as well as their predisposed characteristics of young adults who choose to embark on a physical education career.
An additional aspect of health promotion that was evaluated in the study relates to the behaviors and attitudes of future teachers regarding stimulant medication for treating ADHD. Although the prevalence of their own personal use of such medication was similar between the two groups, more students from the PEST group stated that they sometimes choose to refrain from using these stimulants (even though they have been prescribed) and reported using non-prescribed stimulants. The prevalence of stimulants use for ADHD treatment among both groups of participants in the present study is similar to that reported for college students in other fields of study [28]. However, in the present study, the prevalence of students who had been diagnosed with ADHD and who reported using non-prescribed stimulant medications is higher than those reported among other students [29], and is significantly higher among the PEST group than in the GEST group (Table 3). The findings in the present study imply somewhat undisciplined behavior of future teachers of PE regarding stimulant treatment for ADHD, which may indicate a lack of respect for professional opinions or alternatively, suggest that they possess increased self-sufficiency, where they believe they are capable of reaching their own decisions. A lack of respect for professional opinions can also be seen in the respondents’ answer to the question, "In the future, if you are a teacher, will you recommend that your students use stimulant medication for treating their ADHD?" Disturbingly, more than half the PEST participants answered that they would not recommend using stimulants for ADHD treatment of their future students, and very few reported that they would follow a doctor’s recommendations concerning ADHD treatment for their pupil, compared to GET students. Although teachers have limited knowledge on the topic of ADHD (Lien et al., 2007), the findings of this study suggest that future teachers believe that they are capable of offering advice and even making medication-related decisions for their future pupils.
Practical application
We believe that it is crucial to educate PEST about ADHD and its treatment through stimulant medication, and about the influence that they will have as teachers on their pupil’s compliance with medical treatment regarding ADHD.
Conclusion
PEST respondents were found to be more decisive against using stimulants, with more of them stating that they would not recommend stimulant treatment for their future students who are diagnosed with ADHD. This negative attitude among PEST respondents regarding stimulant treatment for children is highly concerning, as they are soon to be in a position where they can influence their future pupil’s adherence to ADHD treatment.
Conflict of Interests: Authors declare no conflicts of interest, and no funding resource to declare.
References
- First MB. DSM-5® Handbook of Differential Diagnosis. 5th edn, DSM-5® Handbook of Differential Diagnosis. 5th edn. American Psychiatric Publishing, 2013.
- Huss M, Duhan P, Gandhi P, Chen CW, Spannhuth C, Kumar V. ‘Methylphenidate dose optimization for ADHD treatment: review of safety, efficacy, and clinical necessity’, Neuropsychiatric disease and treatment, 2017; 13: pp. 1741–1751.
- Jensen PS. ‘Current concepts and controversies in the diagnosis and treatment of attention deficit hyperactivity disorder’, Current psychiatry reports, 2000; 2(2): pp. 102–109.
- Rowland AS, Lesesne CA, Abramowitz AJ. ‘The epidemiology of attention-deficit/hyperactivity disorder (ADHD): a public health view’, Mental retardation and developmental disabilities research reviews, 2002; 8(3): pp. 162–170.
- Emilsson M, Gustafsson PA, Öhnström G, Marteinsdottir I. ‘Beliefs regarding medication and side effects influence treatment adherence in adolescents with attention deficit hyperactivity disorder’, European child & adolescent psychiatry, 2017; 26(5): pp. 559–571.
- Wolraich ML, Chan E, Froehlich T, Lynch RL, Bax A, Redwine ST, et al. ‘ADHD diagnosis and treatment guidelines: A historical perspective’, Pediatrics, 2019; 144(4).
- Boland H, DiSalvo M, Fried R, Woodworth KY, Wilens T, Faraone SV, et al. ‘A literature review and meta-analysis on the effects of ADHD medications on functional outcomes’, Journal of Psychiatric Research, 2020; 123: pp. 21–30.
- Cheung K, DIerckx B, El Marroun H, Hillegers MHJ, Stricker BH, Visser LE. ‘Methylphenidate Treatment Adherence and Persistence in Children in the Netherlands’, Journal of child and adolescent psychopharmacology, 2021; 31(3): pp. 205–213.
- Lai HR, Wu DM, Lee PH, Jhang YS. ‘Health Literacy Teaching Beliefs, Attitudes, Efficacy, and Intentions of Middle School Health and Physical Education Teachers’, The Journal of school health, 2018; 88(5): pp. 350–358.
- Lien MT, Carlson JS, Hunter-Oehmke S, Knapp KA. ‘A pilot investigation of teachers’ perceptions of psychotropic drug use in schools’, Journal of attention disorders, 2007; 11(2): pp. 172–177.
- Thomas R, Sanders S, Doust J, Beller E, Glasziou P. ‘Prevalence of Attention-Deficit/Hyperactivity Disorder: A Systematic Review and Meta-analysis’, Pediatrics, 2015; 135(4): pp. e994–e1001.
- Sallis JF, McKenzie TL, Beets MW, Beighle A, Erwin H, Lee S. ‘Physical education’s role in public health: steps forward and backward over 20 years and HOPE for the future’, Research quarterly for exercise and sport, 2012; 83(2): pp. 125–135.
- Webster CA, Webster L, Russ L, Molina S, Lee H, Cribbs J. ‘A systematic review of public health-aligned recommendations for preparing physical education teacher candidates’, Research quarterly for exercise and sport, 2015; 86(1): pp. 30–39.
- Hills AP, Dengel DR, Lubans DR. ‘Supporting public health priorities: recommendations for physical education and physical activity promotion in schools’, Progress in cardiovascular diseases, 2015; 57(4): pp. 368–374.
- Yager Z, O’Dea J. ‘Body image, dieting and disordered eating and activity practices among teacher trainees: implications for school-based health education and obesity prevention programs’, Health education research, 2009; 24(3): pp. 472–482.
- O’Brien KS, Hunter JA. ‘Body esteem and eating behaviours in female physical education students’, Eating and weight disorders: EWD, 2006; 11(2).
- Olson MS, Esco MR, Williford H. ‘Body Image Concerns in College-Aged Male Physical Education Students: A Descriptive Inquiry.’, Physical Educator, 2009; 66(1): pp. 45–54.
- Bavarian N, Flay BR, Ketcham PL, Smit E. ‘Illicit Use of Prescription Stimulants in a College Student Sample: A Theory-Guided Analysis’, Drug and alcohol dependence, 2013; 132(3): p. 665.
- Looby A, De Young KP, Earleywine M. ‘Challenging expectancies to prevent nonmedical prescription stimulant use: a randomized, controlled trial’, Drug and alcohol dependence, 2013; 132(1–2): pp. 362–368.
- Benson K, Flory K, Humphreys KL, Lee SS. ‘Misuse of stimulant medication among college students: a comprehensive review and meta-analysis’, Clinical child and family psychology review, 2015; 18(1): pp. 50–76.
- Holt LJ, McCarthy MD. ‘Predictors of Prescription Stimulant Misuse in U.S. College Graduates’, Substance use & misuse, 2020; 55(4): pp. 644–657.
- Faraone SV, Rostain AL, Montano CB, Mason O, Antshel KM, Newcorn JH. ‘Systematic Review: Nonmedical Use of Prescription Stimulants: Risk Factors, Outcomes, and Risk Reduction Strategies’, Journal of the American Academy of Child and Adolescent Psychiatry, 2020; 59(1): pp. 100–112.
- Kinman BA, Armstrong KJ, Hood KB. ‘Perceptions of Risks and Benefits Among Nonprescription Stimulant Consumers, Diverters, and Non-Users’, Substance use & misuse, 2017; 52(10): pp. 1256–1265.
- Bogati S, Singh T, Paudel S, Adhikari B, Baral D. ‘Association of the Pattern and Quality of Sleep with Consumption of Stimulant Beverages, Cigarette and Alcohol among Medical Students’, Journal of Nepal Health Research Council, 2020; 18(3): pp. 379–385.
- Sharareh P, Leili T, Abbas M, Jalal P, Ali G. ‘Determining correlates of the average number of cigarettes smoking among college students using count regression models’, Scientific reports, 2020; 10(1).
- Chen WL, Chen JH. ‘“College fields of study and substance use”’, BMC public health, 2020; 20(1).
- Firth C, LaBrie JW, D’Amico EJ, Klein DJ, Griffin BA, Pedersen ER. ‘Changes in Cigarette, E-Cigarette, and Cannabis Use among U.S. College Students Studying Abroad’, Substance use & misuse, 2020; 55(10): pp. 1683–1691.
- Advokat C, Lane SM, Luo C. ‘College students with and without ADHD: comparison of self-report of medication usage, study habits, and academic achievement’, Journal of attention disorders, 2011; 15(8): pp. 656–666.
- Green AL, Rabiner DL. ‘What do we really know about ADHD in college students?’, Neurotherapeutics: the journal of the American Society for Experimental NeuroTherapeutics, 2012; 9(3), pp. 559–568.

